Definition of disease
Fuchs syndrome, also known as heterochromic Fuchs cyclitis, is a gradually developing chronic anterior non-granulomatous uveitis, that is, inflammation of the choroid. In young people, the problem most often affects only one eye; in children, the pathology is also diagnosed and is rarely bilateral. Heterochromia may be present, but it is often absent or simply difficult to detect, especially in patients with brown eyes.
The disease occurs in approximately 4% of all uveitis sufferers, but it is very often misdiagnosed. To avoid this, you need to carry out diagnostics only with a dilated pupil and in daylight.
Treatment in Italy
Russian Medical Server / Treatment in Italy / Center for the treatment of rare diseases in Milan / Fuchs’ heterochromic iridocyclitis - treatment in Italy
Iridocyclitis is an inflammation of the choroid of the anterior part of the eyeball; in essence, iridocyclitis is anterior uveitis. Most often, the disease develops in active working age (20–40 years) and has a chronic relapsing course.
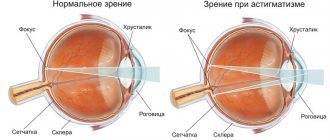
Let us recall that the anterior section of the choroid of the eye includes the iris and ciliary body, inflammation of the iris is called iritis, and the inflammatory process in the area of the ciliary (ciliary) body is called cyclitis. Due to the close location and the presence of a common blood supply network, isolated inflammation of any one of the structures of the choroid of the anterior part of the eye is practically not observed, and usually we are talking about combined inflammation, i.e. about iridocyclitis.
The inflammatory process in iridocyclitis is usually one-sided. The severity of the symptoms of the disease depends on the cause of the disease, as well as on the state of the patient’s immune system. The first signs of iridocyclitis are usually pain of varying intensity; patients also complain of blurred vision (the appearance of a “veil” before the eyes). In acute iridocyclitis, the pain increases quite quickly and can become unbearable. Swelling of the iris causes constriction of the pupil, and photophobia appears.
A characteristic sign of iridocyclitis is increased pain when pressing on the eyeball. The visible vessels of the mucous membrane of the eye are dilated, the color of the iris due to inflammation may become red, rusty or greenish, while the pattern of the iris is smoothed out, details are not distinguishable.
Very often (in about 70% of cases) iridocyclitis takes a chronic, relapsing course. In this case, the symptoms of the disease are less pronounced, complications often arise, the most common of which are adhesions (synechias). With iridocyclitis, adhesions usually affect the area of the pupil, it narrows and becomes deformed. The extreme manifestation of this process is complete occlusion of the pupil and a high risk of vision loss due to the development of obscuration amblyopia.
The causes of iridocyclitis are diverse and can be endogenous or exogenous. Often, iridocyclitis develops as a result of traumatic injury to the eye (wound, contusion, ophthalmic surgery), inflammation of the iris (keratitis). Iridocyclitis can be caused by previous viral, bacterial or protozoal diseases (influenza, measles, HSV, staphylococcal and streptococcal infections, tuberculosis, gonorrhea, chlamydia, toxoplasmosis, malaria, etc.), as well as existing foci of chronic infection in the nasopharynx and oral cavity (sinusitis, tonsillitis).
The cause of iridocyclitis can be rheumatoid conditions (rheumatism, Still's disease, autoimmune thyroiditis, ankylosing spondylitis, Reiter's and Sjögren's syndromes), metabolic disorders (gout, diabetes), systemic diseases of unknown etiology (sarcoidosis, Behçet's disease, Vogt-Koyanagi-Harada syndrome). The prevalence of iridocyclitis among patients with rheumatic and infectious diseases is about 40% of cases.
The occurrence of iridocyclitis is facilitated by the developed vascular network of the eye and the increased susceptibility of the iris and ciliary body to antigens and CECs coming from extraocular foci of infection or non-infectious sources of sensitization.
With the development of iridocyclitis, in addition to direct damage to the choroid by microbes or their toxins, immunological damage occurs with the participation of inflammatory mediators. Inflammation is accompanied by phenomena of immune cytolysis, vasculopathies, dysfermentosis, microcirculation disorders with subsequent scarring and dystrophy.
Of no small importance in the development of iridocyclitis are provoking factors - endocrine and immune disorders, stressful situations, hypothermia, excessive physical activity.
Fuchs' heterochromic iridocyclitis is usually (but not always) a unilateral, chronic, recurrent, practically asymptomatic anterior uveitis in young patients, often complicated by the development of cataracts and glaucoma (75 and 15%, respectively).
The pathogenetic basis of Fuchs' iridocyclitis is an immune reaction involving CD8+ T cells caused by chronic infection with the rubella virus.
The most common complaint is a progressive change in the color of the iris, which occurs in 70% of patients. The initially dark iris becomes lighter due to stromal atrophy. Blue eyes, on the contrary, darken due to the pigment epithelium beginning to shine through the atrophied stroma.
Heterochromia is absent in 6% of patients with bilateral lesions, and then atrophy of the iris stroma acquires special diagnostic value. Other complaints include a slight decrease in visual acuity, floaters, and discomfort in the eye. Pain and pericorneal injection are rare with this pathology. A characteristic, but not obligatory, finding is multiple small, stellate precipitates on the endothelium of the lower third of the cornea, forming the triangle of Arlt. During gonioscopy, newly formed vessels are visualized.
Laboratory diagnostics consists of determining antibodies to the rubella virus in chamber fluid (specificity 100%), oligocponal IgG (sensitivity 87%), as well as the modified Goldmann-Witmer index (antibody level index to the rubella virus antigen exceeding 40, in combination with characteristic symptoms is very informative).
Differential diagnosis should be carried out with other causes of acute anterior uveitis (HSV, herpes zoster virus, toxoplasmosis, Kraup-Posner-Schlossmann glaucomocyclic crisis) and heterochromia.
Local use of glucocorticoids with minimal inflammation, characteristic of Fuchs iridocyclitis, has no obvious indications, since with a slight effect on the underlying autoimmune process, hormonal therapy accelerates the appearance of cataracts and glaucoma. In this regard, careful dynamic monitoring of patients, aggressive therapy (and often surgery) for secondary glaucoma, and also, if indicated, phacoemulsification with perioperative local and systemic hormonal therapy and vitrectomy, seem more justified. The prognosis for vision is favorable even in cases of long-term inflammation.
! Despite the fact that many of the diseases described in this section are considered incurable, the Center for the Treatment of Rare Diseases in Milan is constantly looking for new methods. Thanks to gene therapy, it has been possible to achieve outstanding results and completely cure some rare syndromes.
Contact a consultant on the website or leave a request - this way you can find out what methods Italian doctors offer. Perhaps this disease has already been treated in Milan.
+7 (925) 50 254 50 – urgent treatment in Italy
REQUEST TO THE CLINIC
Symptoms
The key symptom of this syndrome is iris heterochromia . This is manifested, among other things, in the fact that the iris of the affected eyeball looks lighter.
In contrast, patients with light eyes may exhibit reverse heterochromia.
As the problem develops, other symptoms may appear, in particular, blurred vision, formations on the front of the iris (the so-called Russell bodies), pigmentation disorders, and more.
Differential diagnosis
Pigmentary glaucoma must be distinguished from other types of ocular hypertension:
- Primary open-angle glaucoma is sometimes accompanied by hyperpigmentation, but the pigment is concentrated in the lower sector of the angle. Patients are also usually older, and characteristic transillumination defects in the iris and Krukenberg spindle cannot be identified.
- In pseudoexfoliation glaucoma, pigment may be deposited in trabeculae, but transillumination defects are found in the iris at the edge of the pupil rather than at the periphery. Patients are usually over 60 years old. In addition, in half the cases this type of glaucoma is unilateral and does not lead to the development of myopia.
- In pseudophakia, pigmentary glaucoma can also occur, which is associated with contact of the intraocular lens (haptic and optical parts) in the posterior chamber of the eye with the posterior surface of the iris. As a result, pigment dispersion occurs and aqueous humor circulation is disrupted.
- With anterior uveitis, hyperpigmentation in the trabecular zone and iris atrophy may occur. A collection of pigmented old precipitates is sometimes falsely mistaken for Krukenberg's spindle upon examination.
- Subacute angle-closure glaucoma in some cases is associated with significant pigmentation of the trabecular region as a result of contact of the iris and the structures of the angle of the anterior chamber of the eye.
Possible complications
- If uveitis develops against the background of Fuchs syndrome, then there is a high probability that it will become chronic. Also, if treatment with corticosteroid hormones is not rational enough, cataracts or glaucoma may occur, which, in turn, may have their own complications.
- Glaucoma usually follows a long-term illness - and if it develops particularly negatively, it can lead to loss of vision.
- Cataracts can complicate the course of the disease. The situation will improve after surgery, but the risk of developing hyphema cannot be ruled out.
- Mydriasis or permanently dilated pupils develop due to atrophy of the corneal muscles.
Symptoms of pathology
Mydriasis may occur in the affected eye.
- Change in eye color. The right one is darker than the left one and vice versa. This is caused by a greater or lesser accumulation of pigment or the germination of the iris by vessels.
- Cataract. Against the background of decreased trophism of the eye structures, secondary cataracts develop, accompanied by a rapid decrease in visual acuity.
- "Floating" opacities. They appear due to the presence of fibrin fibers and other metabolic products in the vitreous body.
- Mydriaz. This is a persistent dilation of the pupil. It appears as a compensatory reaction to decreased visual acuity. The dilated pupil tries to let more light into the retina.
- Increased intraocular pressure. It is accompanied by the appearance of rainbow circles around the light sources that the person is looking at.
Diagnosis and treatment
The following methods are used to diagnose Fuchs syndrome:
- Visometry or determination of visual acuity.
- Tonometry or measurement of intraocular pressure.
- Ophthalmoscopy.
- Biomicroscopy.
- Ultrasound of the eyeball.
Carrying out Biomicroscopy
There are several approaches to treating this symptom, some of them rely on the use of the right medications , while others may rely on surgery.
Treatment with folk remedies for this type of syndrome is unacceptable; it is important to resort only to effective and proven methods of official medicine.
By medication
Drug treatment occurs mainly through the injection of long-acting drugs into the posterior sub-Tenon's space , which helps to cope with vitreous opacification. Medicines are prescribed exclusively by the attending physician.
Prednisolone is a steroid drug
The use of local steroids is usually ineffective. Also, due to the fact that posterior synechiae are formed extremely rarely, mydriatics are usually not prescribed.
Surgically
If the effectiveness of the use of steroid drugs is low, if no effect occurs, the vitreous body is too cloudy and still remains cloudy, despite all the effects, then a so-called vitrectomy is performed , in which either partial or complete removal of the vitreous body is performed.
Performing vitrectomy
This procedure is a last resort; if possible, the doctor will try to avoid its implementation.
Consequences of the disease
As a result of a long and severe course of the disease, a number of complications develop:
If the optic nerve does not receive normal nutrition for a long time, the person becomes blind.
- Cataract. Persistent clouding of the lens with disruption of all visual functions, which occurs when the trophism of this light-refracting structure deteriorates.
- Glaucoma. Manifested by increased intraocular pressure. The symptoms of glaucoma are varied, first of all, these are rainbow circles around the lights.
- Amaurosis. Complete blindness, which occurs as a result of long-term lack of blood supply to the optic nerve and other eye structures.
Prevention
No specific prevention for this disease has been developed at the moment, since there is still no understanding of the exact causes of its occurrence and development.
However, since hypothetically this disease can develop against the background of other inflammatory processes that occur in the body, it will not be superfluous to monitor your general health and try to overcome any painful processes that develop in the body.
Main symptoms of the disease
The course of the disease can be either latent - without pronounced clinical manifestations, or accompanied by vivid symptoms. The main symptoms that are characteristic of EED:
- blurry, cloudy vision, especially in the morning;
- various visual distortions;
- excessive photosensitivity;
- reduced visual acuity in the dark, halos around light sources;
- discomfort in the eyes - a feeling of “like sand being poured in”, a sensation of a foreign body;
- formation of blisters on the cornea due to fluid accumulation;
- corneal opacities;
- loss of vision (a symptom of a late stage).
EED may manifest itself in different combinations of the listed symptoms in different patients; you should consult a doctor for an accurate diagnosis.
Treatment
The strategy for the prevention and treatment of Fuchs syndrome is determined depending on the stage of the disease and the severity of secondary complications. At the first stages, specific therapy is not carried out. Color correction occurs when using cosmetic colored lenses. But already in later stages of the disease, local and systemic therapy is recommended, aimed at correcting trophic processes.
The complex for treating Fuchs syndrome includes angioprotectors, nootropics, vasodilators and vitamins. In the case of the formation of a significant number of precipitates, the course of treatment procedures should be expanded with corticosteroids for topical use in the form of drops and enzyme therapy.
Drug treatment
When a secondary posterior subcapsular cataract forms in the initial stages of the development of Fuchs syndrome, drug therapy is recommended. If there is no result, microsurgical intervention is practiced, which involves fragmentation of the lens nucleus with the simultaneous installation of an intraocular lens implant. The appearance of secondary glaucoma is regarded as a sign of the need for local antihypertensive therapy simultaneously with the main course of treatment of the disease.