Causes
The main cause of the disease is the spread of bacterial infection. It can enter the eyes in the following cases:
- touching the eyes and the area around them with dirty hands or other objects;
- infectious diseases of the ENT organs and oral cavity that spread to neighboring tissues;
- disturbance of the microflora in the eye area, when any negative factor causes the proliferation of streptococcal and staphylococcal microflora;
- pathology of the lacrimal sac, as a result of which bacteria accumulate inside it;
- contact with a foreign object in the eyes, for example, in a strong wind, particles of dust and dirt can spread to the mucous membrane.
These are the main reasons why the disease can develop. The doctor needs to identify them in order to eliminate the possibility of developing chronic conjunctivitis.
Causes and risk factors
Conjunctivitis can be contracted in different ways.
In children
Children who are already several months old become infected in the following ways:
- Contact and household. For example, when using other people's toys that have been touched by an infected child or in close contact with an infection (kissing, hugging).
- Water. As stated earlier, pathogens can be introduced by swimming in dirty water. To avoid this, it is recommended to wear safety glasses on your child while swimming.
- Airborne. Sneezing and coughing on an infected child.
Expert opinion
Ermolaeva Tatyana Borisovna
Ophthalmologist of the highest category, Candidate of Medical Sciences
Note! The likelihood of infection is increased by a weakened immune system, concomitant ENT diseases or other forms of conjunctivitis.
In newborns
The disease passes to newborns from a mother who is sick with chlamydia, trichomonas or gonococci. Infection occurs during intrauterine development or through the birth canal when a child is born.
Sometimes a child can be infected by medical staff in the maternity hospital who neglect to use disinfectants. Of course, this happens extremely rarely, but it can still happen.
The provoking factor is a weakened immune system, the unusual structure of the visual apparatus and the nasolacrimal duct.
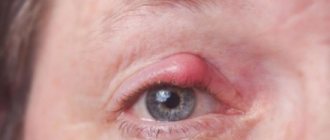
Symptoms
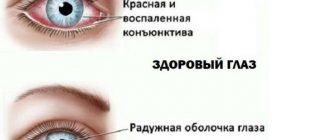
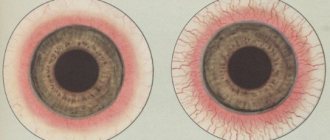
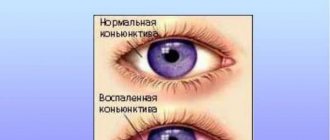
The disease always exhibits the following clinical symptoms:
- purulent discharge from the eyes, which sticks the eyelashes together in the morning, the patient cannot open his eyes;
- severe redness of the eyes;
- irritation, itching, burning, pain in the eyes;
- sensation of a foreign object under the eyelids;
- at the initial stages, increased production of tear fluid is formed, if the disease develops further, dryness of the mucous membrane is formed, which can lead to microtraumas and cracks in the cornea;
- the patient experiences discomfort, symptoms of malaise, he may have a headache, and general weakness.
Most often, ophthalmologists do not prescribe bacterial culture for conjunctivitis. The diagnosis is made based on the above symptoms, especially the presence of purulent discharge.
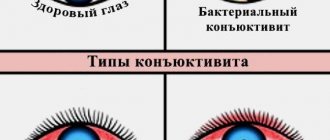
Types of purulent conjunctivitis
Depending on the root cause of formation, the disease is divided into 2 forms:
- endogenous - the cause of an infectious-inflammatory disease in other diseases, for example, sinusitis;
- exogenous - human eyes are affected by external negative environmental factors, for example, dust particles that fall on the mucous membrane.
Depending on the duration and symptoms, the disease is divided into 3 forms:
- acute – pronounced clinical symptoms;
- subacute;
- chronic – symptoms are not very pronounced, the disease periodically worsens.
Depending on the pathogen causing the disease, it is divided into the following categories:
- bacterial (staphylococci, gonococci);
- chlamydial;
- viral (influenza, parainfluenza, adenovirus), which are complicated by the proliferation of bacteria;
- fungal;
- allergenic;
- due to injury in the eye area;
- autoimmune.
If the disease is caused by a form that is not associated with bacteria, the effect of immunity in that area is weakened. Therefore, infectious agents begin to multiply rapidly, causing secondary bacterial infection.
Treatment
Therapy must be started immediately. A person must take an integrated approach. Local agents are mainly used, but systemic drugs are also possible for complications.
Eye wash
The patient's eyes are washed with antiseptics and herbal decoctions. For these purposes use:
- Furacilin (has antiseptic properties) - the tablet is dissolved in water, cooled, then using cotton pads, gently, without strong pressure, wipe the eyes from the outer to the inner edge;
- a decoction of chamomile, calendula, coltsfoot, oak bark - the method of application is the same, the products relieve irritation, soothe, and have a slight antiseptic effect;
- tea decoction or use of tea bags (antiseptic, analgesic effect, relief of irritation) - lotions are applied to the patient’s eyes using moistened cotton pads or tea bags, removed after 5-10 minutes.
It is recommended to wash the eyes before each instillation of the drug. This is necessary to eliminate purulent discharge and prepare the eyes.
Eye drops
Various dosage forms are used to eliminate bacterial infection and inflammation; there should be a break of at least 30 minutes between instillations. The following drugs are used:
- antibacterial drops – destroy bacteria, suppress their growth, are used for no more than 1 week, after this time pathogenic microorganisms develop resistance to the active substance;
- anti-inflammatory drops reduce irritation, burning, redness;
- moisturizing drops help preserve the tear film and prevent damage to the cornea;
- medicinal drops for the treatment of the primary disease (antifungal, antihistamine, antiviral agents).
Drops must be used in the area of the conjunctival sac, instilled into the inner corners of the eyes.
Some antibiotics are not suitable for children and cause side effects. Therefore, first consult with an ophthalmologist.
Ointments
At night, it is recommended to use antibacterial ointments. This is due to the fact that the therapeutic effect does not occur at night, so bacteria begin to actively multiply. The ointment is placed under the lower eyelid, after which the eyes are closed. It is not recommended to open them so that the medicinal substance does not come out.
Treatment methods
Doctors prefer to treat purulent conjunctivitis comprehensively. For mild cases, the use of local drops and ointments is sufficient. These are mainly antibiotics that block the action of the pathogen and suppress inflammatory processes.
Principles of therapy
To maximize the effect of treatment, follow the clinical recommendations:
- Flush the child with gas before using medications. The purulent exudate contains a lot of pathogenic flora. If it is not removed, treatment will be ineffective;
- wash your hands well before and after using eye drops;
- In case of severe lacrimation, instill eye drops more often, as the drug is quickly washed out from the conjunctiva. The dosage and frequency of use should be discussed with your doctor;
- treat both eyes, even if only one is affected;
- for rinsing, use sterile cotton wool or tampons - new for each eye;
- If the doctor has prescribed an ointment, it is best to apply it before the child goes to bed.
Treatment regimen at the initial stage
If the disease has just begun and has not yet fully manifested itself, you can get rid of it very quickly. For first aid, the ophthalmologist prescribes:
- washing the eyes with a weak solution of manganese;
- tetracycline ointment;
- Levomycetin drops.
The treatment regimen is as follows:
- After sleep, the baby’s eyes are wiped with a swab dipped in a manganese solution. Accumulated pus is removed from the outer to the inner corner using a syringe without a needle or a medical bulb;
- the lower eyelid is pulled down and one drop of Levomycetin is instilled. The procedure is carried out hourly;
- if pus is released during the day, it is removed and the eye is washed;
- Before going to bed, tetracycline ointment is placed behind the baby's lower eyelid.
Treatment after symptoms subside
After the discomfort in the eyes goes away and the amount of pus secreted decreases, the number of instillations is reduced to 2-4 times a day, and ointment is applied once before bedtime.
Therapy continues until symptoms disappear completely and for several more days after recovery. This is necessary to completely neutralize pathogenic microflora and minimize the likelihood of relapse.
Eye drops
How to treat conjunctivitis with purulent discharge? Doctors prescribe gentle antibiotics for children that do not cause irritation:
- Levomycetin. Suitable for children from birth, does not cause side effects.
- Albucid. Doctors prefer this drug for the absence of chemical compounds in its composition and the minimum number of unwanted reactions. The duration of therapy is limited to one week.
- Tobrex. A broad-spectrum antibiotic, effective for most types of purulent conjunctivitis.
Sometimes ophthalmologists prescribe Oftadec, but it requires careful adherence to the dose prescribed by the doctor.
Ointments
Ointments have a more concentrated composition, so using them once or twice a day is sufficient. It is best to carry out the manipulation at night. The ointment creates a protective film on the surface of the conjunctiva that has a therapeutic effect.
For children, tetracycline ointment, Floxal, is usually chosen.
Solutions
Used to wash and disinfect eyes. In addition to manganese solution, the following are allowed:
- Furacilin solution;
- decoctions of medicinal herbs (chamomile, calendula flowers, sage);
- ready-made pharmaceutical products: Miramistin, Vitabact.
Complications
If the wrong remedies are used or treatment is delayed, the patient may experience the following complications:
- spread of bacterial infection into internal tissues, high risk of sepsis;
- spread of infection to other organs and systems, for example, a sore throat or sinusitis may form;
- infectious and inflammatory diseases of the eyelids, cornea, lacrimal sac;
- transition from an acute form of a disease to a chronic one.
To avoid complications, it is not recommended to self-medicate.
Prevention
To prevent the risk of the formation of purulent conjunctivitis, it is recommended to use the following rules:
- frequent washing of hands and devices that come into contact with the eyes;
- hygiene procedures for the face;
- wearing sunglasses in windy weather;
- timely treatment of infectious diseases in other areas of the body;
- use of antibiotics according to the rules.
After complete completion of treatment for purulent conjunctivitis, you should consult an ophthalmologist again to prevent the risk of relapse of the disease or its transition to a chronic form.
Causes of conjunctivitis in newborns
An infected mother or maternity hospital staff can infect only a born child due to non-compliance with antiseptic rules.
The risk group includes newborns whose mothers suffer from gonorrhea, trichomoniasis, and chlamydia. Factors contributing to the development of pathology are:
- weak immunological activity in the baby;
- specific structure of the lacrimal canal and visual apparatus: defect or narrowness of the nasolacrimal canaliculus, excessive blood supply to the mucous membrane.
Due to the factors described above, purulent conjunctivitis is especially common in children under one year of age, and develops against the background of blockage of the nasolacrimal duct (dacryocystitis).