In what cases is the procedure performed?
If a person has difficulty blinking, is experiencing constant pain, and the drops do not have an effect, the ophthalmologist usually prescribes an injection into the eye. Such injections are made only by specialists; you should not administer the medicine yourself, as you can harm the organ even more. This procedure is performed with a very thin needle. The drug itself, the duration of the course and the number of injections are determined by the doctor, based on the specifics of the disease.
Ophthalmologists agree that intravitreal injection is an extremely effective way to treat eye diseases. This procedure helps well in stopping inflammatory processes, which, in turn, are of several types:
- uveitis;
- iridocyclitis;
- conjunctivitis.
In addition to inflammation, injections into the eye are prescribed for:
- mechanical damage to the organ;
- identifying blood clots in the retinal venous plexuses;
- macular degeneration, usually occurs in old age;
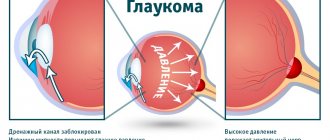
- retinal detachment, glaucoma and similar pathologies;
- astigmatism, atrophy, blepharitis;
- autoimmune pathologies (endocrine-type ophthalmopathy, rheumatoid arthritis, ankylosing spondylitis).
Types of injections
Experts distinguish several types of injections into the eyeball and classify them depending on how exactly the drug is administered.
- Retrobulbar injection. A characteristic feature of this type of injection is the fairly deep insertion of the needle - about three centimeters into the marginal area of the orbit. It is performed through the skin of the lower eyelid, parallel to the wall of the orbit of the eye. In this case, the drug enters the eyeball unhindered.
- Subconjunctival injection. This method involves inserting a needle exactly under the conjunctiva in the lower eyelid area. The procedure is extremely painful and unpleasant; the injection is given only after the doctor instills pain-relieving drops. The manipulation is performed not once, but three times with an interval of one minute. For this type of injection, the doctor uses an insulin syringe.
- Intravitreal injection. It is characterized by the introduction of medicine directly through the vitreous body with a very thin needle. Before starting the procedure, local anesthesia is performed.
- Parabulbar injection. The parabulbar space is the fiber tissue that is located between the periosteum and the eyeball. The injection is made through the lower eyelid, the needle passes parallel to the lower wall of the orbit.
Contraindications
Contraindications depend on the type of drug and individual sensitivity to it.
It is not recommended to try to give injections at home or trust your health to friends, relatives and other people who do not understand anything about ophthalmology. The procedure can only be performed by a doctor or nurse.
Injections in the eyes are generally not recommended:
- pregnant women;
- breastfeeding;
- minors;
- those who have problems with the kidneys and liver.
But each case is individual, and the decision is made by the attending physician based on therapeutic goals.
Types of eye injections
Injections into the eyeball differ in the method of administration:
Retrobulbar injection. This method of performing the procedure is characterized by deep insertion of a needle into the edge of the orbit (3-3.5 cm) through the skin of the lower eyelid parallel to the orbital wall, and the medicine gets behind the eyeball.- Subconjunctival (subconjunctival) injection. The needle penetrates exactly under the conjunctiva through the lower eyelid. The procedure is painful, an injection into the eyeball is performed only after preliminary anesthesia (dicaine, novocaine), anesthesia is carried out three times with a difference of 1 minute. For subconjunctival injection, an insulin syringe is used, the direction is with a cut towards the surface of the eye.
- Intravitreal injection. Injection of the drug directly into the vitreous body. It is carried out after anesthesia with drip anesthesia and a thin injection needle. A 2-3 mm puncture is made 4 mm from the limbus, with the needle perpendicular to the sclera.
- Parabulbar injection. The parabulous space is the fiber tissue located between the periosteum and the eyeball. The injection is carried out through the lower eyelid, the needle passes parallel to the lower wall of the orbit. The second method of injection: the needle enters 2-3 mm at an angle of 25 ° with a cut directed towards the eyeball into the sub-Tenon's space (the space between the sclera and the fascial sheath with fluid).
Injections of drugs into the eyeball can only be performed by an experienced ophthalmologist under sterile conditions using disposable instruments. Before making an injection into the eye, a pain relief procedure is performed with Dicaine or Novocaine in the form of eye drops. After 5 minutes you can begin the procedure. If the procedure is performed using a subconjunctival, retrobulbar or parabulbar method, it is necessary to treat the needle insertion area with 70% ethyl alcohol. After the procedure, press a cotton swab with an antibacterial solution for several minutes.
Preparations for injections into the eyes
Each type of disease requires treatment with the appropriate drug. It is prescribed by a doctor after a thorough examination and review of the patient’s medical record to identify individual characteristics.
Medicines for the eyes are divided into:
- antibiotics;
- vitamin complexes;
- hormonal;
- enzymatic.
One of the popular drugs is the Eylea solution, which is produced in Italy. It is actively used to treat diseases of the organs of vision. But, besides this, there are several more effective remedies that have proven themselves and are actively used by ophthalmologists.
Antiangiogenic therapy using Avastin and Lucentis
To prevent the formation of new microvessels from existing capillaries, antiangiogenic therapy is carried out, during which Avastin is often used. This drug belongs to the class of antitumor drugs. It blocks proliferation processes and helps stop the growth of fresh blood vessels. In addition, it perfectly fights the causes of the disease. Often this phenomenon is caused by pathologies such as the wet form of macular degeneration in older people, diabetic retinopathy, and so on.
The main active chemical in Avastin is bevacizumab. It is this substance that, when penetrating the protein, helps stop tissue proliferation and blocks the growth of a tumor, if there is one.
The ophthalmologist injects the drug into the vitreous body, the direction of play is towards the central sections. The dose is 1.25 mg. The composition must be administered once a month. The course consists of several injections. More than 60% of patients note stabilization of vision after treatment.
An analogue of this drug is the no less famous “Lucentis”. It has the same functions and action. The only difference between the two drugs is that the active chemical in Avastin is bevacizumab, while in Lucentis it is ranibizumab. But both drugs have the same effect on the body, indications and contraindications, which include pregnancy, breastfeeding and problems with the kidneys and liver.
Both drugs are rated as effective and consistently show excellent results. But numbers speak better than words. Statistics on the use of these drugs show that 92% of patients treated with Avastin or Lucentis retained their vision. And in 70% of patients it even worsened after taking Lucentis. Those treated with Avastin performed even better – vision improved by an average of 1.9 letters.
"Pheebs"
This medicine is created on the basis of biogenic stimulants. Thanks to this, “Phibs” increases the speed of regeneration and improves metabolic processes. It is used in the treatment of various diseases:
- inflammatory processes in the cornea and at the edges of the eyelids;
- different types of conjunctivitis;
- diseases causing vision loss;
- vitreous opacification.
The active chemicals in this drug are extracts of estuary mud, cinnamic acid and coumarin.
Contraindications to the use of "Phibs":
- problems with the heart and blood vessels;
- diseases of the gastrointestinal tract;
- pregnancy;
- lactation period;
- kidney problems.
The course of treatment usually lasts for a month or a little longer. The specialist administers the drug once a day. A repetition of the course, if necessary, can be scheduled only two months after the first.
"Ozurdex"
The drug is in the form of an implant. It contains the hormone dexamethasone and other excipients: a copolymer of lactic and glycolic acid.
Dexamethasone is a potent corticosteroid, therefore it is extremely effective in combating inflammatory processes, has an anti-edematous effect, prevents the growth of new blood vessels, thickens the walls of capillaries and the activity of fibroblasts. In addition, this substance shows excellent results in the fight against retinal vein occlusion and helps restore blood circulation in the capillaries.
The statistics of treatment with this drug are convincing: in most patients, the thickness of the retina decreased by two or more times, which brought it closer to normal, and visual acuity increased from 5% to 65%.
But such an effective medicine has its contraindications:
- individual intolerance;
- trachoma;
- glaucoma;
- various types of infections - from bacterial to viral.
"Reaferon EU"
This is an immunomodulatory drug that effectively fights tumors and viruses. Stops the reproduction of viruses in infected cells. Used in treatment if the patient:
- conjunctivitis;
- uevitis;
- inflammation of the outer membrane and cornea of the eye.
The main active substance is interferon alpha 2a, which contains 165 amino acids.
The course usually consists of 15-20 injections, but the final decision on the treatment regimen is made by the attending physician. Injections are given daily.
It is not recommended for use by people who have:
- kidney and liver problems;
- heart diseases;
- pregnancy and lactation;
- mental disorders.
The drug is also contraindicated in people who are already taking immunosuppressive medications.
"Emoxipin"
This drug has a potent effect. Shows excellent results in the treatment of:
- cataracts;
- pathologies of the vascular system of the eyes;
- oxygen starvation;
- glaucoma;
- keratitis;
- damage to the cornea of the eye.
The main active chemical substance is methylethylpyridinol hydrochloride, thanks to which “Emoxipin” exhibits the properties of an antioxidant, antihypoxant, vasoconstrictor and antiplatelet agent. This means that the medicine reduces the number of free radicals that have a bad effect on the body, increases resistance to oxygen deficiency, makes blood vessels stronger and less permeable, and prevents the formation of blood clots.
The specialist administers this drug under the conjunctiva, retrobulbar or parabulbar.
Contraindicated in people who are already taking other medications, have an individual intolerance to the drug, or are pregnant or breastfeeding.
Conjunctival injection
Conjunctivitis is accompanied, first of all, by varying degrees of hyperemia of the tarsal conjunctiva (conjunctiva of the eyelids). Also, there is redness of the transitional fold, the conjunctiva of the eyeball. In the case of chronic conjunctivitis, hyperemia of the conjunctival cartilage is usually observed. In acute inflammation, hyperemia of the conjunctiva of the eye and the conjunctiva of the cartilage is observed.
A distinctive feature of conjunctival hyperemia is that the redness of the conjunctiva of the eyeball is especially intense near the transitional fold. It becomes distinctly red (i.e., not purple or bluish), and it becomes possible to see individual vessels or move them together with the conjunctiva. Undoubtedly, this is not the only symptom of conjunctivitis; the formation of discharge, swelling, foreign body sensation and photophobia are also present. With a particularly pronounced conjunctival injection, a ciliary injection may join it, causing a mixed type of redness.
Preparation and carrying out the procedure
When preparing and performing injection manipulation, it is important to follow the following rules.
- Before the procedure, the eyeball is thoroughly anesthetized, usually with novocaine or dicaine in the form of eye drops. After five minutes, you can begin to administer the drug.
- Intravitreal injections into the eye are performed only by an experienced ophthalmologist using disposable instruments.
- When performing the procedure using subconjunctival, retrobulbar or parabulbar methods, it is necessary to treat the area where the needle will be inserted with a 70% solution of ethyl alcohol.
- After the procedure is completed, the patient needs to press a cotton swab soaked in an antibacterial solution for several minutes.
How to give an injection
The order of the injection procedure depends on how exactly the drug will be administered. But, in any case, all this will happen in strictly sterile conditions on an outpatient basis.
The doctor dilates the pupil with special drops; they begin to act after 20-30 minutes.
Visual acuity will remain reduced for another 12 hours after the end of the procedure.
The needle is inserted either into the edge of the orbit, or with a cut towards the eyeball, or near the limbus, or into the sub-Tenon's space. It all depends on the disease and the purpose of the injection. This is decided only by the attending physician.
How to give an injection in the eye and what drugs are used
Almost every person, faced with the need for such a medical procedure as an injection into the eyeball, experiences shock and fear.
However, most ophthalmologists prefer this method when treating serious eye pathologies.
It helps transport the medicine directly to the affected area of the eye, which significantly increases the chances of a speedy recovery.
Since the injection is done under local anesthesia, the patient does not feel any discomfort, but the benefits from such a procedure, which is scary at first glance, are enormous.
When do you need an eye injection?
The most common and well-known method for treating ophthalmic pathologies is eye drops. In what cases are eye injections prescribed? They are done if it is necessary to deliver the drug to the deeper structures of the organs of vision. Thus, intraocular injections are indicated for:
- inflammatory processes - keratitis, uveitis, iridocyclitis, scleritis, neuroretinitis;
- formation of a blood clot in the retinal vein;
- the formation of edema in the macula in patients with diabetes;
- development of age-related macular degeneration;
- eye injury;
- myopia;
- the presence of autoimmune pathologies affecting the organs of vision - rheumatoid arthritis, endocrine ophthalmopathy, ankylosing spondylitis.
An injection may be required in the postoperative period if the patient has developed glaucoma or retinal detachment.
Types of injections
There are two main types of eye injections:
- Periocular - the medication is administered through a puncture of the skin of the lower eyelid.
- Subconjunctival - the puncture is performed directly into the mucous membrane of the eye. Such injections are more painful compared to periocular ones.
Depending on the type of pathology that has arisen, injections can be performed in different areas of the visual organ. The following types of intraocular injections are distinguished:
- Subconjunctival - carried out both for the treatment and diagnosis of certain diseases. Sometimes subconjunctival injections are given during surgery. This type of intraocular injection is contraindicated in the presence of acute infection in the conjunctival cavity. The injection itself is made at the base of the fold of the conjunctiva, with the needle located parallel to the sclera. The puncture depth is 2–4 mm.
- Parabulbar - both subconjunctival and parabulbar injections are done in cases where an ophthalmological disease threatens complete loss of vision. The injection is made into the lower wall of the orbit (lower eyelid), located in the area under the eyeball. During the procedure, the needle is positioned strictly parallel to the orbital wall. The parabulbar space is fiber tissue located between the eyeball and the periosteum. The puncture depth is 1–2 cm. A contraindication to such manipulation may be an infectious or allergic process in the organ of vision. A parabulbar injection can also be performed in another way - into the sub-Tenon's space. With this method, the puncture depth is 2–3 mm, and the needle is inserted at an angle of 25 ͦ. The cut of the needle is directed towards the eyeball.
- Retrobulbar - the needle is inserted deep into the edge of the orbit (3–3.5 cm). The puncture is performed in the lower eyelid, parallel to the orbital wall. The bevel of the needle is directed towards the eyeball.
- Intravitreal - the injection is performed directly into the vitreous body. Before the procedure, anesthetic drops must be injected into the eyes. Intravitreal injections, like any type of intraocular injections, are made with a very thin needle. It is inserted at a distance of 4 mm from the limbus, to a depth of 2–3 mm. During the procedure, the needle must be positioned strictly perpendicular to the sclera.
- Intra-arterial - with this method, the medicine is injected directly into the bloodstream. To do this, the doctor punctures the arterial vessel of the eye and injects the required dose of the drug. This method is used to create a high concentration of the drug in a certain area of the eye. The method under consideration can also be used for diagnostic purposes: an X-ray preparation is injected into the ophthalmic artery, which makes it possible to determine the exact location of the pathological formation (for example, a blood clot, narrowing of a vessel, tumor or aneurysm).
- Subchoroidal - the injection is performed into the uveoscleral system, through which tear fluid drains from the eyes.
What drugs are used
The following drugs are used in the treatment of eye diseases:
- Reaferon – has immunomodulatory, antitumor and antiviral properties. The solution effectively eliminates inflammation of the outer shell of the eyes that is of viral origin, improves the condition of the eyes in case of hepatitis, herpes, and cancerous tumors. Reaferon cannot be used together with certain types of antibiotics and glucocorticoids.
- Retinalamine - restores retinal tissue without causing adverse reactions. The medicine is used for diseases such as open-angle glaucoma, diabetic retinopathy, myopia, retinal dystrophy, etc. The drug is contraindicated in patients under 18 years of age.
- Ozurdex - contains dexamethasone, which has a pronounced anti-inflammatory effect. The medication helps reduce macular edema resulting from vein thrombosis or inflammation in the eyes. Ozurdex is also sometimes used for macular edema caused by diabetes. The drug may cause adverse reactions, manifested in the form of increased IOP and the formation of cataracts. This medicinal solution should not be prescribed to pregnant women and patients suffering from glaucoma, herpetic eye lesions, or lack of a lens. The main advantage of injections using Ozurdex is its high efficiency in the fight against thrombosis of the ocular vessels.
- Eylea - helps slow down the process of vascular formations and reduce macular edema. The active component on the basis of which this medication is developed is the recombinant protein aflibercept. Contraindications to its use are: ocular and periocular infections, active inflammatory processes in the deep tissues of the eyes, hypersensitivity. The drug is highly effective, but can provoke an increase in IOP.
- Lucentis - a medicinal solution based on a substance that prevents the growth of vascular endothelium - cells located on the inner surface of blood vessels. This helps reduce the pathological growth of new vessels and eliminate macular edema. Injections using Lucentis are contraindicated for pregnant and nursing mothers, patients under 18 years of age, allergy sufferers, and those with infectious processes in the orbital area. The advantage of the drug is the extremely rare development of side effects.
The cost of intravitreal injections, and where you can undergo the procedure
The procedure can be carried out after a thorough examination by a specialist and diagnosis of the disease at an ophthalmology center. To establish a diagnosis, you will have to undergo several tests, which will be prescribed by an experienced doctor.
The procedure described is not cheap. The injection itself costs 200-300 rubles, excluding the price of the drug. And with it, the amounts range from 10,000 to 70,000 rubles. It all depends on the medical center, the qualifications of the doctor and the drug itself.
But health is always worth its money, you just need to trust the professionals, because our eyes help us see this wonderful world, our loved ones, do important things and just enjoy. They are the most important sensory organ that requires timely treatment and care.