Etiology of the disease
What is night blindness?
This is a specific ophthalmological disorder, which can be an independent disease or a symptom of other eye pathologies. The patient experiences spatial disorientation at late times of the day. Adaptation to poor lighting is minimal. The field of vision narrows, the person feels blinded. The disease night blindness usually affects older people. The exception is cases of congenital night blindness. It can be diagnosed at an early age, and gene mutations are called the causes of hemeralopia.
Night blindness is caused by dysfunction of the retina. The production of rhodopsin, a specific pigment in the optic rods, decreases. Under the influence of light, this substance disintegrates, and in the dark it is restored. Thanks to this reaction, people have the ability to adapt to lighting. With normal production of rhodopsin, the eye quickly adapts to any lighting conditions, with the exception of complete darkness.
The pigment is formed when there is a sufficient amount of vitamin A. That is, vitamin deficiency is one of the reasons for weakened vision. A decrease in adaptive capabilities is observed with zinc deficiency. The disease also develops with a lack of vitamin B2. This hemeralopia is called essential. It is also caused by other reasons:
- malnutrition;
- prolonged exposure to toxins on the body;
- liver and stomach diseases;
- diabetes;
- pathologies of the biliary tract.
What vitamin deficiency causes night blindness? In addition to retinol and B vitamins, the eyes need nicotinic acid. It participates in redox reactions and normalizes capillary blood circulation. Deficiency of this vitamin leads to hypoxia of eye tissue.
Symptomatic hemeralopia occurs with glaucoma, extreme myopia, and optic nerve atrophy. Hemeralopia or night blindness can be a consequence of radiation burn or retinal detachment. Cataracts and age-related farsightedness also provoke a decrease in twilight vision. To make an accurate diagnosis, it is necessary to focus on symptoms and instrumental research methods.
Lack of vitamin A: is it dangerous for vision?
Vitamin A (retinol) plays an extremely important role in the functioning of the human visual organs. This substance is responsible for the production of a sufficient amount of melanin, which is necessary to ensure normal visibility in the dark. Therefore, one of the most obvious signs of deficiency of this component is hemeralopia, or “night blindness”. With this disease, the clarity of vision in a person at dusk is significantly reduced, and the process of adaptation to darkness lasts quite a long time - from 7-8 seconds to several minutes. The thing is that retinol regulates the functioning of light-sensitive pigments of the retina: visual purple, rhodopsin and iodopsin. Rhodopsin is responsible for capturing minimal light, which is extremely important for normal vision at night. In turn, visual purple is responsible for the speed of eye adaptation to darkness.
Thus, vitamin A deficiency leads to twilight vision disorder. It has been scientifically proven that the most retinol accumulates in the retina of the eye. Therefore, its lack quickly leads to a decrease in vision clarity due to disruption of light-sensitive pigments. In addition, other unfavorable symptoms in the visual system occur.
Lack of retinol often causes the development of dry keratitis, which is associated with drying out of the mucous membrane of the eye due to partial atrophy of the lacrimal glands. Drying of the cornea leads to a decrease in its protective and barrier functions, which helps create a favorable environment for the development of various eye infections. If left untreated, they can lead to serious consequences, including necrosis of eye tissue and loss of vision.
Hardening and drying of the cornea due to a lack of vitamin A contributes to the exfoliation of cells and partial blockage of the tear ducts. This leads to dehydration of the conjunctiva and the appearance of an inflammatory process in the eyelid area (conjunctivitis). In addition, experts say that a deficiency of this substance in the long term can provoke the development of glaucoma or xerophthalmia. Thus, a lack of retinol in general negatively affects the health of the human visual system. If you have at least one of these symptoms, it is recommended to take a test for the presence of vitamins in the body and, if necessary, replenish the missing nutrients.
Why is a lack of retinol dangerous for the visual system?
- Partial or complete loss of vision at night (“night blindness”);
- Long-term adaptation of the eyes to darkness (from 7-8 seconds to several minutes);
- Development of dry keratitis;
- Reduced barrier and protective functions of the cornea due to drying out;
- Partial blockage of the tear ducts and the appearance of an inflammatory process in the eyelid area (conjunctivitis);
- Development of glaucoma and xerophthalmia.
Causes of hemeralopia
Violation of twilight vision is scientifically called hemeralopia, and popularly called “night blindness”. This disease is associated with dysfunction of the retina and optic nerve. It seems to a person that at dusk the entire world around him seems to be shrouded in a thick haze. Vision weakens and orientation in space is lost.
This disease not only causes inconvenience, but can also be life-threatening, for example, it increases the risk of a car accident at night. In addition, with such an illness, the field of vision narrows and adaptation to light changes. Any bright ray from the darkness can lead to disorientation in space and loss of coordination of movements. Often, those suffering from night blindness have difficulty perceiving shades of yellow and blue.
If a person notices such symptoms, then he should contact an ophthalmologist as soon as possible to reverse the loss of vision.
Representatives of both the stronger and weaker sex, especially the elderly, suffer from hemeralopia. However, ladies of Balzac's age during menopause are more susceptible to it. According to the observations of scientists, the least number of people with night blindness are among the peoples of the Far North, whose eyes have adapted to the polar night.
This disease can be congenital or acquired. The first type is rare and is diagnosed in early childhood.
The occurrence of the second type of hemeralopia depends on many reasons:
- lack of vitamin A, B2, nicotinic acid;
- physical exhaustion;
- anemia;
- eye diseases;
- childhood diseases (chickenpox, measles);
- toxic poisoning;
- alcohol abuse and drug addiction;
- sunburn of the conjunctiva;
- pregnancy.
Very often, a person begins to see poorly at dusk due to a lack of vitamin A. Its deficiency leads to deformation and destruction of photoreceptors. The lack of vitamins and microelements is most noticeable in the spring. Therefore, it is in the spring that patients with night blindness experience exacerbations.
Acquired hemeralopia is divided into essential and symptomatic. The first is characterized by problems with the retina, caused precisely by a lack of vitamins, as well as exhaustion, alcohol abuse, intestinal diseases, etc. The second type includes forms of “night blindness” caused by diseases of the visual organs, in particular, severe myopia, glaucoma, atrophy optic nerve and others.
Symptoms of the disease
Symptoms of hemeralopia are closely related to the types of this vision pathology. So, there are 3 types of disease:
Congenital hemeralopia
- progressive decrease in vision, noted from early childhood;
- discomfort of visual perception in a darkened space;
- spatial disorientation in poorly lit rooms;
- incorrect perception of all yellow and blue shades;
- fear of the dark, developing into a phobia;
- restlessness and increased anxiety with the onset of darkness.
Symptomatic hemeralopia
- the presence of organic diseases of the retina, choroid;
- difficult to correct myopia;
- siderosis (accumulation of iron salts in the eye tissues);
- taperetinal dystrophies.
Essential hemeralopia
- functional pathology of the retina;
- violation of the metabolism of certain vitamins (especially vitamins A, B2, PP);
- insufficient or unbalanced nutrition;
- liver diseases;
- disruption of the digestive system;
- toxic total damage to the body;
- prolonged exposure to too bright light.
Common symptoms of hemeralopia, regardless of the causes of its occurrence, are:
- impaired visual perception due to poor visibility;
- blurred vision at night;
- blurred perception in the dark, as well as during a sharp transition from a very bright to a darker room;
- blurred perception of the contours of objects;
- inability to perceive yellow and blue colors;
- insufficient sensitivity of the eyes to the flow of light.
How to get rid of night blindness
Treatment of this disease is possible only if it is acquired. Congenital hemeralopia cannot currently be treated.
In order to prescribe a course of treatment, the ophthalmologist must identify the cause of the disease. This is done through various studies.
These may include:
- scotometry;
- fundus examination;
- perimetry;
- dark adaptometry;
- electroretinography;
- Ultrasound of eye vessels.
When the factor provoking the disease is identified, therapy is aimed at getting rid of it.
For the most common ailments that provoke symptomatic hemeralopia, the following treatment can be used:
| Initial disease | Treatment method |
| Severe myopia | Laser correction or refractive surgery (scleroplasty, artificial lens implantation). |
| Cataract | Phacoemulsification or cataract extraction. |
| Glaucoma | Antiglaucomatous surgery. |
| Retinal detachment | Laser coagulation. |
In the case of essential form of night blindness, the doctor examines the level of retinol in the blood. After this, he prescribes a special diet and vitamin and mineral complexes. You may need to visit a gastroenterologist or endocrinologist.
Vitamin-mineral complexes must contain the required amount of vitamin A (beta-carotene), ascorbic acid, lutein, selenium, zinc, copper and taurine.
Diagnostics
With initial symptoms of decreased twilight vision, it is necessary to obtain qualified consultation from a specialist. The ophthalmologist conducts traditional studies: visometry and ophthalmoscopy. However, the final diagnosis can be established after additional studies:
- Electroretinography is a study of the retina by recording electrical potentials that are a response to light stimulation;
- Tonometry - the study allows you to determine IOP, the volume of intraocular fluid, its outflow coefficient;
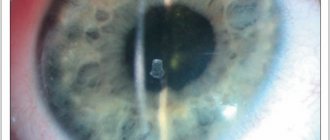
Carrying out tonometry according to Maklakov - Refractometry - determines the ratio of the refractive power in the optical system of the eye and its correspondence to the longitudinal axis of the eyeball under the condition of resting accommodation;
- Biomicroscopy - allows you to conduct microscopy of the main ocular structures: the anterior chamber, cornea, iris, lens, vitreous body. Using a Goldmann lens, fundus examination is possible;
- OCT (optical coherence tomography) – scanning the back wall of the eye to determine the parameters of the optic disc, the condition and thickness of the retinal layers.
Carrying out biomicroscopy of the eye
If necessary, a comprehensive examination is supplemented by consultations with an endocrinologist, gastroenterologist and other highly specialized specialists.
Prevention
Let's turn to the scientific explanation for the formation of night blindness and immediately understand that dietary correction and preventive use of retinol will significantly improve the situation. The diet includes foods containing ascorbic and nicotinic acids, B vitamins and retinol derivatives. It is useful to eat fish oil, nuts, apricots, and green salad. A decoction of rosehip, which replenishes the deficiency of ascorbic acid and stimulates blood circulation, will not harm.
If you have visual impairment, you should be constantly monitored by an ophthalmologist. If vitamin deficiency leads to a deterioration in twilight perception, then a routine examination will allow timely detection of pathological changes. The list of mandatory eye procedures also includes eye gymnastics, contrast showers, and accommodation training. These procedures not only solve the problem of night blindness, but also strengthen the eye muscles and inhibit the development of associated ophthalmological diseases.
Signs of hemeralopia
Symptoms of congenital hemeralopia develop in early childhood, characterized by persistent vision loss that cannot be cured. Night blindness is accompanied by a decrease in the acuity of twilight and night vision, and a feeling of visual discomfort even in twilight. Patients with hemeralopia note that they cannot distinguish between surrounding objects and lose spatial orientation in low light or when moving from a dark room to a well-lit one. At the same time, in the daytime, as well as with sufficient lighting, visual acuity is usually not impaired.
In addition, with hemeralopia, there may be a feeling of “sandiness” or dryness in the eyes. Children with hemeralopia are afraid of the dark, so they behave restlessly and often cry at dusk. This disease is characterized by a narrowing of visual fields with a decrease in the perception of yellow and blue colors.
Essential hemeralopia is accompanied by the appearance of xerotic Iskersky-Bitot plaques on the conjunctiva, which are flat dry spots that are located within the eye fissure. In addition to eye symptoms, there may be dryness of the mucous membranes and skin, and areas of hyperkeratosis may appear on the body, with peeling and scratching of the skin, and bleeding gums. With acute vitamin A deficiency, softening and ulceration of the cornea (keratomalacia) is often observed.
Symptoms
Night blindness occurs due to a lack of vitamin A, but the pathology may not be acquired, but hereditary. Symptoms then appear in infancy.
Children become restless, especially at dusk, and are very afraid of the dark. Children's field of vision narrows. Worst of all, they distinguish between yellow and blue. However, during the day, children see objects well at any distance and do not complain about their vision.
In other forms of nyctalopia, it may be indicated by:
- softening of the cornea, its ulceration;
- itching, dryness and flaking of the skin;
- bleeding gums;
- dry mucous membranes;
- feeling of sand appearing in the eyes.
With essential nyctalopia, dry patches appear on the conjunctiva. They are called Iskersky-Bito plaques. With nyctalopia, vision worsens in the evenings. A person cannot see objects (especially small ones) and cannot navigate in space. Red colors appear much darker and blue colors appear lighter.
How to see with night blindness (photo on the right)
This is the Purkinje effect, discovered in 1819. With nyctalopia, a person can write and read in the evening only in bright light. When moving from darkness to a well-lit room, spots appear in the eyes of a person. The ability to distinguish colors decreases.
Causes of night blindness
The immediate cause of night blindness is a decrease in the number of specific cells in the retina, which are responsible for the perception of images of the surrounding space in low light conditions.
It is known that the retina of the eye has two main types of light-sensitive cells, called rods and cones (see Figure 3). Rods are responsible for twilight vision, and cones, on the contrary, for vision in bright light conditions. Normally, there are many more rods on the retina than cones, since a person finds himself in low-light situations much more often than in conditions of ideal and bright lighting.
Normally, the retina of the eye contains approximately 115,000,000 rods and only 7,000,000 cones. The cause of night blindness is either a violation of the structure of the rods or a decrease in their number. Most often, the immediate cause of night blindness is the breakdown or disruption of the synthesis of the special visual pigment rhodopsin, which is the main functional unit of the rods. As a result, the rods lose their normal structure and cease to function fully, that is, the person develops night blindness.
The cause of congenital night blindness is a genetic mutation that is inherited. This mutation or breakdown in genes does not lead to the development of severe congenital deformities, but only causes night blindness - a disease with which a person can easily live. And since night blindness is a disease compatible with life, a fetus with such a defect in the genes is not “discarded” through spontaneous miscarriage, but continues to develop normally. Night blindness is often combined with other genetic diseases, such as Usher syndrome or hereditary retinitis pigmentosa.
The causes of symptomatic night blindness are various severe diseases associated with damage to the retina of the eyes:
- High myopia (myopia more than -6);
- Glaucoma;
- Pigmentary dystrophies of the retina;
- Chorioretinitis;
- Optic nerve atrophy;
- Siderosis (deposition of iron salts in the tissues of the eye).
Symptomatic night blindness is not an independent disease, but acts exclusively as a sign of another, more serious pathology of the retina.
Essential night blindness develops under the influence of various factors that cause deficiency or impaired absorption of vitamins A, PP and B2. These factors may include the following conditions or diseases:
- Poor nutrition, in which there is a deficiency of vitamins (A, PP and B2) and minerals;
- Starvation;
- Anemia;
- Past rubella or chickenpox;
- Liver diseases;
- Diseases of the digestive tract;
- Chronic alcohol abuse;
- Any poisoning (intoxication due to infections, poisoning, alcohol or tobacco abuse, etc.);
- Exhaustion of the body;
- Treatment with drugs that interfere with the absorption of vitamin A, for example, Quinine, etc.;
- Prolonged exposure to bright light.
Vitamin A deficiency is most important for the development of night blindness, since this compound is the substrate for the synthesis of visual pigment. Therefore, the risk of night blindness is highest in people suffering specifically from vitamin A deficiency.
However, essential night blindness does not develop immediately, since at least two years may pass from the onset of chronic vitamin A deficiency to the appearance of clinical symptoms. This is due to the fact that the reserves of vitamin A present in the tissues of the human body will last for about one year, provided that this compound does not come from the outside at all. However, in practice, there are no situations when vitamin A does not enter the human body at all, so reserves are depleted longer than a year and it takes at least two years for clinical manifestations of night blindness to form.
Description
Night blindness (nyctalopia, hemeralopia) is a disease in which vision is significantly reduced or completely lost in low light conditions. This happens because a person’s retinal ability to perceive light is impaired - the ability to perceive light of varying brightness, which is realized by retinal cells: rods and cones. There are many more rods on the retina than cones. The perception of light occurs as a result of a light wave hitting the membrane disk (the area of light-sensitive cells facing the pupil), which contains visual pigment, resulting in the formation of a nerve impulse. The rods contain the pigment rhodopsin, and the cones contain iodopsin. The rods are responsible for the perception of light levels, that is, twilight vision, and they also take some time to get used to. Cones contain several types of pigment, so they perceive different colors and instantly respond to changes in incoming information. Thus, impaired light perception may occur as a result of a decrease in the number of retinal rods, any changes in their structural organization, and due to a disruption in the formation of the light-sensitive pigment rhodopsin.
Medical designation of the disease night blindness and its synonyms
Night blindness is the popular name for the disease, which in the Russian terminological tradition is referred to as hemeralopia. In general, the term “hemeralopia” is formed from three Greek words – “hemer”, “ala” and “op”, which are translated into Russian as “day”, “blind” and “sight”, respectively. That is, the final translation of the term “hemeralopia” is “day blindness”. As you can see, the literal translation of the term does not reflect the essence of the disease, since with night blindness a person sees poorly in the dark, that is, at night and in the evening, and not during the day. However, this particular term in non-English-speaking countries, including the post-Soviet space, has been used to refer to poor vision in the dark for a long time (more than a hundred years), since a mistake was once made in the name of the disease and was subsequently not corrected. It is in this way, based on the “established” name, that the term “hemeralopia” has come to this day to designate a widely known disease - night blindness.
In English-speaking and many other countries, the medical term for night blindness is “nyctalopia.” The term "nyctalopia" is also derived from the three Greek words "nyct", "ala" and "op", which are translated as "night", "blind" and "sight", respectively. Accordingly, the final full translation of the term “nyctalopia” is “night blindness”. As you can see, nyctalopia fully corresponds to the essence and meaning of the disease, popularly called night blindness. However, this linguistically and functionally correct term is used to refer to night blindness only in English-speaking countries and former colonies of Great Britain.
Due to these features, night blindness is called hemeralopia in Russia, and nyctalopia abroad. Therefore, the terms “nyctalopia” and “hemeralopia” in the mouths of English-speaking and Russian-speaking doctors, respectively, will be synonyms, denoting the same disease, known by its popular name as night blindness.
Treatment
If the patient's condition is caused by a hereditary factor, it is impossible to prevent the development of the disease. He must learn to live with reduced visual acuity at dusk.
When a disease develops due to damage to the internal structures of the eyes, the underlying disease is treated. Conservative therapy is prescribed using drops to eliminate glaucoma and cataracts. If this is not enough, a surgical method is used.
If the disease is caused by a decrease in the intake of vitamins, it is recommended to adhere to the following diet:
- eating plant foods in the form of fruits, vegetables, herbs, berries;
- introduction of dairy products into the diet: cheese, sour cream, cottage cheese, milk;
- Chicken eggs are introduced into the diet several times a week, the yolk is especially useful;
- They eat different types of liver: chicken, beef, pork;
- introduce fish and seafood into the diet.
During illness, some patients complain of the formation of dry mucous membranes of the eyes. In this case, the doctor may prescribe medications that help preserve the tear film on the surface structures of the eyes.
Features of treatment
Treatment of night blindness requires a comprehensive approach. The doctor may prescribe the following measures:
- Diet. Adjust your diet. It contains foods high in vitamins A and D. The patient should eat a lot of dairy products, beef liver and fish, eggs, butter, vegetables and fruits.
- In the off-season, you need to take vitamin supplements. A complex of vitamins and minerals is prescribed by a doctor.
If the disease is congenital, then the treatment is different. In this case, the following may be recommended:
- Operation.
- Laser correction.
- Complex therapy of eye diseases that caused night blindness.
For congenital nyctalopia, a nutritionist recommends a balanced diet.
If necessary, vitamin A is prescribed. But it is worth considering that this vitamin is absorbed only with a normal amount of vitamin E in the body. It is best to eat fresh carrots seasoned with a small amount of vegetable oil.
If you are deficient in vitamin A, you should not take mineral oil as a laxative. In this case, retinol passes through the intestines and is not absorbed.
In case of secondary deficiency of vitamins, diet and retinol preparations are prescribed, but first it is important to find out and eliminate the cause of insufficient absorption of the drug
What vitamin deficiency causes night blindness?
A similar condition can occur not only due to a lack of vitamin A, but also with an insufficient amount of vitamin D. In this case, rickets develops. Most often, this disease is observed in premature and weakened children who were born in the autumn-winter period. Vitamin D is produced by the body as a result of synthesis under the influence of sunlight.
As a rule, in winter there is not enough sunlight, and the child’s skin is hidden under a layer of clothing. To compensate for the lack of this substance in the body, vitamin preparations are prescribed. Most often, Aquadetrim is prescribed to children to prevent rickets.
Therapeutic measures
Since night blindness develops due to a lack of vitamin A, one of the treatment methods is taking retinol acetate
A long-term lack of retinol can cause irreversible changes in the retina, so it is important to start therapy on time. Due to the fact that night blindness develops due to a lack of vitamin A, it is advisable to also take fats that enhance its absorption
Retinol preparations for external use are also prescribed.
Treatment of hemeralopia involves correction of visual stress. Additionally, vitamin drops with a moisturizing effect are prescribed. A solution of riboflavin improves tissue nutrition and normalizes the conduction of nerve impulses. Treatment for night blindness involves daily instillation of riboflavin in the morning and evening. The duration of therapy is determined by the ophthalmologist.
If night blindness develops due to a lack of vitamin, then treatment will bear fruit. But congenital hemeralopia is more difficult to overcome. How to treat night blindness in this case? Surgical treatment is recommended. Hemeralopia or night blindness is eliminated through keratoplasty, lens replacement, laser keratomileusis. After surgery, vitamin and adaptogenic eye drops are prescribed. The recovery period depends on the patient’s age and concomitant ophthalmological diseases.
Treatment of night blindness with traditional medicine methods makes sense only in the essential form. Herbal medicine can provide tangible results.
Hemeralopia or night blindness can be successfully treated with carrot juice. It contains a high concentration of vitamin A. Drink half a glass of juice daily in the morning and evening. To increase digestibility, add a little vegetable oil.
Blueberries, bell peppers, and red grapes are also used to treat night blindness. You should consume at least a glass of blueberries daily to improve visual acuity and get rid of problems with twilight perception.
Millet decoction can cure night blindness. Take two liters of water per glass of grains. Simmer on fire until completely softened. Strain and drink a third of a glass before each meal. Another effective remedy is nettle infusion. Take 2 tbsp per glass of boiling water. l. chopped herbs, bring to a boil and keep covered for at least 2 hours. Strain and drink a glass a day, dividing into 2-3 doses. Hemeralopia or night blindness does not recede immediately, but after a few weeks of such therapy improvements will be noticeable.
Classification and characteristics of types of night blindness
Depending on the causes of occurrence, all types of night blindness are divided into three types: 1.
Congenital night blindness;
2.
Essential night blindness;
3.
Symptomatic night blindness.
Congenital night blindness
It is inherited and manifests itself at an early age - in children or adolescents. The causes of congenital night blindness are often various genetic diseases, such as, for example, Usher syndrome or hereditary retinitis pigmentosa.
Essential night blindness
is a functional disorder of the retina caused by a deficiency of vitamins A, PP and B2 or the microelement zinc. The causes of essential night blindness are various conditions in which the intake or absorption of vitamins A, PP and B2 is impaired, for example, poor-quality poor nutrition, fasting, liver or digestive tract diseases, alcohol abuse, rubella, poisoning with any toxic substances or long-term exposure to bright light.
Symptomatic night blindness
develops against the background of various eye diseases associated with damage to the retina or optic nerve. In this case, night blindness is a symptom of the following severe eye lesions - high myopia, glaucoma, taperetinal dystrophy, chorioretinitis, optic nerve atrophy, siderosis.
In addition to the listed types of hemeralopia, doctors and scientists identify another condition called false night blindness
. In this case, a person’s vision is impaired and deteriorates in the dark and in low light conditions due to simple eye fatigue, for example, after working for a long time with computer monitors, televisions, locators or other devices, etc. False night blindness is not a disease, but reflects a functional deterioration in the functioning of the eye analyzer, resulting from its overstrain. After a person gives his eyes a good rest, his vision will be completely restored. However, if a person often strains his eyes excessively and does not give them quality rest, this can lead to serious illnesses and permanent vision loss.
Let's sum it up
Thus, hemeralopia can be congenital or acquired due to many reasons. The symptoms of this vision pathology also vary depending on the form of the disease.
The disease most often has a favorable prognosis and is treatable and correctable. Treatment largely depends on the causes of the pathology, severity, presence of concomitant disorders and diseases.
Treatment using surgical methods is considered especially effective. In all forms of hemeralopia, an important condition for correcting this vision pathology is the replenishment of essential vitamins (B2, A, PP) in the human body.
Other reasons for the development of pathology
The inability to see at dusk develops not only due to vitamin deficiency. Various diseases can also cause this pathology. The cause of visual impairment may be:
- Ophthalmic diseases that are associated with retinal detachment.
- Severe diseases of the liver and biliary tract.
- Low hemoglobin.
- Lack of a certain pigment in the tissues of the eye.
- Some genetic diseases.
- Oncological diseases of the brain.
The cause of deterioration in visual function may also be a plant called night blindness. This plant has small blue flowers and a slightly velvety stem. If the juice of such a flower gets on the mucous membrane of the eye, it becomes irritated and the person begins to see poorly in the dark.
In addition, metabolic disorders can also lead to a similar problem. This may be a consequence of poor nutrition or systemic diseases of internal organs.
Factors provoking hemeralopia
The disease is divided into several groups.
Essential blindness, which appears as a result of a lack of zinc and certain vitamins.
The problem is also caused by:
- unbalanced diet;
- addiction to alcohol and sweets;
- severe exhaustion;
- serious intoxication;
- inflammatory diseases of the stomach, biliary tract or kidneys;
- anemia;
- diabetes.
Symptomatic blindness is a consequence of the development of eye diseases, such as hypermetropia, glaucoma, cataracts, and others. Sometimes the problem is caused by treatment with retinol (vitamin A) antagonist drugs, one of which may be quinine.
Congenital blindness is a consequence of an abnormality in the formation and development of the retina, which occurs in Usher syndrome. Such night blindness develops from an early age and is hereditary.
Night blindness is sometimes caused by addiction to strict diets, severely limited in the choice of foods, and vegetarianism. Women's vision may decrease during menopause. Measles, herpes and even chickenpox also sometimes cause hemeralopia.
A disease that reduces visual acuity is sometimes defined by doctors as “false night blindness,” which develops when the visual organs are overworked. There is no need to treat such hemeralopia with medications: proper rest is enough for it to disappear on its own.
Treatment
Therapeutic tactics in the treatment of night blindness completely depend on the form of the pathological condition identified after diagnostic measures.
Medicines
The principles of treatment for congenital and essential forms of the disease are the same, but their effectiveness varies greatly. If congenital hemeralopia is practically incurable, causing a permanent decrease in vision, then in the essential form of the pathological condition, the lack of vitamins is easily compensated for by synthetic agents. In addition to vitamin therapy, a special diet of foods with a high content of essential vitamins (A, PP, B2) is recommended:
- Greens (parsley, dill, spinach, celery, young nettle);
- Leaf salad;
- Cod liver (take raw in small pieces);
- Egg yolk, cheese, butter, milk;
- Cabbage, tomatoes, carrots, green onions and green peas, corn;
- Blueberries, cherries, gooseberries, apricots, peaches, blackberries.
In addition, in order to eliminate unnecessary effects on photoreceptors, you should avoid bright lighting in any form, and also wear glasses in the evening if you have even mild myopia.
Surgically
For symptomatic hemeralopia, the main direction of treatment is the elimination of the underlying disease, which in some cases resolves using surgical methods:
- Refractive surgery: lens replacement, scleroplasty, etc.;
- Laser correction of myopia;
- Antiglaucomatous operations: trabeculectomy, trabeculotomy, iridectomy, cyclo-cryocoagulation;
- Phacoemulsification of cataracts;
- Laser coagulation for retinal detachment.
Folk remedies
The use of folk remedies is a necessary addition to the main treatment, as it helps restore the balance of essential substances in the body and, in particular, in the eye structures:
- Take fish oil in any form three times a day according to the regimen recommended by your doctor;
- All types of liver should be present in the diet in any form, even raw;
- Boil a large amount of liver and make an “inhalation” for the eyes, but the steam should not be too hot. A maximum of three such inhalations are required for treatment. Boiled liver must be eaten within 2 weeks;
- Introduce millet porridge into your diet, and consume it constantly;
- Mix dill and carrot juices (1: 5), drink 140-150 ml every morning;
- Grate carrots, 3 tbsp. l. cook in 1 liter of water or milk until tender, take 70 ml of filtered decoction at night;
- Take a mixture of equal portions of herbs (lingonberries, blackberries, primroses, viburnum, raspberries, lemon balm, snakeweed rhizome), brew 1 tsp. raw materials 1/3 liter of boiling water and leave for 60 minutes. Take the filtered infusion 100 ml three times a day;
- Make a rice broth (1 tablespoon of cereal per glass of water), take 70 ml at night.
Methods for diagnosing hemeralopia
Diagnosis of this disease begins with the collection of anamnestic data based on the patient’s characteristic complaints.
In order to make an accurate diagnosis, the following research methods are used:
- examination of the fundus by an ophthalmologist (this is a mandatory procedure, since in the presence of congenital and essential forms of hemeralopia, there are pathological changes in the fundus of a person, which provoked the onset of the disease);
- examination of the conjunctiva of the eye to determine the presence or absence of specific plaques;
- color and achromatic perimetry (detection of narrowing of visual fields);
- adaptometry (with this procedure, the patient is asked to look at a brightly lit screen of the device for 2-3 minutes, then a certain object is placed on the screen and the time after which the subject begins to see this object is noted; normally, a person should see the object no more than after 45 seconds after presentation, with hemeralopia the amount of time is more than 45 seconds);
- electroretinography (assessment of the functional state of the retina);
- biomicroscopy using a Goldmann lens;
- refractometry (detecting the refractive power of the eye using a refractometer, which allows you to quickly determine the presence of any refractive error).
The doctor can take other measures based on his experience and the complexity of the diagnosis.
You may find the following articles useful in preventing and combating hemeralopia:
- Vitamins for the prevention of eye diseases
- Pros and cons of laser vision correction
- In which Moscow clinics can hemeralopia and other diseases be treated?
Causes
The retina consists of two types of cells. These are rods and cones. It is the rods that are responsible for visibility in poor lighting conditions. Cones, in turn, are responsible for visual acuity and color recognition.
Night blindness is characterized by changes in the structure of both rods and cones.
Rods are formed from rhodopsin, which is produced with the participation of vitamin A. When light hits the retina, rhodopsin disintegrates, and regeneration in case of vitamin A deficiency takes a lot of time.
When the ratio of cones to rods changes, when there are significantly fewer cones, night blindness also develops. The essential type is the most common.
The reasons for its occurrence are as follows:
- Lack of vitamin A, P2 and PP.
- Liver diseases.
- Poor nutrition or problems with vitamin absorption.
- Anemia and exhaustion of the body.
- Long-term treatment with vitamin A antagonists.
The cause of congenital blindness is heredity and genetic diseases.
Symptomatic hemeralopia occurs for the following reasons:
- Eye diseases such as glaucoma, severe myopia.
- Retinal pigment pathologies.
- Retinal detachment.
- Diseases of the optic nerve.
- Inflammatory processes of the retina.
Regardless of the cause that causes night blindness, there is one common cause across all types. This is a violation of the production of rhodopsin in the retinal rods.
An exacerbation of hemeralopia, as a rule, occurs in the spring, when the body’s reserves of vitamin A run out.
There are cases when night blindness appears in an absolutely healthy person without any pathologies or eye diseases. Constant work at a computer in poor lighting conditions can cause vision deterioration. Because of this, the nerve endings in the eye become irritated and symptoms of hemeralopia appear.
To prevent such changes from happening, every hour of work at the computer should be accompanied by 30 minutes of rest. How to cure night blindness?
Night blindness is a vitamin disease. Vitamin A deficiency (“night blindness”)
Vitamin A deficiency (“night blindness”) is a visual disorder expressed in the inability to see in dim (twilight and night) lighting, photophobia, decreased color perception to blue and yellow colors, which occurs when there is a deficiency in the body, usually in early spring.
Night blindness, also called night blindness, is a disease associated with a disorder of human twilight vision. The origin of congenital night blindness is not yet fully understood.
Sometimes the disease is associated with anemia, exhaustion, pregnancy, and certain eye diseases (for example, glaucoma).
The occurrence of the disease is caused by a long-term lack of food or its provitamin - carotene; impaired absorption of carotene in the gastrointestinal tract; disorders of the liver's formation of carotene. The main manifestation of the disease, in addition to growth retardation, should be considered night blindness, as well as some changes in the eyes: dryness, inflammation of the eyelids, keratinization of the conjunctiva, etc. Pigment spots, rashes, etc. appear on the skin. The mucous membranes harden and dry out, which leads to the appearance of bronchitis, otitis media and other diseases. Patients lose their appetite, lose weight, and the acidity of gastric juice drops. The body becomes very sensitive to infections.
Symptoms and course:
In patients, the ability to navigate in space at dusk or in a dark room sharply decreases; in good lighting, the patient sees normally.
The main manifestation of the disease, in addition to growth retardation, should be considered night blindness, as well as some changes in the eyes: dryness, inflammation of the eyelids, keratinization of the conjunctiva, etc.
Pigment spots, rashes, etc. appear on the skin. The mucous membranes harden and dry out, which leads to the appearance of bronchitis, otitis media and other diseases.
Patients lose their appetite, lose weight, and the acidity of gastric juice drops.
The body becomes very sensitive to infections.
In this state, a person’s visual acuity and associated orientation in space during the twilight period noticeably decrease. Characteristic is:
- decreased light sensitivity;
- worse adaptation in the dark;
- a noticeable change in the electroretinogram;
- narrowing of the field of view;
- predominantly;
- for various colors.
The seriousness of this disease is also confirmed by the fact that a medical certificate for the right to drive a car with night blindness found in the driver is not issued.
When making diagnoses, doctors, in addition to the patient’s complaints, are also guided by the results of a study of human dark adaptation.
Recognition:
Based on clinical findings and contrastometry.
Treatment:
If the cause of the disease is poor nutrition, then “night blindness” goes away quickly with intake or by eating food rich in it (animal and cod liver, fresh fruits, vegetables, especially carrots). Since it belongs to the group of fat-soluble substances, sour cream and butter are recommended.
When a decrease in twilight vision is caused by other reasons - damage to the retina or eye (high myopia, retinal degeneration, etc.), then the underlying disease is treated
Congenital (night blindness) cannot be treated. Moreover, with this disease, vision gradually deteriorates.
With essential night blindness, a diet that includes foods containing the contents found in butter, cod liver, cheese, milk, egg yolk, provitamin A, which is rich in spinach, carrots, lettuce, green peas, tomatoes, blackberries, black currants, helps. gooseberries, peach, cherry, apricots, fish. Additionally, you should take riboflamin in a daily dose of approximately 0.02 grams per day. By the way, even with symptomatic night blindness, these products will not be superfluous at all, and can have a beneficial effect.
At the beginning of treatment for this disease, doctors try to find the cause of the disease, to somehow determine what the body lacks. An examination is carried out to determine the level of carotene in the blood. If the concentration of these vitamins is low, appropriate treatment is prescribed. You may also need examinations from other specialists.
It is known for sure that self-treatment of night blindness is absolutely pointless, with the possible exception of the diet suggested above. By the way, millet is useful here.
With essential blindness, the prognosis is usually favorable, but with symptomatic blindness, one can only hope for a positive completion of treatment.