Causes of cortical blindness and its symptoms
The causes of the disease can be partial or complete damage to the back of the head, visual radiation, as well as hypoxia (a pathological condition characterized by oxygen starvation of individual organs and tissues or the body as a whole) and anoxia (lack of oxygen in the body or in individual organs, tissues, blood) , causing temporary loss of vision. The disease can develop as a secondary clinical symptom in injuries, malignant hypertension (hypertension), toxemia (poisoning of the body caused by the presence of toxins in the blood, coming from outside or formed in the body itself) in pregnant women and other diseases.
Cortical blindness can also occur after severe stress or trauma.
When the first symptoms of the disease appear, we recommend getting diagnosed. An ophthalmologist must take into account the symptoms that help diagnose the disease:
- Certain areas of images disappear from view
- A veil appears before the eyes, cloudiness
- Complaints about poor coordination of movements
- Difficulty directing your gaze to objects in the periphery
- The pupillary reaction to light is preserved, but when a ray of light hits the eyelids reflexively do not close
- With a congenital disease, speech is impaired.
Tests to detect blindness in children
— To identify one reason or another, it is necessary to collect data about the child, mother and father, as well as about hereditary diseases, how the pregnancy proceeded, at what time the child was born, and anthropometric data of the child. — Assess the child’s ability to fix his gaze — Assess the reaction of the pupils to light, their symmetry — Determine the degree of refraction after cycloplegia — It is imperative to consult a neurologist — If the child has neurological symptoms, CT and MRI of the brain are prescribed.
You may be interested in Iritis of the eye (inflammation of the iris)
Types of cortical blindness
Cortical or cerebral blindness is a secondary pathology. To date, very few cases with congenital pathology have been registered. Ophthalmologists distinguish the following forms of the disease:
- Permanent cortical blindness
caused by irreversible damage to brain structures, for example, after a hemorrhagic stroke (acute cerebrovascular accident with vascular rupture and hemorrhage in the brain. Is the most severe brain catastrophe) - Paroxysmal cortical blindness
is a reversible phenomenon. It is observed most often in children and is associated with metabolic disorders (metabolic disorder).
Causes of congenital blindness
Congenital blindness in a child can have both obvious causes, which entail structural changes in the eyes, and latent, that is, hidden, without visible structural changes. Let's take a look and break them down a little.
— Aniridia is a developmental defect in the color structure of the eye, which can be congenital or acquired. This malformation, diagnosed at birth, is much more common than acquired one.
— Congenital cataract is a very common congenital disease. The diagnosis of congenital cataract is made in more than 50% of cases. Among all eye pathologies diagnosed at birth, this pathology is the most common. It is characterized by both unilateral development (in one eye) and bilateral development (in both eyes); in addition, it can develop in parallel with another eye pathology.
— Retinopathy of prematurity is a congenital malformation in which the development of the retina is disrupted due to the influence of various factors, including: premature birth, mechanical ventilation (artificial ventilation), oxygen dependence, exposure to infections during fetal development, general immaturity.
— Optic nerve hypoplasia is most often a congenital developmental defect than an acquired one, in which the size of the optic nerve head is small as a result of underdevelopment of nerve fibers. Causes include FGR (fetal growth restriction syndrome), hormonal deficiency during pregnancy, consumption of alcohol and tobacco, drugs in the first three months of pregnancy, certain specific drugs, such as steroids, and cold medications in the subsequent months of pregnancy. Optic nerve hypoplasia can be unilateral, bilateral, or isolated. It often occurs together with strabismus; bilateral hypoplasia is in some cases combined with Morsier syndrome.
You may be interested in Farsightedness: causes, symptoms, diagnosis, treatment
— Congenital atrophy of the optic nerves - occurs when the fibers of the optic nerve are completely or partially destroyed, followed by replacement of their connective tissue. The cause of congenital optic nerve atrophy is hereditary and genetic in nature; Leber's disease is most common. I distinguish between primary and secondary optic atrophy. In children, congenital optic atrophy is rare.
- Congenital impairment of twilight vision - has a hereditary-genetic nature of development. With this pathology, the adaptation of the eyes to conditions with poor lighting (twilight, darkness, artificial darkening) is disrupted. Very often observed in Usher syndrome, hereditary retinitis pigmentosa and other inherited pathologies. Symptoms of this disease are noticeable at an early age; there is a narrowing of the visual fields and decreased vision. Decreased vision with this pathology cannot be treated. Children with this pathology are afraid of the dark, so they often scream and cry.
— Achromatopsia is a congenital pathology characterized by a complete lack of color perception. The disease has two forms: rod monochromasy and cone monochromasy. With rod monochromasia, there are no cones, so a person sees the whole world in gray, but with cone monochromasia, the world is perceived only in one shade of color.
— Severe refractive errors – myopia, hypermetropia, astigmatism.
Some doubts
It is important to note several limitations, not least the long-standing adage that absence of evidence is not evidence of absence. What we mean is that these numbers alone do not prove that cortical blindness is the key factor in eliminating schizophrenia.
The authors also note that their data only covers people aged 14 to 35 years; in some cases, schizophrenia may be diagnosed later.
However, given how the study fits with previous case studies, these relationships appear worthy of future study.
Causes
The causes of blindness are related to the social and technical development of society.
In the most developed countries, the cause of blindness can be complications from a number of diseases, such as traumatic injuries to the cornea, diabetes, and macular degeneration. In less developed countries, blindness is more common. Its reasons are:
- cataract;
- infections;
- glaucoma;
- various injuries;
- inability to use glasses.
In underdeveloped countries, the causes of the disease may be river blindness, leprosy, trachoma, etc.
Cortical blindness has become a defense
In particular, cortical blindness, caused by abnormalities in the brain rather than damage to the eyes, seems inconsistent with the presence of schizophrenia.
According to the authors of this latest study, no cases of schizophrenia have yet been reported in cortically blind people.
The researchers analyzed data from 467,945 children born in Western Australia between 1980 and 2001. In this sample, 1870 children (0.4%) developed schizophrenia, but none of the 66 children in the sample who were born with cortical blindness received a diagnosis of schizophrenia.
“The protective phenomenon observed in case studies of people with congenital cortical blindness and now confirmed by our data in the entire population requires rigorous clinical investigation,” say researchers from the University of Western Australia.
"Children need happy parents." Natalie Nevedrova named the reason for the divorce
A woman designed her bathroom in Japanese style. Now I want to repeat
This narrow house seems inconspicuous only from the outside, once you look inside
What makes the findings particularly noteworthy, aside from the large sample size, is their potential to tell us more about how schizophrenia works and how it can be better treated in the future.
Blindness in both eyes in an infant - examination, treatment
Children's medical ophthalmology / To help parents. Diseases and their treatment / Blindness in both eyes in an infant - examination, treatment
OBJECTIVE SYMPTOMS
Searching, incoherent eye movements begin at approximately 1 month of age. Poor pupillary response to light in children >31 weeks gestational age. is a key feature. Inability to fixate or follow large, bright objects after 4 months of age.
ETIOLOGY (CAUSES) IDENTIFIED DURING OPHTHALMOLOGICAL EXAMINATION
• Severe eye disease or malformation.
• Retinopathy of prematurity . See Retinopathy of Prematurity. • Dense cataracts in both eyes in children >8 weeks of age. See Congenital cataract. • Aniridia and other severe malformations (dysgenesis) of the anterior segment . See Developmental anomalies/dysgenesis of the anterior segment and lens. • Optic nerve hypoplasia . Small optic discs are sometimes difficult to identify if such discs are present in both eyes. The “double ring” sign is diagnostically significant (pigmented ring along the inner and outer edges of the peripapillary scleral ring), if present. If changes are present in only one eye, strabismus, a relative afferent pupillary defect, and poor fixation in one eye may be detected instead of “searching” nystagmus. Hypoplasia is usually idiopathic. Bilateral optic nerve hypoplasia in some cases is combined with septo-optic dysplasia (de Morsier syndrome). On the contrary, unilateral optic nerve hypoplasia is only very rarely combined with this syndrome. De Morsier syndrome includes changes in the midline structures of the brain, as well as a deficiency of growth hormone, thyroid-stimulating hormone and other trophic hormones. Growth retardation, seizures (as a result of hypoglycemia) and diabetes insipidus may develop. If there is bilateral optic nerve hypoplasia, MRI is performed with special attention to the hypothalamic-pituitary region. • Shaken baby syndrome . Multilayer retinal hemorrhages, often in combination with subdural/subarachnoid hemorrhage.
ETIOLOGY IN THE ABSENCE OF VISIBLE CHANGES IN EYE STRUCTURES
• Congenital stationary twilight vision disorder . Visual acuity may be close to normal, nystagmus is less common and is accompanied by myopia. The electroretinogram is pathological. There are autosomal dominant, recessive and X-linked forms. Paradoxical pupillary reactions (ie, constriction of the pupil in low light conditions after exposure to bright light) often occur. • Achromatopsia (rod monochromasia) . Visual acuity is about 0.1. Severe photophobia. The pupils react normally to light, but pupillary responses may be paradoxical in the dark. The fundus is normal, but the photopic electroretinogram is significantly abnormal. Lack of response to flicker stimulation (stimulation with flashes of light) (25 Hz) allows a diagnosis to be made. Scotopic electroretinogram is normal. • Albinism with foveal hypoplasia . During transillumination, iris defects are visible. See Albinism. Differential diagnosis of signs of blindness Diffuse brain dysfunction. Infants do not respond to sound or touch and have neurological impairments. Visual acuity may improve slowly over time. • Delayed formation of the visual system . Normal reaction to sound and touch, no neurological pathology. The electroretinogram is normal and visual function usually returns to normal by the age of 4 to 12 months. It is more common in patients with some type of albinism (nystagmus may be detected upon examination). • Extremely severe refractive error . Diagnosed with cycloplegia. • Infantile idiopathic nystagmus . Patients with this disease have a slight decrease in vision (visual acuity of about 0.33 or better). The iris is normal. May be accompanied by head turning, nodding, or both.
• Congenital atrophy of the optic nerves. Rarely seen. A pale, normal-sized disc is often associated with mental retardation or cerebral palsy. Electroretinogram is normal. It can be autosomal recessive in inheritance or sporadic.
• Leber's congenital amaurosis . Rod-cone lesion. At first, the fundus may appear normal, but eye examination in childhood reveals narrowing of the retinal blood vessels, pallor of the optic disc, and pigmentation abnormalities. The electroretinogram is noticeably abnormal or flat, which helps establish the diagnosis. Autosomal recessive inheritance.
SURVEY
1. History. Prematurity? Normal development and growth? Maternal infection, diabetes, or taking medications during pregnancy? Seizures and other neurological disorders? Family history of eye diseases? 2. Assess the infant's ability to fixate and follow an object. 3. Study of pupillary reactions, assessment of their symmetry and speed. 4. Look carefully for nystagmus. 5. Inspection of the anterior segment using a flashlight; Check especially carefully for transillumination defects during slit-lamp examination. 6. Examination of the retina and optic nerve with a wide pupil. 7. Determination of refraction in conditions of cycloplegia. 8. ERG, especially if there is a suspicion of Leber congenital amaurosis. 9. Consider CT or MRI of the brain only in cases of other focal neurological symptoms, seizures, poor weight gain, developmental delay, optic nerve hypoplasia, optic nerve atrophy, or neurologically localized nystagmus (eg, reciprocating, vertical, with paresis of gaze, vestibular). If unilateral or bilateral optic atrophy is present, perform an MRI to identify optic glioma or chiasm and craniopharyngioma. 10. Solve the question of studying visual evoked reactions to assess visual potentials. 11. Consider recording eye movements to assess nystagmus waveforms, if possible.
TREATMENT OF BLINDNESS IN BOTH EYES IN INFANTS
1. Correction of refractive error and treatment of established or suspected amblyopia. 2. A conversation with parents is necessary for all of the listed diseases, taking into account the visual potential of the baby, the likelihood of vision problems in brothers and sisters, etc. 3. Referral to educational services for the visually impaired or blind may help. 4. Provide genetic counseling. 5. If neurological and endocrine disorders are detected or suspected, the child should be referred to a pediatrician for appropriate examination and treatment.
Source: https://zrenue.com/
Night blindness
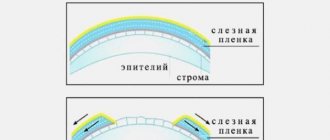
Night blindness (night blindness or nyctalopia) is a disease in which blindness occurs in low light conditions. Normally, a person is able to see in twilight color. A person suffering from night blindness has characteristic symptoms - the inability to see at dusk (night blindness). The disease occurs due to dysfunction of the eye rods or a decrease in their number.{banner_gorizontalnyy}
The disease night blindness can be congenital or acquired. Congenital night blindness is extremely rare. The causes of congenital night blindness are unknown.
One of the causes of acquired night blindness is a lack of vitamin A in the body. Vitamin A is part of rhodopsin, a special protein found in rods. When exposed to light, rhodopsin is broken down. Depending on which rods received the light stimulus, the primary image is formed.
In daylight, patients with night blindness see through cones. At night, only the sticks work, which are defective in patients with nyctalopia. Therefore, only twilight vision suffers, hence the second name - night blindness.
If the cause of the disease is vitamin A deficiency, then the disease can be cured. The largest amount of vitamin A is found in chicken liver, fish, and carrots. The daily intake is 800-900 mcg per day.
There are situations when, with sufficient consumption of foods containing vitamin A, night blindness still occurs. The reason lies in an unbalanced diet. The fact is that vitamin A is fat-soluble and fat is needed to break it down and enter the body. Otherwise, vitamin A transits through the intestinal tract and is excreted along with feces. Therefore, it is necessary to eat carrots with sour cream, butter or vegetable oil.
Blindness in child development
OBJECTIVE SYMPTOMS
Searching, incoherent eye movements begin at approximately 1 month of age. Poor pupillary response to light in children >31 weeks gestational age. is a key feature. Inability to fixate or follow large, bright objects after 4 months of age.
ETIOLOGY (CAUSES) IDENTIFIED DURING OPHTHALMOLOGICAL EXAMINATION
• Severe eye disease or malformation.
• Retinopathy of prematurity . See Retinopathy of Prematurity. • Dense cataracts in both eyes in children >8 weeks of age. See Congenital cataract. • Aniridia and other severe malformations (dysgenesis) of the anterior segment . See Developmental anomalies/dysgenesis of the anterior segment and lens. • Optic nerve hypoplasia . Small optic discs are sometimes difficult to identify if such discs are present in both eyes. The “double ring” sign is diagnostically significant (pigmented ring along the inner and outer edges of the peripapillary scleral ring), if present. If changes are present in only one eye, strabismus, a relative afferent pupillary defect, and poor fixation in one eye may be detected instead of “searching” nystagmus. Hypoplasia is usually idiopathic. Bilateral optic nerve hypoplasia in some cases is combined with septo-optic dysplasia (de Morsier syndrome). On the contrary, unilateral optic nerve hypoplasia is only very rarely combined with this syndrome. De Morsier syndrome includes changes in the midline structures of the brain, as well as a deficiency of growth hormone, thyroid-stimulating hormone and other trophic hormones. Growth retardation, seizures (as a result of hypoglycemia) and diabetes insipidus may develop. If there is bilateral optic nerve hypoplasia, MRI is performed with special attention to the hypothalamic-pituitary region. • Shaken baby syndrome . Multilayer retinal hemorrhages, often in combination with subdural/subarachnoid hemorrhage.
Treatment
In most cases, vision problems occur in older people (an exception is hereditary blindness). But nowadays there are already many diagnostic methods that can at an early stage identify diseases that can lead to blindness. It is necessary to undergo regular examinations with an ophthalmologist in order to identify the disease at an early stage and begin its treatment. In 90% of cases, blindness can be prevented through a combination of education and access to health care. Blindness due to injury can be prevented by providing instructions on eye protection for various types of work. Food blindness can be prevented through proper nutrition. Blindness due to glaucoma or cataracts can be prevented with early diagnosis and treatment of the disease. The prognosis for blindness also directly depends on the cause of its occurrence. If this disease develops as a result of damage to the optic nerve or a stroke, then basically vision is not restored after this. If a patient has a retinal detachment, vision can be improved through surgical correction. Patients with cataracts or scarring have an excellent chance of restoring their vision if they undergo surgery on time. There is no cure for complete blindness to this day. In case of irreversible loss of vision (total blindness), it is necessary to create the most comfortable conditions for life and development for the patient. For this purpose, such auxiliary measures are used as guide dogs (helping the blind to navigate the area), books and programs in Braille, computers equipped with a keyboard in Braille and other devices. Also developed, but not yet widely used, are devices for the blind such as the “Bionic Eye” (electronic visual system), “Electrosonar”, etc.
Blindness
Blindness refers to a severe degree of visual impairment. Blindness is a disease characterized by a complete absence of vision or its significant reduction. With blindness, visual perception becomes impossible or limited, which is due to a significant narrowing of the visual field, with a decrease in the acuity of central vision.
It is customary to distinguish between total (absolute) and practical blindness.
Total blindness is a condition in which there is absolutely no visual sensation in both eyes. Practical blindness is characterized by residual vision, as well as preserved color and light perception.
Why does a person go blind?
Sudden blindness does not occur in people with a completely healthy body. This pathology is a consequence of the presence of diseases and conditions such as:
- Diabetic retinopathy;
- Degeneration of the optic spot;
- Glaucoma;
- Cataract;
- Onchocerciasis;
- Trachoma;
- Keratomalacia and xerophthalmia;
- Injury.
Congenital blindness depends on intrauterine diseases or fetal malformations.
The first place in the statistics of the causes of acquired blindness is glaucoma, the second is trachoma, and the third is eye injuries. Cases of blindness from diseases of the cornea, optic nerve and retina are observed less frequently.
Most often, vision loss occurs before the age of 10 years and over 50 years. This is explained by the fact that children are diagnosed with congenital blindness and there is loss of vision from eye and general diseases common in childhood, as well as eye injuries. In people over 50 years of age, the causes of blindness are glaucoma and vascular diseases.
Symptoms
People who have no visual sensations are considered blind. At the same time, they may have light perception and residual vision in the eye, which sees better within 0.01 - 0.05D with correction by glasses or contact lenses.
People with blindness cannot perceive the color, shape, size of objects and their location in space. Therefore, it is difficult for them to navigate in space, and the formation of movements is delayed. At the same time, blind people have an enhanced orienting reaction to sound.
Vision loss can be sudden or gradual if the cause is a medical condition.
Diagnostics
To determine whether vision is completely absent, to identify the width of the visual fields, as well as color vision, and whether it is possible to correct the problem with the help of lenses, glasses, or surgery, it is necessary to undergo a detailed examination at an ophthalmology center.
If acquired vision loss is suspected, it is necessary to establish the localization of the pathological focus (ophthalmological examination - biomicroscopy, ophthalmoscopy). In some forms of retinal pathology, decreased vision may appear even before the manifestation of morphological changes in the retina. If optic nerve atrophy is suspected, especially asymmetric or unilateral, a CT or MRI of the brain is required.
Can blindness be cured?
Some types of total blindness are reversible. In particular, vision lost due to cataracts, inflammatory and infectious diseases is restored after treatment of the underlying disease. For acute vision loss (for example, retinal detachment), surgical or laser treatment is possible.
Treatment depends on the cause of blindness. If the cause is a dysfunction of the optic nerve, or the lack of vision is caused by a cerebral hemorrhage, it is usually not possible to restore vision. The patient needs psychological help and learning to move without vision control.
A modern achievement in the treatment of blindness is the artificial visual system “bionic eye”.