Hello, dear readers. In the article I will talk about glaucoma of the 2nd degree, the development of this disease and symptoms, which will allow the patient to monitor the condition of his eyes, promptly seek medical help and carry out preventive measures.
People often do not pay attention to the deterioration of central vision, color perception and distortion of the outlines of objects. And these are the first signs of vision deterioration, which may result in its loss.
In the initial stage, the disease is quite difficult to diagnose, but grade 2 glaucoma shows itself with clear manifestations, so it is easier to recognize it. At this stage, the disease responds well to treatment and there is a guarantee of vision restoration.
What is glaucoma?
Many people have heard about the eye disease glaucoma, but they don’t know exactly what it is. Meanwhile, glaucoma is called one of the dangerous eye diseases from which you can lose your sight.
Ophthalmologists say that almost 3% of the population is susceptible to the disease. The likelihood of getting sick increases after 40 years, and by the age of 50-60, second-degree glaucoma develops.
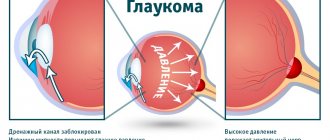
Glaucoma is considered a chronic disease. At the initial stage, intraocular pressure periodically increases, the outflow of intraocular fluid is disrupted, there are problems in the functioning of the retina, and damage to the optic nerve occurs. As a result, visual defects appear.
The disease can be in open-angle and closed-angle forms. The open form begins unnoticed and the patient does not experience discomfort in the initial stages. In the second form, which is rare, the disease progresses quickly and is difficult to treat.
Causes of open angle glaucoma
Predisposing factors such as myopia, inflammation, and farsightedness can provoke the appearance of this disease. But this is always a whole complex of interconnected pathological conditions, which together give rise to a disease such as open-angle glaucoma. The main causes and risk factors for the development of glaucoma:
- Age – by the age of 40, many chronic diseases accumulate in the body, and the structure of tissues changes. If a person also has bad habits, the risk of developing glaucoma increases several times. The deterioration of blood circulation and tissue trophism occurs gradually, and at a certain point an acute period of eye disease begins.
- Compression of the optic nerve by neoplasms, hematoma after injury. When compression occurs for a long time, the functional ability of the nerve is impaired and it dies.
- Dysfunction of the outflow of ocular fluid - this disorder underlies the development of the disease, as it provokes increased intraocular pressure. The accumulation of fluid due to blockage of the canal or another cause leads to the acute onset of glaucoma.
- Dystrophic processes in the eye - disruption of the nutrition of the optic nerve and structures, tissue ischemia, breakdown of fibers trigger the mechanism of destruction of the eye and blindness occurs against the background of acute-angle glaucoma, and in this case treatment is ineffective.
- Hypoxia and circulatory failure are associated factors of the disorder.
As the disease develops, the optic nerve gradually atrophies and part of it is in a passive state, that is, it does not take part in functional processes. In this case, it is still possible to completely restore vision by activating the nerve endings.
Advice! The primary disease manifests itself mainly at the stage of nerve death, when vision begins to deteriorate more and more. This is a dangerous period, and in a short time the function of eye movement can completely stop. Early identification of symptoms and effective prevention of complications is a chance to restore vision using medications and surgical treatment, but it will not be possible to return the eye to its previous condition.
Laser treatment
Source: BeregiZrenie.ru Any eye surgeon uses a laser to clear and create a hole in the eye.
Thus, the process of fluid leakage is easier, and eye pressure decreases. Laser treatment can be performed in an eye doctor's office or at an outpatient surgery center. Laser vision correction is performed only after drug reduction of IOP.
Has a varied character. In one case, a laser is used to create a hole for better movement of fluid inside the chambers of the eye, which helps reduce pressure.
This type of operation is used to eliminate angle-closure glaucoma, after first reducing the pressure with medications. Another type of laser intervention is the removal of blockages in drainage channels, which restores the outflow of fluid.
The operation lasts about 20 minutes, but to get the full effect you will have to wait several weeks.
Main causes of the disease
Medicine considers jumps in intraocular pressure to be the main cause of glaucoma. The change in pressure lies in the imbalance in the formation and outflow of intraocular fluid.
Provoking factors are age-related changes, heredity, the development of myopia, neurological diseases, thyroid dysfunction, low blood pressure and diabetes.
Important! Eye diseases such as cataracts, iridocyclitis, and retinitis can also cause glaucoma.
Often the causes of the disease are associated with stress, addictions, eye injuries or taking certain medications.
Prognosis and prevention
Despite the fact that even modern treatment methods cannot get rid of glaucoma forever, therapy helps preserve vision and ensure a comfortable life for the patient. Even if glaucoma is not accompanied by severe symptoms, treatment cannot be refused, because the pathology is constantly progressing and at a late stage of development leads to irreversible blindness.
Risk factors:
- age from 40 years;
- presence of glaucoma in relatives;
- refractive errors;
- diabetes;
- presence of pseudoexfoliation;
- long-term therapy with corticosteroids (treatment of bronchial asthma, autoimmune diseases);
- disruptions in the central circulation (hypertension or hypotension, myocardial infarction, vegetative-vascular dystonia, cerebrovascular accidents);
- disruptions in local and regional blood circulation (vascular spasms, migraines, narrowing of the lumen of the carotid artery);
- thyroid disease.
The presence of each risk factor increases the likelihood of developing glaucoma. If there are several warning signs at once, it is recommended to visit the ophthalmologist more often and respond to all symptoms. In the early stages of glaucoma, the prognosis is usually favorable. A person can carry out life activities and work in almost any position.
Prevention of glaucoma in people without a predisposition comes down to undergoing an examination every six months. Patients with an established diagnosis must register with a dispensary and visit a doctor every 2-3 months.
Open-angle glaucoma is a very dangerous disease that does not always produce pronounced symptoms, but without treatment leads to disability in a matter of years. Therefore, it is so important to regularly visit an ophthalmologist and monitor the condition of your visual system, especially when you reach 40 years of age. You should not wait for the first manifestations of glaucoma; it is better to start treatment on time and ensure a comfortable life.
Who is diagnosed?
The average statistical norm for measuring eye pressure with a Maklakov tonometer is 23 mm Hg. If the ophthalmotonus exceeds this indicator, the patient may be suspected of glaucoma.
If a patient has signs of glaucoma, he is registered and special treatment is prescribed. If a patient's IOP exceeds the average, but there are no signs of the disease, he is classified as a patient with essential hypertension.
Useful video
Early diagnosis of glaucoma: mechanical and computer perimetry, tonometry:
Symptoms of second degree glaucoma
Clinical signs are:
- tearfulness;
- veils before the eyes upon awakening;
- vision becomes worse in the dark;
- there is a feeling of heaviness in the eyes.
These signs are the first signal that you need to immediately visit an ophthalmologist.
Open-angle glaucoma at the first stage does not give obvious signs of vision deterioration.
The symptoms of the second stage are more obvious - the patient feels a deterioration in vision: periodically a veil or flickering dots appear before the eyes; Fatigue quickly sets in under high load - when writing, reading, working in front of a monitor; from the side of the nose the field of vision narrows; the affected eyeball enlarges, pain and pain appear.
At the second stage, it is easier to diagnose the disease, but the risk of unpleasant consequences is higher.
Acute attack of angle-closure glaucoma
An acute attack is dangerous because it leads to irreversible consequences. If signs of this condition appear, you should immediately contact a medical specialist.
Characteristic symptoms:
- Severe pain, which is localized in the area of the visual apparatus. At the same time, unpleasant sensations radiate to the temples.
- Pain syndrome near the brow ridges.
- Sudden deterioration of vision.
- Increasing pain in the head, which is difficult to get rid of with medications.
Various provoking factors lead to this condition. Among them are nervous shock, severe hypothermia, increased physical activity, and abuse of liquids. There are other reasons that provoke the problem. For example, an attack begins with the uncontrolled use of medications that can affect the eyes and blood vessels. Also, if you stay in a dark room for a long time, an acute stage may occur.
https://youtube.com/watch?v=Af4vwapkgi4
Differential diagnosis of glaucoma
It is possible to determine whether a person has glaucoma using instrumental ophthalmological diagnostic methods. Differential diagnosis is carried out for two diseases: an attack of acute glaucoma and iridocyclitis.
It is important to understand that with iridocyclitis, the symptoms are similar to those of an acute attack of glaucoma, but the treatment is completely different. Therefore, the main thing in this case is to make a correct diagnosis so that complications do not develop.
So, what does the differential diagnosis of these two diseases show? Let's look at the comparison table:
| Symptom of the disease | Acute attack of glaucoma | Iridocyclitis |
| Eye injection (dilated vessels) | Congestive in nature, all eye vessels are significantly dilated. | Pericorneal (inflammation of the cornea, redness of the eye), in severe cases a purple color appears. It may be accompanied by irritation of the conjunctival vessels, in which case the injection is mixed. |
| Cornea | Cloudy, the surface is not transparent, usually matte | The cornea has a smooth appearance, the surface is shiny |
| Corneal sensitivity | Below normal | Fine |
| Anterior chamber size | Decreased | Fine |
| Iris | edematous | There is no swelling, there is a change in color and a smoothed relief |
| Pupil changes | Pupil dilated | The pupil is constricted |
| Presence of headaches | Available, radiates to the forehead and back of the head | Not available |
| Intraocular pressure | Increases greatly | Remains within normal limits, in some cases decreases |
| General complaints | Nausea, vomiting | Pain in the eye area |
How is diagnosis carried out?
Obviously, the earlier the diagnosis is made, the more optimistic the prognosis for recovery and restoration of visual function will be. Diagnostics includes the following procedures:
- IOP (intraocular pressure) is measured;
- the pupils are dilated with the help of medications and the shape and color of the optic nerve is assessed;
- the field of view along the perimeter is determined;
- the angle between the cornea and the iris is measured;
- the thickness of the corneal layer is determined (pachymetry method); the thickness of neuronal cells is determined.
First of all, the doctor measures the pressure inside the eye and examines the fundus, then, if necessary, the following tests are prescribed.
Diagnostic methods are:
- 24-hour tonometry monitoring. Significant fluctuations in intraocular pressure during the day indicate the disease;
- Perimetry and campimetry. Allows to identify central and paracentral scotomas and the presence of narrowings in the field of view;
- examination of the fundus using an ophthalmoscope and biomicroscopic studies allow us to track how the fundus of the eye is changing.
In the second stage of the disease, significant pressure surges, changes in the fundus of the eye are observed, and there are shifts in the vascular bundles of the optic nerves.
You may be interested in: Tonography of the eye for glaucoma - the essence of the method and analysis of the results
Manifestation
It should be said that there is a triad of symptoms characteristic of glaucoma of any form:
- Increased or fluctuating intraocular pressure (IOP);
- Formation of atrophy of the optic nerve, as well as excavation of its disc (glaucomatous optic neuropathy);
- Pathology of visual fields in the form of their narrowing.
These symptoms are taken into account when determining the stage of glaucoma. Here is their brief description:
- Stage I (initial) – visual fields are normal; minor changes occur in the paracentral parts (scotomas, expansion of the blind spot). Expansion of the excavation of the optic nerve head (OND). As a rule, a person does not yet experience any discomfort.
- Stage II (developed) – pronounced change in visual fields in the paracentral part. Narrowing of the visual field by 10° or more in the superior and/or inferior nasal segment. Excavation of the optic disc reaches its edge.
- Stage III (far advanced) – the field of vision narrows on the nasal side to 15° or less from the point of fixation. Subtotal marginal excavation of the optic disc.
- Stage IV (terminal)—total loss of visual function or light perception with incorrect light projection. It is possible to preserve an island of visual field in the temporal part. Total excavation of the optic disc.
The first signs of the disease noticeable to humans appear only at stage II of the disease (see photo). The most characteristic is a gradual narrowing of the visual fields.
Open angle shape
It occurs more often in people over 35 years of age and is usually asymptomatic, with a gradual increase in IOP and a painless decrease in vision.
Rarely, with POH, complaints of iridescent halos when looking at light, asthenopia (easy eye fatigue) and “fogging” before the eyes may appear.
Tonometry reveals an increase in IOP to 40-60 mm Hg.
Biomicroscopy reveals changes in the conjunctiva and episclera - a violation of the caliber of blood vessels (narrowed arterioles, dilated venules).
Small hemorrhages, “granular” blood flow, and funnel-shaped dilated anterior ciliary arteries at the entrance to the emissary (“cobra symptom”) occur. The phenomena of necrosis of the iris stroma develop.
Ophthalmoscopy reveals a defect in the layer of nerve fibers: its thinning and smoothness in the peripapillary zone, atrophy with excavation and hemorrhages on the optic disc.
When examining visual fields, paracentral scotomas are revealed, expansion of the blind spot zone, visual fields are narrowed mainly in the nasal quadrants.
Primary closed-angle
The highest incidence of occurrence occurs at the age of 60-70 years, but it can appear at any age. More often, PAOG develops in women and in hypermetropic eyes, which is associated with a smaller anterior chamber.
Often manifests itself in attacks. There are acute and subacute attacks of PAOG.
Acute attack of gastrointestinal tract
As a rule, PAH manifests itself in this variant after the action of provoking factors. In most cases, one eye is affected, but the process can also be bilateral.
The following symptoms appear:
- Sudden sharp pain in the eye and the same half of the head of a bursting nature with irradiation to the frontal, temporal, zygomatic areas (along the trigeminal nerve);
- Severe visual impairment (“foggy” or decreased until it disappears completely)
- The appearance of rainbow halos when looking at light sources;
- With a pronounced attack - bradycardia, nausea, vomiting.
When examining the eye, corneal edema, dilation of the episcleral vessels, a shallow anterior chamber, protrusion of the iris, mydriasis are noted, and there is no reaction of the pupil to light. In addition, IOP was sharply increased - 50 mm Hg. and more. Gonioscopy reveals a blocked anterior chamber angle.
Subacute attack of PAOG
Quite a rare occurrence. It causes slight visual impairment and the appearance of rainbow circles when looking at light sources.
During the examination:
- Minor eye injection;
- Mild swelling of the cornea;
- Mild mydriasis;
- IOP not higher than 35 mm Hg;
- Gonioscopy of the anterior chamber reveals a blocked angle.
The subacute attack passes without any consequences. In this case, vascular strangulation, atrophic and necrotic processes in the iris do not occur.
And in this video you will find the answer to the question “can glaucoma occur without increased intraocular pressure?”
Perimetry: determination of visual fields
To identify defects in the visual fields, the instrumental perimetry method is used.
The picture visible to the human eye has its own boundaries. In this case, the field of view can be divided into two groups:
- Central vision is what we see in the center when the head is in a static position.
- Peripheral vision is what we see to the sides.
There are different types of perimetry, the main ones are:
- Isopperimetry involves studying the boundaries of the visual field using different volumes of objects.
- campimetry, which is used to determine disturbances in the central field of vision.
- kinetic perimetry – used to study the peripheral visual field. The method is based on photosensitivity.
- static perimetry – based on the perception of light fluxes in different fields of view.
Defects in visual fields with glaucoma, depending on the stage (up to complete loss of vision)