What is strabismus
In ophthalmology, strabismus is defined as an aberration of the visual axes from the vector directed at a specific object.
In this case, there is a violation of the coordinated work of the organs of vision, their stable fixation of both eyes on the object. Experts consider the objective symptomatology to be the asymmetrical arrangement of the corneas in relation to the corners and edges of the eyelids.
ICD-10 code
In the International Classification of Diseases (ICD-10), strabismus is coded H50.
Strabismus code according to ICD 10
Doctor's consultant. Convergent strabismus ICD 10
34.1. COMMON STRABISM
Strabismus is the deviation of one of the eyes from the common point of fixation, accompanied by impaired binocular vision.
SYNONYMS
Strabismus, heterotropia.
ICD-10 CODES
H50.0. Convergent strabismus.
H50.1. Exotropia.
H50.2. Vertical strabismus.
EPIDEMIOLOGY
Convergent strabismus is a social problem. It affects 1.5 to 3.5% of children. Currently, there are at least 10 million patients with strabismus in the world.
PREVENTION
Compliance with all requirements of visual hygiene, timely prescription of glasses for ametropia, general health measures. Mass early examinations of children with determination of refraction. Refraction should be determined in all children at 10-12 months and corrective glasses should be prescribed according to indications. First of all, it is necessary to examine children whose parents have some form of ametropia or strabismus.
SCREENING
Examination by an ophthalmologist according to decreed ages, annual targeted medical examination.
CLASSIFICATION
In the direction of deviation of the squinting eye
They distinguish between convergent strabismus (esotropia) - deviation of the squinting eye towards the nose; divergent (exotropia) - deviation of the squinting eye towards the temple; vertical strabismus - deviation of one eye up or down (hyper- and hypotropia). With torsional displacements of the eye (inclination of its vertical meridian towards the temple or nose) they say
about cyclotropy (ex- and incyclotropy).
By the nature of eye deviation
strabismus can be one-sided, i.e. monolateral (constantly squints one eye) and alternating (alternately squints one eye or the other).
According to the degree of participation of accommodation
In the occurrence of strabismus, accommodative, partially accommodative and non-accommodative strabismus are distinguished.
Strabismus can be periodic or constant.
ETIOLOGY
Congenital and acquired diseases of the central nervous system, general infections, mental trauma, ametropia, decreased vision or blindness in one eye (for example, with congenital cataracts).
Registration is required to continue.
Disease deforming osteoarthritis - ICD code 10
Content
Deforming osteoarthritis of the extremities (DOA) is a severe degenerative disease characterized by the progressive destruction of the cartilage tissue of the joints, accompanied by the formation of bone growths - osteophytes. It is worth noting that deforming osteoarthritis has been known to mankind for thousands of years, but even now this disease has not been fully studied and can only be cured in the early stages of development. This arthrosis, listed in the international classification under ICD code 10, leads to severe degenerative changes in the joint, which is accompanied by a change in the shape of the joint and a decrease in its mobility.
Deforming osteoarthritis. having ICD code 10, is considered a disease of old age, occurring mainly in people over 50 years of age. Statistics show that approximately 10-15% of people who undergo regular examinations have signs of developing deforming arthrosis ICD 10. In fact, arthrosis ICD 10 can begin to develop at a young age, that is, up to 25 years, but there are noticeable symptoms may appear only in old age.
Pathogenesis and symptoms of deforming arthrosis ICD code 10
Arthrosis deformans, which has an ICD code of 10, is a common disease in which, first of all, there is a decrease in regeneration in connective tissue, which leads to early aging of cartilage. The process of early aging of cartilage tissue is accompanied by the appearance of roughness on its surface, thinning, as well as loss of elasticity and strength of the tissue. In this case, compaction of the subchondral bone, complete disappearance of cartilage tissue, formation of cysts and osteophytes, as well as sclerosis of surfaces are observed.
There are 2 options for the development of deforming arthrosis: primary and secondary type. In the primary type, this disease develops due to congenital low functional endurance of the joint. Thus, the disease develops in initially healthy cartilage due to early aging. Deforming arthrosis of the second type develops due to the presence of defects observed during aseptic necrosis, trauma and hormonal disorders.
As the deformation process in the joints develops, patients experience the appearance of a number of symptoms that make it possible to determine the degree of destruction of cartilage tissue.
- Arthralkia. There are 3 main types of pain associated with deforming osteoarthritis. The most common pain is caused by mechanical damage to the joint. The joint damaged by the disease is constantly exposed to trauma, and dislocations and microfractures of cartilage tissue or sclerotic membranes are often observed in it. Type 2 pain is associated with the onset of motor activity of the joint. As a rule, painful sensations last for a fraction of a second. Type 3 pain is associated with cases of joint jamming. In the final stages of destruction, the joint “jams” quite often, which causes severe aching pain.
- Crepitus. This term refers to the most common crunch. A number of factors can contribute to the appearance of crunching, including narrowing of the cartilage gap, decreased mobility, muscle spasms, and the proliferation of osteophytes.
- Irreversible bone deformation. In this case, the process is considered irreversible, since the structure of the subchondral bones undergoes a change.
- Muscular atrophy.
- Swelling of adjacent tissues and inflammation.
Deforming arthrosis, which has an ICD code of 10, affects more and more joints over time. The symptoms of this arthrosis are most clearly visible when it affects the hip and knee joints, intervertebral cartilages, as well as small cartilages located in the fingers. The severity of the disease depends on which elements were affected. The most unfavorable is considered to be damage to the hip and small joints located in the fingers.
Degree of development of deforming osteoarthritis code according to ICD 10
Studies of deforming arthrosis have made it possible to identify the main radiological stages of the development of deformity in the affected joints.
Degree No. 1
At this stage, there is a slight change in joint mobility due to a decrease in the clearance of the joint space. Most patients at this stage do not experience pain, but there is a crunching sensation. It is at this stage that the initial processes of osteophyte formation on the lateral part of the joint can already be seen under x-ray.
Degree No. 2
The disease, which is of this degree, already manifests itself clearly not only on an x-ray, but is also noticeable for the patient. There is a serious decrease in joint mobility, muscle atrophy, and narrowing of the lumen of the joint space. The x-ray image clearly shows osteophytes and subchondral osteosclerosis of the adjacent bones.
Degree No. 3
The disease, which has entered the third stage, has many symptoms that are clearly visible in the picture. All previous problems are only getting worse. In addition, this degree is characterized by the appearance of severe swelling of soft tissues and the presence of an inflammatory process.
The changes observed with stage 3 of the disease are irreversible and lead to human disability. Some researchers of deforming arthrosis also identify the zero stage of development of this disease, during which signs of damage to the articular tissue are not yet visible on x-rays.
Diagnosis and treatment of deforming osteoarthritis
Diagnosis of deforming arthrosis, which has an ICD code of 10, begins with taking an anamnesis and taking x-rays, magnetic resonance imaging of the diseased joint, computed tomography of the spine, punctures from the area of the diseased cartilage, biopsy, and arthroscopy. All these research methods, carried out in combination, make it possible to accurately determine not only the disease itself, but also the degree of damage to the joint. Treatment of deforming arthrosis requires an integrated approach. First of all, it is recommended to reduce the load on the damaged cartilage. In this case, it is necessary to minimize motor activity, especially if we are talking about the supporting joint in the hip or knee. If there is an urgent need for movement, you must use a walker or cane.
If the disease was diagnosed at an early stage of development, treatment is carried out with chondroprotectors. However, in later stages, when there are clear signs of joint destruction, it is necessary to take non-steroidal anti-inflammatory drugs, hormonal drugs, painkillers and vitamin complexes.
If there is effusion in the joint, puncture evacuation may be prescribed to remove excess fluid. In case of severe damage, prosthetic surgery is often prescribed, and in some cases, immobilization of the joint.
Be sure to consult your doctor before treating any illness. This will help take into account individual tolerance, confirm the diagnosis, ensure the correctness of treatment and eliminate negative drug interactions. If you use prescriptions without consulting your doctor, it is entirely at your own risk. All information on the site is presented for informational purposes and is not a medical aid. All responsibility for use lies with you.
ICD-10 - International Statistical Classification of Diseases and
health problems (updated 2007)
Class VII
Diseases of the eye and its adnexa (H00-H59)
Excluded:
- certain conditions that arise in the perinatal period (P00-P96);
- some infectious and parasitic diseases (A00-B99);
- complications of pregnancy, childbirth and the postpartum period (Q00-099);
- congenital anomalies, deformations and chromosomal disorders (Q00-099);
— diseases of the endocrine system, nutritional disorders and metabolic disorders (E00-E90);
— injuries, poisoning and some other consequences of external causes (S00-T98);
— neoplasms (C00-D48);
- symptoms, signs and abnormalities identified during clinical and laboratory tests,
This class contains the following blocks
H00-H06 - Diseases of the eyelids, lacrimal ducts and orbits
H10-H13 - Diseases of the conjunctiva
H15-H22 - Diseases of the sclera, cornea, iris and ciliary body
H25-H28 - Diseases of the lens
H30-H36 - Diseases of the choroid and retina
H43-H45 - Diseases of the vitreous body and eyeball
H46-H48 - Diseases of the optic nerve and visual pathways
H49-H52 - Diseases of the eye muscles, disorders of concomitant eye movement, accommodation and refraction
H53-H54 - Visual impairment and blindness
H55-H59 - Other diseases of the eye and its adnexa
The following categories are indicated by an asterisk:
H03* - Lesions of the eyelid in diseases classified elsewhere
H06* - Lesions of the lacrimal apparatus and orbit in diseases classified in other headings
H13* - Lesions of the conjunctiva in diseases classified elsewhere
H19* - Lesions of the sclera and cornea in diseases classified elsewhere
H22* - Lesions of the iris and ciliary body in diseases classified elsewhere
H28* - Cataracts and other lesions of the lens in diseases classified elsewhere
H32* - Chorioretinal disorders in diseases classified elsewhere
H36* - Retinal disorders in diseases classified elsewhere
H42* - Glaucoma in diseases classified elsewhere
H45* - Lesions of the vitreous body and eyeball in diseases classified elsewhere
H48* - Lesions of the optic (2nd) nerve and visual pathways in diseases classified elsewhere
H58* - Other lesions of the eye and its adnexa in diseases classified elsewhere
Diseases of the eyelids, lacrimal ducts and orbits (H00-H06)
H00 Hordeolum and chalazion
H00.0 Hordeolum and other deep inflammations of the eyelids
Other forms of strabismus (h30)
h30.0 Convergent concomitant strabismus
Esotropia (alternating) (monocular), except intermittent
h30.1 Concomitant divergent strabismus
Exotropia (alternating) (monocular), except intermittent
h30.2 Vertical strabismus
h30.3 Intermittent heterotropia
Intermittent. esotropia >. exotropia > alternating (monocular)
h30.4 Other and unspecified heterotropies
Concomitant strabismus NOS Cyclotropia Hypertropia Hypotropia Microtropia Monofixation syndrome
h30.5 Heterophoria
Alternating heterophoria Esophoria Exophoria
h30.6 Mechanical strabismus
Brown's capsule syndrome Strabismus due to adhesions Traumatic limitation of the elasticity of the eye muscle
h30.8 Other specified types of strabismus
Duane syndrome
h30.9 Strabismus, unspecified
International Classification of Diseases, 10th Revision (ICD-10)
Class 7 Diseases of the eye and its adnexa
h39-h32 Diseases of the eye muscles, disorders of concomitant eye movement, accommodation and refraction
h39 Paralytic strabismus
- h39.0 3rd [oculomotor] nerve palsy
- h39.1 4th [trochlear] nerve palsy
- h39.2 6th [abducens] nerve palsy
- h39.3 Complete external ophthalmoplegia
- h39.4 Progressive external ophthalmoplegia
- h39.8 Other paralytic strabismus
- h39.9 Paralytic strabismus, unspecified
h30 Other forms of strabismus
- h30.0 Convergent concomitant strabismus
- h30.1 Concomitant divergent strabismus
- h30.2 Vertical strabismus
- h30.3 Intermittent heterotropia
- h30.4 Other and unspecified heterotropies
- h30.5 Heterophoria
- h30.6 Mechanical strabismus
- h30.8 Other specified types of strabismus
- h30.9 Strabismus, unspecified
h31 Other concomitant eye movement disorders
- h31.0 Gaze paralysis
- h31.1 Convergence insufficiency [insufficient and excessive convergence]
- h31.2 Intranuclear ophthalmoplegia
- h31.8 Other specified disorders of conjugal eye movement
- h31.9 Concomitant eye movement disorder, unspecified
h32 Impairments of refraction and accommodation
- h32.0 Hypermetropia
- h32.1 Myopia
- h32.2 Astigmatism
- h32.3 Anisometropia and aniseikonia
- h32.4 Presbyopia
- h32.5 Accommodation disorders
- h32.6 Other refractive errors
- h32.7 Refractive error, unspecified
Sources: https://prounly.ucoz.ru, https://artrozmed.ru, https://glazzky.narod.ru, https://mkb-10.com, https://medi.ru/icd10/ 7h39h32.htm
Next:
- How to prevent strabismus
- March 03, 2021
No comments yet!
Forms
Ophthalmological disease can be congenital or acquired. In the first case, it may be present in the newborn or appear in infants up to six months of age.
The most common types of horizontal strabismus are:
- convergent friendly;
- divergent friendly.
Less commonly diagnosed is a vertical form with an upward (hypertropia) and downward (hypotropia) direction.
| Types of disease | ||
| Name | How it manifests itself | Code |
| Convergent friendly | Turning 1 or 2 eyes inward | H50.0 |
| Divergent friendly | Turning 1 or 2 eyes outward | H50.1 |
| Vertical |
| H50.2 |
| Intermittent |
| H50.3 |
| Unspecified and other heterotropies |
| H50.4 |
| Heterophoria |
| H50.5 |
| Mechanical |
| H50.6 |
| Dr. refined varieties | The congenital type of the disease is rare. Refers to the inability of the eye to move outward | H50.8 |
| Unspecified | ————- | H50.9 |
Diagnostics
The examination of a patient with strabismus begins with a detailed medical history. The ophthalmologist uses a physical examination to draw attention to the movement of the eyeballs. The position of the eyes is assessed by fixing vision at near and far distances with and without the corrective lenses included in the kit. Mandatory studies include the following procedures: With constant exotropia, vision on the affected side is reduced. With the intermittent form, visual function can be maintained at a high level for a long time. The examination is carried out without correction and with glasses. • Autorefractometry.
Divergent strabismus is often combined with refractive errors.
According to statistics, hypermetropia predominates in patients, and myopia is very rare. The study is carried out for cycloplegia. • Coverage test.
With alternating overlap, eye movements are visualized from outside to inside.
Test results may vary depending on how far the patient's vision is set. When properly corrected, the range of motion in glasses is usually less. • Four-point Worth test.
The study allows us to determine the nature of vision.
With a small angle of strabismus, vision is binocular or simultaneous. A constant and large angle is associated with the monocular nature of vision. • Survey in the synoptoforum.
This allows you to accurately determine the angle of deviation with and without eyepiece correction. In the case of continuous exotrophy, the ability to bipolar connection is lost.
General characteristics of the disease
The proportionate position of the organs of vision ensures that the image falls on the central zone of the eyes. Subsequently, visual information enters the sections of the analyzer, where it is layered.
This produces a single binocular image. If there is a deviation, the overall picture is impossible, which is explained by the refusal of the nervous system to process information from the affected eye.
The pathology can be localized in one eye or affect both organs of vision. Taking into account the nature of the course of the disease, the following types are recognized.
Alternating strabismus
The main symptom of the disease is alternate distortion of the projection by the eyes. It is important that their deviation from the norm is almost identical. If the patient examines objects with one eye or the other, this indicates the functionality of both organs.
Both eyes with an alternating type of pathology see non-identical images. The brain cannot process them at the same time, so only one organ is actively working. The second one stops seeing over time.
Amblyopia with alternating strabismus develops, but less intensely.
Monocular
The main symptom is that the lesion is observed on one organ. People never use it. Visual function is reduced, the brain reads information only from the non-squinting eye. Dysbinocular amblyopia develops on the oblique organ due to functional inactivity.
Reference! After a series of studies, the ophthalmologist concludes that it is possible to restore vision in a squinting eye. If there is no chance, only a cosmetic defect is corrected.
In addition to a visual examination by a doctor, a thorough examination is required to identify the provoking factor and the condition of the eye tissue. Depending on the causes, the disease is divided into two types.
Friendly
The disease is diagnosed mainly in children. Upon visual inspection, the following nuances are noted:
- both eye sockets are movable;
- identical location of both eyes;
- There were no disturbances in binocular vision or double vision.
Paralytic
The pathology develops against the background of paralysis of the muscles of the oculomotor system. Among the provoking factors: diseases affecting the central nervous system, brain, muscle tissue.
The movement of the affected organ is impaired. Diplopia develops when the image hits the retina. Paralytic strabismus progresses when looking towards the affected area (muscle, nerve, etc.).
Causes of convergent concomitant strabismus
Only one type of convergent strabismus is not considered a pathology, this is the displacement of the eyes relative to one visual center at the age of up to 3 months after birth. The eye muscles learn to act in concert, and the rudiments of binocular 3D perception are formed. The ability of the brain to combine images coming from two eyes into one three-dimensional image is fully formed in children by the age of 7.
Convergent strabismus can manifest itself as a shift to the center of one or both eyes. In the first case, we can talk about the paralytic type of strabismus, and in the second, about the friendly type. Most often, a concomitant type of pathology is observed in children and becomes noticeable before the age of one year. The causes of visual impairment are most often congenital.
The main causes of concomitant strabismus in children:
- Disruption of the normal course of pregnancy in the mother.
- Pathologies in children under one year of age, including injuries and infections.
- Hereditary factors.
The presence of close relatives with serious visual pathologies is only a risk factor that increases the likelihood of the disease in children. It is not strabismus itself that is inherited, but the spectrum of conditions for its development. The following pathological conditions can provoke strabismus, if there is a predisposition:
- intrauterine or acquired disorder of the central nervous system;
- severe infection;
- fear or prolonged stress;
- head or eye injury;
- abnormalities of the visual apparatus in children;
- large difference in diopters between eyes;
- pronounced farsightedness or myopia;
- disruption of the shape of the lens and cornea, which leads to blurred images (astigmatism).
The classification of ophthalmological disorders accompanied by convergent strabismus is quite extensive. When diagnosing, the persistence of the disorder, the angle of deviation from the normal center of fixation, and many other factors are taken into account. An important step in diagnosing strabismus is determining the alternating or monolateral type of strabismus.
Possible reasons
The list of provoking factors is quite extensive. All of them are divided into 2 groups: congenital and acquired.
Sources of motor dysfunction of the organ of vision are:
- mechanical and mental injuries;
- damage to the central nervous system;
- paralysis of the oculomotor nerve and other tissues;
- ametropia of moderate and high degree;
- stressful situations;
- infectious diseases;
- deviations from the norm in the development of the muscles of the oculomotor system;
- somatic diseases;
- decreased vision in one eye.
Causes
In children, convergent strabismus develops as a result of:
Infections suffered by the expectant mother during pregnancy. Hereditary factor. Presence of neurological diseases. Severe increase in body temperature. Diseases of the visual apparatus. Incorrect placement of toys above the crib. Abnormal development of the eye muscles. Intrauterine intoxication.
Convergent strabismus in the early stages of development of the baby’s visual system
Place the mobile above the crib correctly - otherwise the child runs the risk of developing strabismus.
In adulthood, convergent strabismus may appear as a consequence of:
Injury Toxic poisoning. Various vision defects (most often farsightedness or myopia). A noticeable difference in the strength of the eye muscles. Endocrine disorders. Stress. Mental illnesses.
Convergent strabismus in adults
Paralysis of the eye muscles also leads to the development of strabismus in adults.
Symptoms
It is easy to recognize an ophthalmological disease by eyes that are tilted to the side (usually towards the bridge of the nose). A similar manifestation occurs in infants, but by the age of 6 months, in the absence of pathology, everything returns to normal.
Signs of a concomitant form of pathology:
- alternating displacement of the eyes (or one);
- when focusing the gaze on a stationary object, one organ of vision deviates to the side (down, up, to the nose, to the temple);
- the angle of deviation of the squinting eye when viewing a certain image is almost always equal to the angle of deviation of the fellow eye;
- no ghosting effect;
- decreased vision in the affected eye;
- lack of binocular vision.
The paralytic form is recognized by the following manifestations:
- lack of binocular vision;
- possible ghosting effect;
- the secondary aberration angle is greater than the secondary one;
- lack of turning of the eye towards the affected muscle (nerve);
- dizziness;
- aberration towards the affected muscle.
| Symptomatic manifestations of other forms of the disease | |
| Type of strabismus | Signs |
| Convergent | The pupil is observed to be directed towards the bridge of the nose. |
| Divergent | The pupil looks at the temple. |
| Vertical | Eye deviation up or down. |
Treatment
Treatment methods are selected taking into account the causes and nature of the pathology.
In children
When diagnosing the disease in children, correction is carried out before the end of the period of formation of the visual organ. This is approximately 18-25 years old. The peculiarity of treatment measures is an integrated approach, since pathology disrupts the functioning of the analyzer departments.
Conservative treatment involves the use of various devices. Courses are repeated up to 4 times a year. The main efforts are aimed at improving vision and involving the affected organ in the physiological process. The connections between the eyeballs are also regenerated, when the visual image is formed from data taken from both eyes.
If diagnosed early, a child’s visual defect can also be corrected with the help of properly selected glasses. Lenses are able to regulate the degree of load on each organ. They also help both organs focus their gaze on an object.
If traditional treatment is unsuccessful, surgery is prescribed. These are not complex manipulations that are performed to restore muscle activity. They are carried out under anesthesia for 40-60 minutes. 1.5 hours after the operation the patient is discharged home.
In adults
To solve the problem, a therapeutic or surgical treatment method is chosen.
- Pleoptic
The essence of the therapy is to create an impact on the visual system of the diseased organ using therapeutic computer programs and a laser. The purpose of the manipulation is to artificially increase the load to train muscles.
- Orthoptic
This method involves the use of equipment. The complex program also includes special exercises. The main tools in therapy are computer programs, devices (synoptic) and other devices. Thanks to the intensive course, it is possible to improve binocular vision.
- Diploptic
Therapy is carried out in conditions close to natural. The essence of the technique is to eliminate functional suppression using the optomotor fusion reflex.
Reference! You should not rely on vision distortion to improve spontaneously. Without therapeutic correction, complications are inevitable.
- Botulinum toxin injections
Botox on the eyes is the latest technique that eliminates cosmetic problems. Vision does not improve after the injection.
Treatment of strabismus
The treatment method for strabismus (strabismus) depends on many different factors, such as the patient's age, the cause and type of the disease, and the degree of deviation. With strabismus, the eye is deviated to the side and, over time, reduces its visual functions. Therefore, treatment is recommended as early as possible.
Convergent strabismus in a girl
- Optical correction (wearing glasses or contact lenses of increased softness).
- Carrying out hardware procedures to improve visual acuity.
- Carrying out orthoptic treatment (using synoptic drugs and special computer programs).
- Carrying out diploptic treatment (natural conditions for the development of binocular vision).
- Treatment of strabismus with folk remedies (this treatment is effective in the initial stages of the disease, and is primarily aimed at strengthening the eye muscles): • Chocolate. • Decoctions and infusions of herbs. • Alcohol infusions. • Phytotherapeutic drops. • Exercises for the eye muscles.
- Surgery to eliminate strabismus (performed in one day, using local anesthesia, recovery takes about a week, a course of medications is recommended to restore visual function).
Strabismus due to genetic congenital anomalies
The method of treating strabismus is chosen by an ophthalmologist after clarifying the diagnosis and determining the specific type of strabismus.
In some cases, only a few therapeutic procedures are sufficient, and sometimes there is simply a need for serious surgery, in which one or both eyes are operated on
Surgical and non-surgical treatment
If conservative therapy does not lead to the desired result, surgical treatment is prescribed. The surgeon eliminates part of the vision problem, but special exercises are required for complete recovery.
The surgical method clearly solves the cosmetic problem. To improve vision, additional non-surgical measures are needed to equalize the functionality of both eyes.
Surgical intervention becomes necessary when there is damage to muscle tissue. Muscle balance is achieved through surgery. Not all types of the disease can be treated using this method. Sometimes it is more advisable to use less traumatic means, for example, glasses with prisms.
Modern ophthalmological centers offer a wide range of services to eliminate the disease. Correction of impaired motor function of the eyes is carried out using special devices. Monobinoscopes and synoptophores show good results.
The duration of the course and the set of treatment measures are developed differently for each patient. On average, 5 to 10 procedures are required.
Stages of therapy:
- eliminating manifestations of amblyopia (hardware effects, stickers, etc.);
- resumption of connections between the eyeballs;
- correction of muscle balance (mainly surgically);
- correction of vision, in which the shapes, sizes and distance to the object in question are perceived.
Reference! You cannot put off going to the ophthalmologist; the longer the disease develops, the more difficult it is to treat.
Types and stages of treatment for strabismus
Many patients consider strabismus treatment to be only a correction of a cosmetic defect, and complaints during an appointment with an ophthalmologist can only be about external manifestations. Meanwhile, deviations that are subtle at first inevitably develop into serious vision problems, even if strabismus occurs spontaneously or from time to time.
Convergent strabismus is accompanied by a number of unpleasant sensory disturbances, which are marked by certain symptoms:
- Diplopia is double vision. May in turn cause headaches and dizziness.
- Decreased vision, forming a vicious circle. Amblyopia aggravates strabismus, which further impairs vision and increases the deviation of the eyeball to the side.
- Functional scotoma is the brain's exclusion of the signal from the deviating eye. A three-dimensional image does not appear.
- Lack of depth, volume, binocular vision. Turbidity and blurriness of the visible image.
Treatment of strabismus involves getting rid of associated unpleasant symptoms, cosmetic correction, and restoration of vision. This requires eradication of the main cause of the pathology, which means a careful examination is needed to establish an accurate diagnosis. The diagnosis itself may consist of many medical terms in several lines, giving a complete picture of the disorder, determining treatment tactics, and its duration.
Diagnosis is possible in children from a very early age; congenital pathology can be definitively established at the age of 10–11 months. Acquired strabismus begins to appear after a year of life. Preschoolers most often suffer from strabismus, but the same process can begin at any age, if provoking factors arise.
The best time to treat strabismus in children is between 2 and 4 years of age. In this case, with due diligence, it is possible to correct the deviation as much as possible before school. This allows you to avoid psychological problems in children and minimize educational lag due to poor vision.
Methods for treating convergent strabismus
The method applicable in each specific case is selected by an ophthalmologist based on the diagnosis. An important role in prescribing effective treatment is played by the division of the mechanism of development of the disorder. There are three main types of convergent strabismus:
- Accommodative. Occurs due to farsightedness or myopia. Can be corrected with properly selected glasses.
- Partially accommodative. Shows slight improvement with bifocals, but does not go away completely. Fresnel prisms glued to lenses are also used.
- Non-accommodative. It cannot be corrected with glasses; hardware therapy and subsequent surgery will be required.
Treatment for any type of strabismus should be comprehensive and consistent. Each stage is developed by an ophthalmologist based on an examination and depends on the patient’s age, the size of the angle of discrepancy between the eyes, and the effectiveness of the previous stages of therapy.
Treatment for strabismus is based on the following methods:
- correction using glasses or lenses;
- occlusion: exclusion of the healthy eye from the visual process (for example, using a blind bandage);
- hardware correction using orthoptic exercises, special gymnastics for the eyes;
- drug therapy aimed at relaxing or tightening various eye muscles;
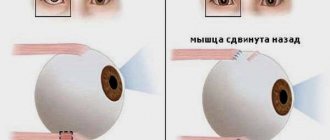
- a surgical operation to change the strength of the muscles that ensure synchronous eye movement: strengthening (resection) or weakening (recession), according to individual indications.
Important! The operation is indicated for very young patients with a congenital form of strabismus with a large angle of deviation. In other cases, treatment begins with conservative methods in children and adults. If therapy does not produce noticeable results within 1.5 years, surgery is prescribed.
The use of modern surgical methods, in particular, a radio wave knife, makes it possible to perform operations to correct convergent strabismus in a matter of hours and go home on the same day. With severe strabismus, several step-by-step operations with a gradual change in the angle of deviation may be required.
The operation itself does not solve the entire problem; it is considered only as a stage of complex treatment that takes several years.
Mandatory stage of successful therapy
The recovery period after surgical treatment of strabismus is as important as the operation. Even in young patients, with timely surgical intervention, full restoration of functions and consolidation of bipolar vision takes up to two years. In adults, the rehabilitation period can be much longer.
Without daily gymnastics, hardware simulators and compliance with doctor’s recommendations, there is a high risk of relapse, even with the most successful surgery. With this disorder, attention will have to be paid to vision throughout life: avoid overexertion, sunburn, infections, injuries, and observe a rest regime.
A prerequisite for the effectiveness of therapy for convergent strabismus is the creation of a favorable environment for the restoration of normal visual functions: good nutrition, proper lighting, daily exercises according to medical recommendations.
Restoring full bifixation, as the basis of binocular vision, is a task that can be solved after surgery. Success in a situation where correction is still possible depends on the perseverance and perseverance of the patient himself.
Forecast
Minor deviations detected at an early stage of strabismus can be cured by wearing glasses and special exercises. This may take from several months to a year and a half.
Good prognosis for surgery. Restoring muscle mobility promotes rapid recovery. Complex treatment may take 1.5-2 years.
It is quite difficult to restore vision of advanced strabismus to patients in adulthood. This is due to lost time and the development of related problems.
Possible complications
Complications after surgery are rare. However, risks cannot be excluded, as with any other surgical intervention. Among the possible manifestations:
- infections;
- decreased vision;
- adverse reactions to anesthetics;
- ghosting effect;
- incorrect alignment of the eye axis.
Preventive measures
To avoid vision problems, it is recommended to adhere to the following recommendations.
- You should not put heavy strain on your eyesight. If your work involves them, you need to give your eyes a rest for 10-15 minutes every hour. At this time, you need to close them and try to completely relax the eye muscles.
- You should visit an ophthalmologist at least once every six months for a preventive examination. Diseases detected at an early stage are much easier to treat.
- After an injury or other damage to the face and head, you should see a doctor.
- When performing hygiene procedures or applying makeup, it is recommended to handle your eyes with extreme caution. Any strong impact is fraught with tissue damage.
- If your vision deteriorates (myopia, farsightedness, astigmatism), you should visit the clinic to select a correction method.
It is easier to prevent a disease than to deal with pathological manifestations and complications. Sometimes it is impossible to regain vision due to lost time. The conclusion suggests itself: you need to visit a doctor regularly for early detection of the problem and its treatment.
Watch a video about strabismus: