Conjunctivitis is a disease that can occur in both adults and children. But in the latter it occurs much more often, especially in bacterial form. The disease may go away on its own without special treatment, but in this case there is a risk of developing a number of complications, especially in children, so it is important to know what to use to wash the eyes with conjunctivitis in children and how to defeat this disease.
How to wash eyes for conjunctivitis in children
When to wash your eyes
Let's look at the most common situations when flushing is necessary.
Inflammatory diseases. Most often – conjunctivitis. Its bacterial form is always accompanied by a huge discharge of pus, especially after sleep, which sticks the eyelashes together. Washing alone will not help get rid of the disease completely, but it will improve the patient’s condition.
If something is wrong. Dust, specks, midges, and other foreign bodies cause discomfort to a person. The protective system of the eye cannot always cope with the problem and cleanse itself with the help of tears. Do not rub with your hands; you need a special liquid to cleanse your eyes.
If you feel dry. Occurs during intense visual stress: intense study, work, prolonged exposure to a monitor, reading, and can be affected by dry room air, for example, when the air conditioner is constantly running. Cleansing procedures will help restore a comfortable state.
Manifestations of recurrent disease
The repeated manifestation of signs of the disease may indicate the onset of a relapsing form. The most common cause of the chronic form of the disease is poor hygiene. In addition, a child’s low immunity can also cause symptoms after improper treatment; in such children, a relapse can be triggered by hypothermia, an outbreak of influenza, or a metabolic disorder after taking medications. In case of relapse, conjunctivitis becomes chronic, which is characterized by periodic exacerbations.
We begin treatment by rinsing
There is a simple answer to the question of how to treat conjunctivitis - start by visiting a doctor. This is due to the nature of the disease, since the disease has different forms. One can go away on its own, while the other, without proper treatment, easily becomes a chronic form and causes complications.
The doctor, having identified the cause of inflammation: virus, infection, allergy, will prescribe a comprehensive treatment, consisting of: eye treatment, installation, application of ointment, use of eye drops, strict adherence to personal hygiene, and doctor’s instructions.
Many people believe that special drops alone are enough to treat the disease. As practice shows, an important stage of treatment is washing. If you don’t do it, the recovery process will be long. By constantly rinsing your eyes, you will remove bacteria and constantly accumulating secretions.
Prevention of recurrent conjunctivitis
In order to avoid re-infection of a child with conjunctivitis, a number of simple rules should be followed, namely:
- ensure that the child does not touch his eyes with dirty hands;
- do not use bandages during treatment of the disease;
- in case of disease outbreaks, isolate the child from other children;
- change personal hygiene items daily;
- disinfect toys.
In order for the doctor to promptly diagnose a recurrent case of conjunctivitis, the child must be regularly brought to see an ophthalmologist. This is especially important in the first year after he suffered from the disease. This will help the ophthalmologist detect the disease at its first symptoms and prescribe a set of therapeutic measures. It is very important to explain to your child the need to wash his hands regularly and teach him to follow the rules of hygiene.
vitamins and minerals. In addition to vitamin complexes that are sold in pharmacies, you can also take live foods. Retinol, also known as vitamin A, is found in carrots, dairy products, liver, greens, and rose hips. Vitamin C - ascorbic acid strengthens the walls of blood vessels, preventing pinpoint hemorrhages. It is found in citrus fruits, sea buckthorn, black currants, and kiwi.
Proper eye rinsing technique
This is one of the first procedures for the disease. This can be done using different means depending on the type of illness. An ophthalmologist will help you decide and individually prescribe treatment procedures and medications that are most necessary for effective treatment.
In parallel with special drops and ointments, compresses from special decoctions are prescribed for cleansing. They contain substances that neutralize bacteria, reduce the degree of infection, and cleanse the inflamed area of accumulated secretions. This speeds up the healing process.
How and with what to wash the eye at home for conjunctivitis. The technique for correctly performing procedures depends on the situation.
If a speck, dust, or midge gets in, you need to fill your palms with another clean container of clean water, lower your eyes, and blink several times. If it doesn’t help, then to remove the foreign body you will need a cotton swab soaked in clean water. Then rinse again.
For the infectious form, the washing technique is different. Prepare two cotton pads and liquid for treatment. There is a separate tampon for each eye. The movements should be from the outer corner to the inner corner so that the separated bacteria come out. Do not reuse used cotton pads.
If you are tired, use any of the methods described above. You can also apply special ice made from herbal infusions and compresses.
How to properly wash your eyes for conjunctivitis
To prepare infusions and decoctions according to recipes, you only need water that has been boiled for at least ten minutes. Clean the bath and pipette thoroughly. One eye is washed, then all devices are re-treated so that pathogens do not pass from one to another. Strain the prepared solution through several layers of gauze.
Let's look at how to correctly perform processing in various ways:
- Pipette. The cleaning procedure is extremely simple using a pipette with special liquids. Pull back the eyelid with clean hands and pour the mixture onto the inflamed area. Do not use a product that is too hot; the temperature should be equal to body temperature so as not to cause a burn to the mucous membrane.
- A bath is a special container for cleaning. After sterilization, fill with a filtered composition at a suitable temperature. Bend over the container, dip your eyes in water for no more than a minute, for better cleansing you need to blink in the water.
- Compress. One of the most common ways to cleanse the mucous membrane. Compresses are used in the treatment of almost all forms of eye diseases and are very convenient to use. They are performed by applying a tampon soaked in a special infusion for ten to twenty minutes on the inflamed area.
Before cleansing, you should make sure that it is conjunctivitis that is causing the discomfort. Washing is harmful and useless for inflammation of the iris and iritis. Therefore, you cannot self-medicate at home; consult an ophthalmologist.
Symptoms
If the patient has an adenoviral form of the disease, the main symptoms are:
- severe redness of the eyes, minor hemorrhages may occur in the cornea, which subsequently resolve on their own;
- swelling of the skin of the eyes, due to which the eyeball is difficult to see or is completely absent;
- increased lacrimation from the eyes in the initial stages;
- possible formation of a small amount of serous discharge from the inner corner of the eyes;
- enlargement of regional lymph nodes;
- increased production of mucus from the nasal passages (rhinitis);
- increased body temperature due to intoxication of the whole body by the virus;
- dyspepsia (nausea, vomiting, abdominal pain);
- it is possible to form bubbles on the mucous membrane of the eyes, the contents of which are transparent, they can spread to the inner corner of the eye;
- a film may form on the mucous membrane of the eyes, which has a grayish-white tint, preventing normal vision;
- Often the condition can be aggravated by increased dryness of the eyes, due to which injuries and microcracks form on the cornea.
What and how to wash your eyes with conjunctivitis
If you have not yet decided on treatment methods, know that there are several effective methods. To perform the procedure, a weak composition of boric acid, furatsilin, and manganese is used. Infusion of chamomile and calendula helps well. It is used as a compress, it relieves irritation, itching, and soothes.
The choice of treatment depends directly on the cause of the disease. For the allergic form, treatment is based on the use of antihistamines. For bacterial diseases, special ointments are prescribed.
Regardless of the form or type of illness, it is important to know how to properly wipe your eyes with conjunctivitis. This is a very effective, simple procedure. Thanks to rinsing, the eyes are quickly freed from viruses and infections and return to normal.
It is important to rinse both eyes, even if one is healthy. For cleansing, special infusions and compositions are used. In order not to stain your clothes, you need to do it over the sink, covered with a towel or cellophane. Perform several times a day, do not allow the discharge to dry out.
The most common special liquids are: clean cool water, herbal infusions, decoctions, saline solution, furatsilin, chlorhexidine, black and green tea.
Causes and treatment of conjunctivitis in children
le> What signs can be used to suspect conjunctivitis in children and what to do while the diagnosis has not yet been made?
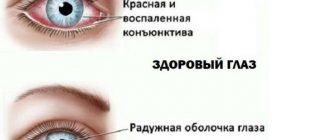
What is conjunctivitis?
Manifestations of conjunctivitis in children are very diverse. Mom can pay attention to sudden swelling and redness of the eyelids and the mucous membrane of the conjunctiva (with swelling, the conjunctiva swells, forming a ridge), lacrimation, discharge of pus or mucus from the baby’s eye: this sign can be indicated by gluing of eyelashes after sleep. The child also becomes uncomfortable in bright light: photophobia and constriction of the eyelids (blepharospasm) appear. If your baby starts rubbing his eyes, you may suspect itching and burning.
conjunctivitis appears , you should immediately consult a doctor, because without adequately prescribed treatment, the infection can spread to other parts of the eye, which, in turn, can cause decreased vision.
Also, conjunctivitis in a child can be only one of the symptoms of an infectious disease, so it is necessary to monitor the baby’s body temperature, which may increase, the presence of general weakness, and enlarged lymph nodes (often the submandibular, occipital, cervical, and parotid lymph nodes react to inflammation). From the side of the eye, it is necessary to note the dynamics: how the redness of the mucous membrane has changed, what is the quantity and nature of the discharge from the eye; The doctor will ask about this at your appointment.
Conjunctivitis in children can affect either one or both eyes - it depends on the causative agent of the infection. Inflammation caused by bacteria is often unilateral, while viral and allergic processes are predominantly bilateral.
The causes of conjunctivitis in children are very diverse. The most common conjunctivitis is of infectious origin, caused by bacteria or viruses. And the annual occurrence of the process during the flowering period of certain plants or after eating certain foods may indicate the allergic nature of the process.
Let us consider the features of the clinical course of some conjunctivitis.
Bacterial conjunctivitis in children
Diphtheria conjunctivitis. The causative agent is diphtheria bacillus. The disease occurs in children in the first year of life and begins with severe swelling and redness of the eyelids; a cloudy liquid with a reddish tint is released from the conjunctival cavity (located between the back surface of the eyelid and the front surface of the eyeball, determined when the eyelid is pulled back). The conjunctiva itself is swollen, covered with films tightly attached to it and therefore difficult to remove. Infection occurs through airborne droplets from a patient with diphtheria. Without adequate treatment, damage to the cornea (the transparent membrane covering the outside of the eyeball) may occur and its inflammation may develop - keratitis.
This conjunctivitis is often accompanied by general symptoms - an increase in body temperature to 38 - 390C, weakness, enlargement of the submandibular and pre-auricular lymph nodes.
If the diphtheria nature of the process is confirmed, the child is hospitalized in an infectious diseases hospital and placed in a separate box, since this disease is very contagious and requires special treatment.
Blennorrhoea conjunctivitis (gonoblenorrhea)
The causative agent of this conjunctivitis in a child is gonococcus. Newborns are sick, to whom the infection is transmitted when passing through the birth canal of a mother suffering from gonorrhea.
In a child, the disease begins 2–3 days after birth. Both eyes are affected at once: pronounced swelling of the eyelids is observed, their skin becomes purple, and serous-bloody fluid is released from the conjunctival cavity. After 3 days from the onset of the disease, the discharge becomes purulent, acquires a yellow-green color, and its quantity is very abundant. During this period, severe damage to the cornea may develop, leading to decreased vision.
In maternity hospitals, to prevent this severe damage to the conjunctiva, prevention of gonoblennorrhea of newborns is carried out. For this purpose, the baby’s eyes are wiped with a cotton swab moistened with a disinfectant solution, and drops of 30% sodium sulfacyl (ALBUCID) are instilled - 2 drops into each eye 3 times with an interval of 2-3 minutes.
Intrauterine infection of the fetus is possible, as well as infection through the dirty hands of a sick mother caring for a child (that is, contact with the infection can occur after preventive measures).
Pneumococcal conjunctivitis
The causative agent is pneumococcus. The disease usually affects both eyes at once; films appear on the conjunctiva, which are easily separated from the mucous membrane. This is a distinctive sign of pneumococcal conjunctivitis in children , other symptoms are similar to conjunctivitis caused by another microbe: redness of the eye, lacrimation, mucopurulent discharge. This conjunctivitis is highly contagious, and the routes of infection for infants are airborne and contact (infection through the patient’s dirty hands, infected household items, toys).
Acute bacterial conjunctivitis
Its causative agents are staphylococci and streptococci, which are activated in the conjunctival sac when immunity is reduced or the body has chronic diseases.
The disease develops acutely (literally within a few hours a picture of inflammation of the conjunctiva appears), the process begins in one eye and quickly moves to the other. Redness and swelling of the conjunctiva and eyelids and purulent discharge from the eye appear. The surface of the conjunctiva becomes uneven, bumpy - this may be accompanied by a feeling of “sand in the eyes”, and isolated hemorrhages may appear.
The route of infection is airborne or contact.
Viral conjunctivitis in children
Adenoviral conjunctivitis. The causative agent is adenovirus. The virus is transmitted by airborne droplets from a patient. The onset of the disease is acute, eye damage is preceded by an increase in body temperature to 38–390C, headache, enlargement of the submandibular lymph nodes, as well as pharyngitis (inflammation of the pharyngeal mucosa).
First, one eye is affected, and on days 2–3 the other is affected. All the typical signs of conjunctivitis appear - photophobia, lacrimation, redness of the eye, swelling of the skin of the eyelids and mucous membranes, discharge from the eyes is not very abundant, with a grayish tint. During examination, the ophthalmologist may note small tubercles on the mucous membrane of the inner surface of the eyelids - vesicles, as well as thin, easily separated films. Small hemorrhages under the conjunctiva and severe vasodilation are very characteristic.
Herpetic conjunctivitis. The causative agent is the herpes simplex virus. It enters the child’s body usually in early childhood through contact with a person with herpes, through airborne droplets or contact. Under unfavorable conditions (decreased immunity), the virus is activated and causes disease.
A distinctive sign that helps determine the cause of the process is the presence of bubbles on the wings of the nose, on the skin of the eyelids and directly on the conjunctiva.
Chlamydial conjunctivitis. This is a lesion of the mucous membrane of the eye caused by chlamydia. Chlamydial conjunctivitis occurs in newborns; infection occurs during the passage of the birth canal of a mother with chlamydia. If a pregnant woman has chlamydia, conjunctivitis in newborns is prevented: 1% TETRACYCLINE or 0.5% erythromycin ointment is placed behind the eyelid. This is done once after childbirth after the prevention of gonoblenorrhea.
In newborns, the disease is severe, affecting both eyes at once.
In young children, the pathogen can enter the conjunctival cavity along with infected water - when swimming in pools or open water bodies. At this age, one eye is more often affected; a bilateral process occurs less frequently.
At the onset of the disease, swelling of the conjunctiva and skin of the eyelids, small amounts of mucopurulent discharge from the eye, redness of the eyes, and the presence of enlarged papillae of the mucous membrane along the eyelids are observed. From about the 3rd day of the disease, an enlargement of the preauricular lymph node on the side of the affected eye occurs.
Detection of such conjunctivitis in a child requires a complete examination of the child and parents. If necessary, consultations with specialists are prescribed - an otorhinolaryngologist, a urologist, since chlamydia can affect the respiratory and urinary system in addition to the eyes.
Allergic conjunctivitis in children
The process occurs when the body is hypersensitive to any allergen substance. Their role can be food, medicine, particles of pet hair, bacteria and much more.
Allergic conjunctivitis in children to food products occurs 8–24 hours after eating them. Foods that often cause allergic reactions include citrus fruits, chocolate, fish delicacies, including caviar, eggs, strawberries or strawberries. Their breakdown products can reach the baby from the mother’s body (through breast milk) or through the introduction of complementary foods. Therefore, it is better not to include these products in the diet of young children.
Also, allergic processes can occur during the flowering period of plants, in which case an allergy occurs to the pollen of plants, such as cereals, birch and other flowering plants pollinated by the wind.
With such conjunctivitis, itching, burning (children begin to scratch their eyes), redness, severe swelling of the conjunctiva and skin of the eyelids, lacrimation, and photophobia are noted. Enlarged swollen papillae can be seen on the mucous membrane of the eyelids. Both eyes are almost always affected.
Conjunctivitis in children: first aid
If signs of eye inflammation appear in a child, the mother can carry out the following manipulations before contacting a doctor.
The most important thing is to thoroughly treat the eyes so that no discharge remains on the eyelashes, eyelids or in the conjunctival cavity. To do this, you need to take a 0.02?% solution of FURACILIN, as well as decoctions of medicinal herbs that replace it - chamomile or sage. To prepare the decoction you need to take 2 tbsp. spoons of chamomile flowers or sage leaves, pour 1 cup of boiling water, leave for 1 hour in a well-sealed container, then strain. A cotton ball or disk should be generously moistened with a warm solution (using sterile cotton wool is recommended) and the eye should be thoroughly wiped from the outer edge to the inner until completely clean. Use a different cotton ball or disk for each eye. This procedure is carried out 6 to 8 times a day. The most important thing is not to leave crusts on the eyelashes and eyelids and discharge in the conjunctival cavity! They are a cause of concern for the child and a source of infection that remains in the eye cavity (the baby can rub the eyes and contribute to the spread of infection to other parts of the eye).
After rinsing, you need to instill eye drops with an antibiotic, which should be prescribed by a doctor - LEVOMYCETINOV 0.25?% or TOBREX 0.3?% - 1-2 drops 6-8 times a day. These drugs are approved for use from the first days of life.
Mothers need to remember that if their child develops conjunctivitis, they should immediately consult a doctor and not self-medicate.
If the baby only has symptoms of conjunctivitis, it is necessary to consult an ophthalmologist, but if there is also a high temperature, runny nose, or malaise, contact a pediatrician who will make a diagnosis and refer to an ophthalmologist for special treatment.
After an examination, the ophthalmologist may prescribe additional procedures to determine the cause of the disease and select medications accordingly:
Examination of smears from the conjunctiva under a microscope. The purpose of the study is to determine the causative agent of conjunctivitis. The material is taken with a sterile disposable loop.
Before visiting an ophthalmologist, the mother should thoroughly wash the child’s eyes. There should be no discharge in the eye cavity - mucus, pus - otherwise the examination results may be false. If you do not wash the eye, the test material will be pus, i.e., the smear will contain not the pathogen, but leukocytes. Any eye drops should not be instilled before a visit to the doctor, as this makes it difficult to identify the pathogen (the pathogen is partially washed out of the conjunctival sac after using the drops, and drops containing an antibiotic can weaken or partially destroy the pathogen).
You need to take with you a diaper or a small sheet and your baby’s favorite toy – one that sounds better so that the child can look at it during the examination. The nurse or doctor pulls back the baby’s lower eyelid (while the mother holds it tightly to prevent the baby from moving and possible trauma to the mucous membrane) and draws a loop along the mucous membrane. The material is then sent to the laboratory.
The scraping may also be sent for additional examinations - culture on nutrient media (the pathogen that caused the disease will grow on the nutrient medium), as well as enzyme-linked immunosorbent and immunofluorescence tests to detect antigens of viruses or bacteria.
If the doctor suspects the allergic nature of the process, he will refer you for a consultation with an allergist to identify the allergen that caused the disease.
During the examination, the ophthalmologist may use a special dye (fluorescein) that will show whether there is damage to the cornea. Therefore, you need to take disposable tissues with you to remove traces of dye from your baby’s eyes.
Treatment of conjunctivitis in children
If the cause of conjunctivitis is bacteria, the ophthalmologist will prescribe eye drops containing antibiotics or sulfonamides. This is ALBUCID 10?% and 20?%, which can be used from the first days of life; LEVOMYCETIN drops 0.25?%, TOBREX 0.3?% are also approved for use from the first days of a baby’s life; FLOXAL 0.3?% is approved for use in children in the first months of life.
You can also use ointments containing antibiotics - 1?% TETRACYCLINE, 1?% erythromycin 2-3 times a day. Drops are instilled 6-8 times a day, almost every 2-3 hours after thoroughly washing the conjunctival cavity. As the inflammation subsides, the frequency of instillations decreases first to 3-4 times a day, and then to 2 times. Treatment is carried out under the supervision of a doctor and usually takes 7–14 days.
In case of severe conjunctivitis, the ophthalmologist can also prescribe systemic therapy - antibiotics in tablet form, anti-inflammatory drugs, but in agreement with the pediatrician.
For viral conjunctivitis in children, treatment is somewhat different. The ophthalmologist prescribes human interferon preparations - OFTHALMOFERON or inducers that promote its production - POLUDAN. The use of these drugs is allowed from the first days of a baby’s life.
POLUDAN is made in powder form; before use, it is diluted with water for injection and also instilled 6–8 times a day, 1–2 drops. It should be remembered that the activity of the diluted drug remains for 24 hours; after this time it is not effective to use.
OFTHALMOFERON is available in the form of ready-made drops and is instilled in the same way. Treatment of conjunctivitis in children takes 7–14 days and is carried out under the supervision of an ophthalmologist.
In addition to these drugs, the doctor may prescribe medications that have antiviral activity - 3% ointments ZOVIRAX or ACYCLOVIR, 0.25% TEBROPHEN. Ointments are placed behind the lower eyelid 3 times a day. Their use is possible from the birth of the baby.
For adenoviral conjunctivitis, the use of DNase has a good effect. This is a dry powder that requires dilution with water for injection. It is instilled into the conjunctival cavity 6–8 times a day, 1–2 drops. The drug is approved for use from the first months of a child’s life.
If bacterial flora is present, antibacterial drops are prescribed.
Treatment of allergic conjunctivitis in children is carried out with eye drops that have an antiallergic effect.
This is 2–4?% LEKROLIN, 0.1?% ALOMIDE, SPERSALLERG. The use of these drugs is permitted from the neonatal period. With a pronounced process, it is possible to prescribe antihistamines (antiallergic) drugs orally.
The child’s parents should follow all doctor’s recommendations, regularly wash the eyes and instill drops. It should also be noted that wearing a blindfold for conjunctivitis, especially with copious discharge, is unacceptable! A warm and moist environment is formed under the bandage; under such conditions, keratitis, an inflammation of the cornea, can develop.
One of the main conditions is that you cannot stop instilling drops on your own when an improvement appears; you must follow the duration of use recommended by the doctor, since otherwise the process may take a chronic course.
How to give drops to a child?
- To instill drops, you should either use disposable pipettes, or (if the bottle is in the form of a dropper) treat the tip of the bottle with disinfectant solutions (MIRAMISTINE, CHLORHEXIDINE) after each instillation.
- Before carrying out the procedure, you must wash your hands thoroughly. It is better for the baby to instill drops together: one person will fix the baby’s head and open the eyelids, the second will instill the drops, while you need to pull the lower eyelid down. You can also instill eye drops during the baby’s deep sleep, gently opening the eyelids.
- The pipette with the medicine should be brought close enough to the eye, but not touching it. It is enough to drop 1-2 drops - this is the capacity of the conjunctival sac.
- In order to prevent infection, instillation can also be done in a healthy eye, but with a lower frequency.
Prevention of conjunctivitis in children
The following preventive measures will help prevent conjunctivitis:
- carrying out preventive measures in the delivery room to prevent the occurrence of gonococcal and chlamydial conjunctivitis;
- compliance with hygiene measures at home (daily washing of the baby’s eyes);
- keeping the house clean, maintaining air humidity at 50–70?%, carrying out health and hardening procedures to maintain good immunity in the child.
If the mother has conjunctivitis and the baby is breastfed, which does not allow contact with him to be excluded, it is necessary to treat the mother and preventive measures for the baby - instilling eye drops, but also only as prescribed by the doctor. Mandatory preventive measures also include ventilation, humidification, hand washing, and treatment of nipples. You can quartz the room. The baby should be brought to the mother only for feeding, and mother and baby should sleep separately.
You may be interested in the tests “Moles and their meaning” and “Moles, birthmarks” on the website mamaexpert.ru
Providing first aid for eye injuries
Cleaning the inflamed area after exposure to objects or harmful substances is more important than all the following steps. Since prolonged exposure to an irritating factor causes more serious inflammation. You can treat it at home with: furatsilin, special manganese solution, boiled water, strong tea leaves.
Carry out the procedure correctly, quickly and efficiently. Rinsing with tea is the easiest way: take a cotton swab, soak it in strong tea leaves, turn your head to the side so that excess liquid drains.
It is important to wash the affected area in the right direction - from the inner corner. Blot the remaining liquid with a napkin. Wash your hands, only then you can clean another if necessary. This should be done with a fresh tea solution and a clean cotton swab.
In an emergency, if a dangerous impurity, an irritant in the form of an alkali, an acid, or another chemical substance gets in, immediately, immediately wash your eyes with plenty of running water, carry out the procedure for at least 15 minutes, call an ambulance.
The sooner you seek qualified medical help, the higher the likelihood of not losing your vision and preventing serious damage to the eye membranes.
Some more ways to wash your eyes
There are many containers that are designed for washing. Syringes, bulbs, pipettes. But there are others. For example, a container with an oval base, the shape of a glass. It is made of glass and has elongated edges that allow it to be pressed tightly against the face.
Very easy to operate. Thanks to her, the procedure becomes easy and effective. Fill the bath with a special liquid, bend over, press your vision organs to the bath, throw back your head, open your eyes wide, blink. After the procedure, you should blot the area with a clean napkin.
It is important to choose the right processing method. To carry out the procedure, use ready-made sterile pharmaceutical special solutions with a balanced neutral level; sterilized, bottled water; milk. Regardless of the washing method, the solution temperature should be 15-36°C.
A compress helps a lot - infusion of chamomile, calendula, a weak solution of potassium permanganate. Such compresses will quickly calm inflammation and relieve irritation. Apply a compress for 15 minutes.
How to wash your eyes: simple folk remedies
Is it possible to wash your eyes with chamomile for conjunctivitis without seeing a doctor? It is possible, but only after consultation with an ophthalmologist. There are a number of simple folk remedies that, when used correctly, make it possible to alleviate the condition of a sick person and defeat an infectious disease.
These traditional medicine recipes have been used for many centuries, and they have proven themselves to be very good. It’s easy to prepare a medicinal decoction using one of the well-known folk recipes.
Take a tablespoon of cumin seeds and boil in a glass of water. Add a teaspoon of cornflower petals, plantain leaves, and eyebright herb. Pour everything into a thermos and leave for a day. Then strain well to remove small particles that can cause even greater inflammation.
You can also use:
- aloe juice - squeeze the juice out of the leaf, dilute it with water 1/10;
- aloe vera tincture - take 5 leaves, add warm boiled water, leave;
- rose tincture - pour rose petals with a glass of hot water, leave for 30 minutes;
- tincture of marshmallow root - grind the root, add water, leave for 7 hours.
Infusions can be alternated, each time they should be fresh. Use a separate swab for each eye. When washing, open your eyes wide, pull back your eyelid, and use a syringe without a needle or a small bulb to inject the medicinal liquid.
Traditional recipes help speed up and facilitate the healing process. It is necessary to wipe and wash the eyes to get rid of pus, mucus, and gluing eyelashes. But this in no way replaces medical treatment. After a day there is no improvement, immediately go to the doctor.
You can use traditional medicine recipes for simple discomfort in the eye, without fear of any serious consequences.
Medicines for eye rinsing
Ophthalmologists recommend sterile medicinal infusions for washing, which also help remove harmful bacteria and fight infections. The following methods are recommended:
- treatment with Chlorhexidine, use an antiseptic only on the recommendation of a doctor, it is aggressive. After treatment, rinse the eye thoroughly with clean water and apply additional eye drops. Rarely prescribed;
- washing with Miramistin is an antiseptic that accelerates the regeneration process of mucous membranes, effectively coping with various infections and burns;
- solution of furatsilin - relieves irritation, inflammation, fights infections.
There are many medications for flushing. Only a specialist can select one after a thorough examination of the patient and finding out the cause of pain in the visual organs.
Causes
The main cause of the disease is infection with adenovirus of various strains and forms. The pathogen is transmitted through airborne droplets, but you can also get sick as a result of contact with a sick person. In the first case, the virus is transmitted through sneezing, coughing or breathing.
Initially, the pathogenic microorganism penetrates through the entrance gate of the human mucous membrane of the nasopharynx. There it causes a local inflammatory reaction, penetrating into the blood. It is from there that the pathogen penetrates the eye tissue, forming severe swelling, inflammation and redness.
How to wash your eyes with tea, chamomile, furatsilin and Miramistin
Is it possible to wash a child’s eyes with chamomile, tea, furatsilin or Miramistin for conjunctivitis? Definitely yes, since all these remedies are very effective.
Chamomile eye baths are recommended for absolutely all sick children. Pour boiling water over dry chamomile flowers, leave and strain. Dip your eyes into the resulting solution, blink so that the liquid rinses your eyeballs well. The infusion cannot be used twice.
A solution of furatsilin is the best method of cleansing, relieving inflammation. Can be used by children and adults. A properly prepared medicinal furatsilin special solution and knowledge of the basic processing rules will help you quickly achieve the desired effect.
The recipe is quite simple: take two furatsilin tablets, crush them, pour a glass of warm boiled water. Leave the solution for ten minutes, strain through a sterile gauze bandage so that no grains of tablets get in. Rinse the inflamed, irritated eye with a moistened sterile cloth.
Miramistin is simply instilled. A few drops are enough for one procedure. If for some reason the remedy is not suitable, the child will immediately experience unpleasant sensations.
Strong tea brewing is no less effective means of treatment. The main thing is that the tea contains no additives – artificial flavors, dyes. Natural supplements are not always useful. Tea with caramel is harmful, medicinal tea with chamomile is preferable.
Proper tea brewing should be cold and strong, then it has benefits - it reduces inflammation, relieves fatigue, and refreshes. It is better to wash dry, tired eyes with yesterday's tea; freshly brewed tea increases discomfort and fatigue.
Eye cleansing for newborns
Newborn babies need to have their eyes washed for hygienic purposes. The procedure should be carried out even if the tear ducts are not clogged and there is no pus. Using these preventive measures helps prevent other eye diseases.
To clean, take sterile cotton wool and moisten it with warm boiled water. Use a light movement from the outer corner to the inner corner to wipe. Use new, clean cotton wool for each child's eye. Do not use cotton pads, they are very hard and cause irritation.
The resulting pus causes the eyelashes to stick together. In this case, washing alone is not enough. All medications used to combat infection must be agreed upon with the attending physician. To wash the eyes of newborns, use solutions of potassium permanganate, boric acid, and furatsilin.
There are mothers who begin to wash the pus that appears with breast milk. Whether this can be done or not is still a controversial issue today. Some are sure that this is a natural eye treatment. Others are sure that nutritious breast milk is a favorable environment for the proliferation of pathogenic bacteria. It's better not to take risks.
Sometimes it is necessary to flush the tear ducts. This is a painless and quick procedure, you should not be afraid of it. If the tear ducts are closed, the baby is additionally prescribed a special massage.
Washing children's eyes
Before rinsing a child's eyes with conjunctivitis, he or she must be shown to a doctor. Only an ophthalmologist can prescribe the correct treatment, before making a diagnosis.
For allergies, no treatment is required.
You can cleanse children's eyes using both folk remedies and saline, since they are gentle and do not harm the baby. You can use decoctions of sage, chamomile, eyebright, and calendula, which have anti-inflammatory properties. You can wash it with a 1% boric acid solution.
You can wash with tea, green or black. Make a strong brew, take sterile cotton wool, soak it in liquid, rinse from the outer corner to the inner corner. It is better not to use cotton swabs so as not to damage the mucous membrane.
Diagnosis of recurrent conjunctivitis
The main difference between recurrent conjunctivitis and the acute form of the disease is the discrepancy between the severity of the symptoms and the objective changes that occur in the eyeball. It is possible to establish that conjunctivitis has “returned” to the child only in the ophthalmologist’s office. During the consultation, the doctor must carefully review the patient's medical history and also conduct a visual examination. For the purpose of diagnosis, the doctor uses several laboratory procedures. One of them is visometry - testing visual acuity. If a repeated case of conjunctivitis is suspected, the child may undergo biomicroscopy. This procedure allows us to identify changes in the conjunctiva and transitional folds of the eyelids, hyperemia - overflow of blood in the vessels of the eyelids and conjunctiva.
If during the examination it was discovered that recurrent conjunctiva is accompanied by other diseases, the doctor will recommend an additional visit to an allergist, otolaryngologist, gastroenterologist, dermatologist, endocrinologist. Other procedures may also be required, for example:
- taking bacterial cultures from the nasopharynx;
- radiography of the paranasal sinuses;
- chlamydia test;
- determination of blood sugar;
- allergy tests.
It also happens that recurrent conjunctivitis is associated with refractive errors, for example, myopia or farsightedness. With a sharp decrease in vision, the child often rubs his eyes with his hands, which is why recurrent conjunctivitis can develop. In such cases, the ophthalmologist performs refractometry and skiascopy - a shadow test.
Solutions for children
Individual intolerance to certain medicinal substances, unexpected allergic reactions of the child’s body, discrepancy between the child’s age and the drug used, self-medication are some of the most well-known mistakes of parents.
When faced with this insidious disease for the first time, immediately consult a doctor who, after examining the child, will prescribe the correct treatment. You cannot risk children's health, it is forbidden to experiment, you must be careful not to harm the baby's health.
However, you can diagnose a disease of a viral or bacterial form without a doctor by looking at the secretions, using Albucid. Inflammation, accompanied by pain, without discharge, is a direct sign of an allergic nature. When treating this type, mild antihistamines are used.
If the inflammation is caused by harmful bacteria, then gentle solutions are recommended for treatment, for example, chamomile decoction, furatsilin. For a child, one tablet dissolved in half a glass of water is enough. Perform the procedure from the temple to the nose, using a new cotton pad for each eye.
For infants, rinsing can be performed with a 10% Albucid solution; for older children, the use of Levomycetin, Futsitalmic, Vitabact and other drugs is allowed after consultation with the attending physician.
Why does conjunctivitis reappear in adults?
When adults again show signs of inflammation of the conjunctiva a week or a month after complete recovery, this indicates that they are faced with chronic recurrent conjunctivitis. The reasons for this phenomenon may be due to:
- The entry of viruses and bacteria into the body, provoking a repeated inflammatory process. In this case, we are talking about viral, adenoviral or bacterial conjunctivitis.
- Long-term inflammatory process of the organs of vision caused by physical or chemical exposure (burns, mechanical injuries, etc.).
- Hypovitaminosis.
- Chronic diseases of the digestive system (gastritis, cholecystitis).
- Diabetes mellitus.
- Incorrectly selected treatment regimen or non-compliance with the recommendations of the attending physician.
- Inflammation of the organs of vision, which developed against the background of diseases of the ENT organs.
Solutions for adults
When treating a mature adult body, you can use stronger infusions and drugs, having previously agreed on the treatment with your doctor. At home, an adult can independently prepare infusions and carry out treatment several times a day, which will only contribute to a quick recovery.
Procedures for an adult are recommended to be carried out with the following solutions:
- oak bark – the infusion contains a huge amount of tannins, relieves swelling and inflammation well, and easily copes with harmful bacteria;
- chamomile infusion - successfully used by adults and children; relieves inflammation, eases the course of the disease;
- cucumber juice – relieves itching, has a strong anti-inflammatory effect, normalizes the condition of the skin;
- solutions with aloe juice are used for lotions and rinses; Aloe juice is diluted one to ten with lukewarm boiled water.
At home, you can use strong brewing of ordinary black and green tea. This infusion does not have much effect on the course of the disease.