Intraocular pressure indicators have a significant impact on the overall health of a person. Untimely diagnosis of ophthalmotonus is the beginning of the path to the emergence and progression of glaucoma, which entails a complete loss of the ability to see.
Monitoring intraocular pressure indicators is a mandatory procedure for people over the age of 40. We will reveal what dangers fraught with IOP deviations, diagnostic methods and the meaning of ophthalmotonus indicators, and the corresponding norms.
IOP what is it?
Intraocular pressure is the pressure of the fluid of the eyeball on the walls of the eye. The role of ophthalmotonus is determined by maintaining the shape and anatomical features of the eye, maintaining stable blood flow in the tissues.
IOP values that are normal range from 10 to 25 mmHg. They fluctuate in different directions throughout the day. The greatest peak occurs at the beginning of the morning, since towards the end of the day the eyes need to rest from the stress received.
Warning symptoms of increased IOP
Increased eye pressure may not show any particular signs of trouble for a long time. A person continues to live in a normal rhythm, unaware of the impending danger, because real symptoms of a pathological eye condition appear only when the IOP changes significantly towards an increase. And here are some signs of illness that may suggest that, putting everything aside, you need to immediately visit an ophthalmologist to check your vision and measure intraocular pressure:
- Pain in the eyes, in the eyebrow area, in the frontal and temporal areas (or on one side of the head);
- “Fog” before the eyes;
- Multi-colored circles when looking at a burning lamp or lantern;
- Feeling of heaviness, fullness and tiredness of the eyes at the end of the day;
- Attacks of unmotivated lacrimation;
- Change in corneal color (redness);
- Decreased visual acuity, lack of image clarity (with glaucoma, patients often change glasses).
An increase in IOP and the development of glaucoma can be suspected if a person often changes glasses because he begins to be unable to see in the “old” ones, and also if this disease was diagnosed in close relatives.
What dangers do IOP disorders pose?
| A value of ophthalmotonus that does not correspond to the norm, with out-of-date diagnosis and treatment, can provoke a complete loss of the ability to see. |
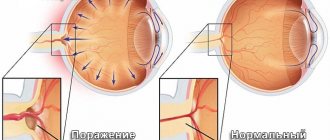
Elevated IOP values lead to the death of cells responsible for light sensitivity, resulting in a stable decrease in the quality of vision.
If the nerve is compressed, the supply of oxygen and nutrients will be disrupted. The result will be atrophy of the optic nerve and loss of quality of vision. The consequences may be irreversible.
Underestimated IOP values will be the result of circulatory disorders in the visual system, leading to atrophy of eye tissue. Ultimately, the patient may become completely blind.
At the initial stages of development of the consequences of deviations from the norm in intraocular pressure indicators, there is practically no discomfort felt, however, a belated visit to an ophthalmologist in most cases leaves no chance of returning full vision.
When to contact an ophthalmologist for an IOP check?
It is mandatory to conduct a study of intraocular pressure indicators in the presence of diseases:
- Neurology;
- Diabetes mellitus;
- Vegetative-vascular dystonia;
- Glaucoma.
In addition, determination of ophthalmotonus indicators is necessary in the presence of factors:
- Dry eye condition;
- Stable visual impairment;
- Violation of the shape and structure of the pupil and eyeball;
- Pain in the head and eyes;
- Fatigue of the visual system in a short period of time;
- Clouding or redness of the eye.
| It should be remembered that the procedure is contraindicated when under the influence of drugs or alcohol, in the presence of psychiatric disorders, or infectious diseases of the visual organs. |
Increased intraocular pressure
Increased eye pressure (ophthalmohypertension) is not necessarily the result of age-related changes, as many people think.
The reasons for increased IOP can be very diverse, for example:
- Constant tension on the organs of vision, leading to fatigue;
- Atherosclerosis;
- Persistent arterial hypertension (periodic surges in blood pressure, as a rule, are not dangerous for the eyes);
- Vegetative-vascular dystonia;
- Psycho-emotional stress, chronic stress;
- Fluid retention in the body due to cardiovascular pathology;
- Intracranial hypertension often causes increased fundus pressure;
- Professional activities (wind musicians);
- Individual (strength) physical exercises;
- Medicines used locally;
- Strong tea or coffee (due to caffeine);
- Heart rhythm disturbances, respiratory arrhythmia;
- Features of the anatomical structure of the eye;
- Intoxication;
- An inflammatory process localized in the organ of vision;
- Diencephalic pathology;
- Traumatic brain injuries;
- Diabetes;
- Menopause;
- Hereditary pathology;
- Side effects of certain medications, treatment with corticosteroid hormones.
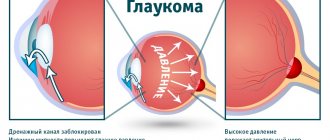
Increased intraocular pressure is often a sign of glaucoma, the risk of developing which increases markedly after 40 years.
IOP and its types
Ophthalmologists distinguish three degrees of IOP:
- Normal;
- Increased;
- Decreased.
Indicators that do not cause concern for an adult patient range from 18-30 mmHg. Daily fluctuations in IOP are around 2-3 mmHg. do not cause concern among doctors, since IOP has its highest peak at the beginning of daylight hours.
Factors influencing elevated intraocular pressure are hereditary pathology, excessive fluid content in the eye capsule, age-related changes, disorders of the genitourinary system, unstable outflow of fluid inside the eye, and glaucoma.
Glaucoma can be triggered by:
- Vegetative-vascular dystonia;
- Chronic stressful condition;
- Problems with the kidneys, heart and blood vessels;
- Inflammation of the organs of vision;
- Excessive strain on the eyes;
- TBI.
Inflated indicators of ophthalmotonus are also divided into:
- Stable (permanent);
- Labile (periodic);
- Transient (episodic).
Most often, the deviation is a consequence of pathological development of the eye, injuries to the apple of the eye, or surgical intervention.
Reasons for low IOP also include:
- Dehydration;
- Liver and kidney problems;
- Shock;
- Blood loss;
- Retinal disinsertion.
Return to contents
Symptoms of high IOP
An increase in intraocular pressure occurs due to a violation of the outflow of fluid inside the eye and increased production of ocular secretion. This causes deformation of blood vessels and optic nerve atrophy. Glaucoma is always asymptomatic at first, but as the pathology develops, the following symptoms begin to appear:
- feeling of pain;
- hyperemia of the eye shell;
- feeling of discomfort;
- blurred image;
- pain in the area of the eyes, eyebrows, temples;
- fatigue, heaviness in the eyes in the evening;
- light halos when looking at the light;
- decreased visual acuity;
- poor visibility at night;
- decreasing viewing angle.
With glaucoma accompanied by increased IOP, the patient quickly gets tired and complains of discomfort in the eyes even after a short period of work at the computer. Sometimes there are sudden attacks of tearing.
Palping method for measuring IOP indicators
Palpation of the apple of the eye provides a rough assessment of the IOP condition. The technique is widely used in cases of injury to the organs of vision and after surgery, when it is impossible to obtain measurements using instrumental methods.
Determining IOP indicators using fingers assumes a sitting position of the patient with drooping eyelids. The doctor, having fixed his hands on the frontal part of the patient's head, presses on the apple of the eye with his index fingers, thereby determining the level of sclera density.
Stable IOP readings within normal limits suggest the sensation of small impulses. The hardness and density of the eyeball indicates increased IOP, and its softness indicates decreased IOP.
| The palpation method is used at home because it does not require special skills. |
Methods for contact measurement of IOP indicators
The methods involve the impact of devices on the cornea of the eye to determine the state of IOP. Contact measurement methods are very unpleasant and often require instillation of painkillers. The disadvantage of such methods may be the likelihood of infection through the device.
Maklakov method
It is used in the presence of inflammatory eye diseases and after surgery. The procedure involves the use of anesthesia, as discomfort may occur.
The measuring device consists of several metal cylinders weighing 10 grams. The patient is placed on a horizontal surface. Weights are placed on the open eyelids, previously soaked in a special solution of pigment dye.
When the weight is pressed, the applied composition is imprinted on the apple. The weight is imprinted on a white sheet of paper. The final stage of the procedures is instillation of the eye with a disinfectant, which prevents the risk of infection.
Indicators are determined using a measuring ruler. The diameter of the print shows how much paint is left after placing the weight on the patient's eye. The larger the residue of the substance on the eyelid, the lower the IOP.
Currently, a portable device has been developed for conducting research using the Maklakov method. It is a ballpoint pen that applies pressure to the closed eyelid.
Goldmann tonometer
A slit lamp is used for research. Before starting the procedure, the patient needs to drip the eyes with anesthetic drugs, and also inject a special dye solution.
The device is brought to the cornea until it makes full contact. By squeezing the cornea, the device divides the presented image into two half-rings. Impact regulation occurs while the half-rings form a single whole. The scale determines the IOP indicator.
Schiotz and his method of measuring ophthalmotonus
The technique was developed for diagnosing the condition of IOP in the adult population. The procedure requires pre-treatment of the eyelid with anesthetic drops. A weight is applied to the apple of the eye, the pressure of which is prevented from being pressed. As a result, the needle of the measuring device moves to the side on the scale by which the IOP value is judged.
Dynamic measurement of IOP indicators
Dynamic contour tonometry is a contact technique for determining the state of ophthalmotonus, excluding the effect on the corneal membrane. The essence of the measurement involves applying the tip of the device to the apple of the eye. Thanks to the pressure sensor located inside the tip, measuring the indicators takes about 10 seconds. and is saved on the device’s memory card.
| The advantage of this technique is the simultaneous diagnosis of multiple indicators in one procedure, which makes it possible to determine the IOP status with high accuracy. |
Pneumotonometry
Contact method for diagnosing IOP indicators, determined by compressing air masses in the apparatus. The measuring device consists of a hollow tube and a slit lamp.
With the help of the device, an air flow is supplied, providing blood supply to the eye. An indicator of ophthalmotonus is the value of the ocular pulse.
| The measuring method is very painful and requires preliminary administration of an anesthetic drug. |
Tono-Pen
The technique involves diagnosing the condition of the apple of the eye using a portable device. The study is unpleasant and involves the administration of painkillers.
The measurement is taken by touching the tip of the instrument to the cornea of the eye. The study values are instantly displayed on the device display.
Rebound tonometry
The method is effective for diagnosing a number of ophthalmological diseases in the primary stages of development. The procedure is carried out without the use of painkillers. Involves disposable use of tips. The measuring device is located 3-10 mm from the center of the eye.
When the device is turned on, the probe moves at lightning speed to the cornea of the eye and then bounces off it. The speed of the device is directly dependent on IOP indicators.
Return to contents
Measuring IOP using non-contact methods
Non-contact diagnosis of ophthalmotonus is less accurate. The technique is used to study the intraocular globe in children and patients with diseases of the cornea.
| Diagnostic methods do not cause discomfort and do not have the risk of infection. |
Air flow
Measuring intraocular pressure using airflow devices is a popular way to diagnose IOP and examine the apple of the eye. The method involves the following steps:
- The patient concentrates his gaze on a point;
- The device delivers air flow to the center of the cornea;
- Depending on the degree of deformation, the IOP indicator is determined.
The device is able to easily detect elevated IOP values, whereas with low intraocular pressure, the measurements are not so accurate.
Optical coherence tomography
The method makes it possible to examine the condition of eye tissue and diagnose pathologies at an early stage. Measuring procedures using an infrared beam, which the doctor directs at the patient's fixed gaze.
Due to the projection of infrared radiation on the shell, a picture is formed, from which the doctor judges the condition of the IOP.
The measuring technique can detect glaucoma, visual nerve atrophy and other dangerous ophthalmological diseases in the early stages.
Portable devices
Portable tonometers are very effective when the patient needs to constantly monitor the pressure inside the eye. It is worth highlighting the ICare device, equipped with disposable sensors that are applied to the cornea for a moment and provide very accurate indicators of the IOP condition.
| The measuring method is absolutely painless and has no risk of infection. |
Reichert device for determining ophthalmotonus indicators
The Eye Response Analyzer measures the degree of flattening of the cornea. The device reflects two indicators of corneal hysteresis. This method of diagnosing IOP allows you to obtain information about the state of elasticity of the apple of the eye.
Transpalpebral tonometry
Non-contact method for studying the state of IOP through a lowered eye. Tonometry is performed using a Diaton apparatus. The device is designed to quickly determine IOP.
Advantages of the technique:
- Lack of contact with the cornea of the eye;
- Infection is excluded;
- No painkillers;
- Does not entail complications;
- It is performed in any position of the patient.
Electrotonograph
The device is used to diagnose glaucoma in the early stages of its development. The measurement takes 5 minutes by placing the device's sensor on the cornea of the eye. The device displays indicators of changes in IOP in a graphical form, and the final result is calculated by a computer.
Return to contents
Measuring intraocular pressure
It should be noted that not all people referred for annual preventive examinations to an ophthalmologist are enthusiastic about the upcoming measurement of intraocular pressure. Women may be afraid of ruining carefully applied makeup; men will refer to the absence of any complaints about their own organs of vision. Meanwhile, measuring intraocular pressure is a mandatory procedure for people who have turned 40 or older, even if they assure the doctor that they are in perfect health.
Measuring intraocular pressure is carried out using special equipment and instruments, and in general, modern ophthalmology uses 3 main types of measuring intraocular pressure:
tonometry according to Maklakov
The above-mentioned method according to Maklakov - many patients remember it, know it and most of all dislike it, since drops are dropped into the eyes, providing local anesthesia, and “weights” are installed (for a very short time), which are quickly removed and lowered onto a clean sheet paper to leave imprints indicating the IOP value. This method is more than 100 years old, but it still has not lost its relevance;- Pneumotonometry, very similar to Maklakov tonometry, but different in that it uses an air jet. Unfortunately, this study is not particularly accurate;
- Electron diffraction is the most modern method, successfully replacing the previous two. It is used mainly in specialized institutions (not all clinics can yet afford expensive ophthalmological equipment). The method is classified as non-contact, highly accurate and safe research.
Most often in the Russian Federation and neighboring countries, Maklakov tonometry or non-contact tonometry using an electronograph are used.
What is the norm?
Stable IOP values, which do not cause concern, do not exceed 23 mmHg. The average value varies between 14–16 mmHg, increased IOP starts from 33 mmHg. When the IOP value is from 10 to 13 and from 23 to 33 mmHg. do not indicate the presence of a disease, but observation by an eye specialist is still recommended.
The value of ophthalmotonus varies by 2-6 mmHg. at the beginning of daylight and the cold period.
| IOP values invariably increase with patient age. |
For children from 1 to 12 years old, the value of ophthalmotonus increases from 6 to 12 mmHg. People over 40 experience an increase in IOP values by an average of 1 mmHg. in 10 years.
Applanation tonometry
When measuring blood pressure using the instrumental method, the doctor expresses the values in millimeters of mercury. The Maklakov tonometry technique has been used in domestic ophthalmology for more than a hundred years (since 1884).
This technique is based on the ability of the cornea to flatten (applanate). This method is quite simple and relatively accurate. To perform tonometry according to Maklakov, a set of tonometers of different weights is used (a weight of 10 g is most often used). The tonometer itself looks like a hollow metal cylinder with a lead base inside. At the ends of the tonometer there are smooth, well-polished plates made of frosted glass.
The diameter of the plates is 1 cm. They are usually treated with alcohol, and then a coloring agent is applied to the surface, which consists of 50 drops of glycerin and distilled water, 3 g of collargol. Instead of collargol, you can use Bismarck-brown.
To apply paint, use a stamp pad, which is also included in the tonometer set. To remove excess paint, use a dry, sterile cotton swab. After applying the anesthetic solution (0.5% dicaine), the examination begins after 3-5 minutes.
The patient takes a horizontal position, face up. The doctor sits at the head of the room. The subject should extend his arm up in front of him and look at the index finger. It is necessary to ensure that the cornea is located strictly in a horizontal plane. After this, the doctor with his left hand spreads the patient’s eyelids and presses them to the bony edges of the orbital sockets. The doctor takes the tonometer in his right hand, which he lowers strictly vertically onto the central zone of the cornea. At this time, the holder disconnects from the tonometer and slides along the cylinder. Under the influence of the load, the cornea is flattened.
In the area of contact between the tonometer and the cornea, the surface of the latter is colored with the substance.
In this study, there is an important relationship: the more pronounced the intraocular hypertension, the less pliable the eyeball. That is, there is less applanation of the cornea, a smaller area of contact with the tonometer, and a smaller diameter of the white disk on the matte disk of the tonometer.
After this, the intraocular pressure measurement is repeated on the same eyeball, changing the direction of the tonometer (the unused glass disk should be at the bottom, and the print should be at the top). Next, the tonometer is put back into the case, and another weight weighing 10 g, which is prepared for tonometry of the second eye, is taken with a special handle.
After the procedure is completed, all devices are placed in a case.
Typically, tonometry is performed first on the right eye and then on the left. After measuring the pressure level, preventive disinfection of the surface of the eyeball is performed using special drops.
The prints obtained during the study are transferred to paper. To do this, it is moistened with an alcohol swab and the tonometer pads are printed on paper one by one. It is important not to touch the tonometer platform with your hands, so the tonometer should only be held by the cylinder. The remaining dye is removed from the tonometer pads using a cotton swab. The received prints are signed (patient's name, time and number of measurements, etc.). using a Polyak ruler, which is graduated in mmHg. Art., measure indicators.
The white print must fit into the diverging lines of the scale. The pressure level is obtained on a line that corresponds to 10 g. The normal value for this technique is from 18 to 27 mm Hg. Daily pressure fluctuations within 3-5 mmHg are allowed, with morning readings usually being higher.
If the patient suffers from glaucoma, then the readings and daily pressure fluctuations will be higher. In order to clarify the diagnosis, the doctor prescribes daily tonometry, during which blood pressure is measured in the morning and evening.