Measuring intraocular pressure is a diagnostic procedure that allows you to assess the degree of pressure of intraocular fluid on the inner membranes of the eye. This indicator is very important and informative for an ophthalmologist. Based on this, we can conclude that glaucoma is present. Ocular tonometry also monitors the effectiveness of treatment for this disease or determines how well the visual system is recovering after surgery. Let's find out how to correctly measure intraocular pressure, and who needs this procedure regularly?
Why is ophthalmotonus dangerous?
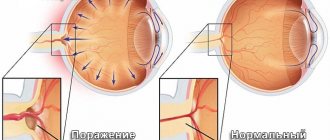
Excessively high or low internal ocular pressure (IOP), or ophthalmotonus, is a vision-threatening symptom. With high IOP, the capillaries of the fundus are compressed, certain areas of the retina are injured, and at this point the light-sensitive cells may die. As a result, vision deteriorates. If the optic nerve is compressed, it will not receive enough oxygen and nutrients. This can lead to atrophy and irreversible vision loss.
A low level of ophthalmotonus is an equally dangerous sign. If at high pressure inside the eye the capillaries are compressed, then at low pressure they are simply not able to push blood to the “destination point”. As a result, tissue atrophy of the visual organ occurs, which can also lead to blindness.
High IOP can also be a symptom of chronic cardiovascular disease. Low blood pressure may indicate liver failure or the onset of retinal detachment.
Why do you need to measure eye pressure?
- Something keeps floating and doubles...
Increased eye pressure does not manifest itself in any way and can suddenly lead to blindness at one moment. How to recognize the problem in time? Today our expert is an ophthalmologist, Dr. med. Dr. Erika ESKINA
What do an eye and a balloon have in common?
To understand what intraocular pressure (IOP) is, imagine an inflated balloon. Due to the pressure inside it, its shape is maintained. Likewise, eye pressure maintains the spherical shape of the eye and provides its nutrition.
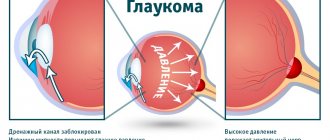
IOP is formed by the process of fluid flowing in and out of the eye. When it is released more than normal or the outflow is disrupted, the eye pressure increases. Also, the reasons for this may be the anatomical features of the structure of the eye, a disorder of the cardiovascular system.
High blood pressure can lead to the development of a chronic disease - glaucoma, which cannot be completely cured, and in 30% of cases it leads to irreversible blindness.
The field of view narrows gradually
With increased IOP inside the eye, the sensitive cells of the retina and optic nerve are destroyed, and metabolic processes are disrupted. But the worst thing is that the person himself may not even know about it until his vision deteriorates to such an extent that it is no longer possible not to notice.
Why is this happening? Destructive processes inside the eye (glaucoma), caused by increased pressure, begin not from the central, but from the peripheral areas of vision - the field of vision narrows gradually.
There is a common misconception that if you look at a light bulb or candle and rainbow circles appear before your eyes, it means that intraocular pressure is increased. This is not entirely true, because such sensations can occur at very high pressure (about 40 mm Hg), when there are two steps left before losing vision and urgent help from an ophthalmologist is required.
With a slight increase in IOP, heaviness in the eyes may occur, they quickly get tired, and the head hurts. But patients often attribute these symptoms to ordinary fatigue and do not attach much importance to them, but in vain. If these troubles bother you regularly, then it is better not to postpone a visit to an ophthalmologist and undergo an examination - measure your pressure, check the condition of the optic nerve and field of vision. After forty years, when the risk of glaucoma increases, it is advisable to undergo such an examination once a year.
Recently, experts have begun to identify another form of glaucoma, which can also only be detected during a full examination - it is accompanied by low or even normal pressure.
In such cases, even normal pressure is considered dangerously high for a particular eye.
Reduced is rare
Reduced IOP, although rare, is no less dangerous. Its causes are an underdeveloped eyeball, injuries, complications after operations. If low IOP persists for more than a month, the nutrition of the eye structures is disrupted, and as a result the eye may die.
LED glasses and miracle drops do not help
Do not believe false specialists who offer drops of energetically charged water, informational ophthalmic elixirs (IOE), microspheres, magnetic and LED glasses - laser vision, super vision, etc. as a panacea for glaucoma.
In order to reduce blood pressure, the doctor prescribes drops. Despite the seemingly simple purpose, the treatment process requires constant monitoring - side effects may appear or the eyes may simply get used to the drops, then the treatment regimen is changed.
If drops do not help, and no more than three types of drugs can be used simultaneously for one patient, the question of surgery is raised - laser or microsurgical, as a result of which a new path is created for the outflow of fluid from the eye or the old one is improved. But surgery does not eliminate glaucoma once and for all; it helps temporarily, and the treatment process must be continued constantly.
With glaucoma, there are no strict restrictions on visual load - you can watch TV or read. You should not drink more than 2 liters of liquid per day (including fruits and soups), lift heavy objects, or work upside down.
To see well...
Vitamins and foods that contain them will help reduce the risk of developing eye diseases and preserve vision:
A - most orange vegetables and fruits (especially carrots) and blueberries.
B1 - rice, vegetables, poultry.
B2 - milk, eggs, broccoli.
B6 - whole grains, egg yolk, brewer's yeast, beans.
B12 - meat, cheese, seafood.
C - rose hips, sweet peppers, black currants, sea buckthorn, citrus fruits.
RR - wholemeal bread, fish, nuts, vegetables, meat, dried mushrooms.
IMPORTANT!
Increased IOP may be a symptom of hormonal imbalance in the body (menopause, thyroid dysfunction) or other diseases. In this case, it is not so dangerous, but requires constant monitoring by an ophthalmologist.
For patients with glaucoma, low blood pressure is more dangerous than high blood pressure. When it is elevated, it is easier to maintain the level of nutrition of the optic nerve.
Risk factors for glaucoma: atherosclerosis, farsightedness, heredity.
Glaucoma occurs in 4 stages (4th, the very last, when the field of vision narrows to the maximum).
ON A NOTE
There are no generally accepted clear IOP standards. This largely depends on the method of measurement. The most common one in Russia is this: special weights with precisely adjusted weights are installed by eye. In this case, pressure up to 26 mm Hg is considered normal. Art. However, recent studies have proven that in 70% of healthy people, IOP is within 22 mmHg. Art.
IOP is also measured using a stream of air using devices called pneumatic tonometers. There are several models of this device, and each has its own pressure standards. Therefore, it is better to check with your doctor whether your blood pressure is normal.
The process of measuring IOP by any method is unpleasant, but painless.
BY THE WAY
Swimming and tennis will make your eyes sharper
Scientists have proven that physical activity is very useful for maintaining vision. The best sports are swimming, tennis, badminton, which train the muscles of the eyes and collar area and improve blood circulation in the organ of vision. But only if you play or swim for at least half an hour. A therapeutic neck massage is also useful. Ordinary walks are also no less useful, when we look at the surroundings and objects in the distance with interest.
In addition to vitamins A, C, D and E, the eye also needs calcium. It strengthens the sclera - the outer layer of the eye. And recently, scientists have found that with myopia, there is a lack of zinc, magnesium and iron in the sclera. This means that a person prone to myopia will benefit from complexes of vitamins and minerals.
Make your eyes dark
To give your eyes a little rest while working at the computer, American ophthalmologist Dr. Bates offers a simple exercise.
Sit at the table and lean on your elbows. Shake your hands and relax your wrists and fingers. Rub your palms together until they become warm. Rest your head on your hands and cover your eyes with your palms. The fingers of both hands should intersect on the forehead. Try to keep your hands completely relaxed and not putting pressure on your eyes. The palms should lie on the eyelids like a dome.
Feel the darkness. In the dark, rhodopsin, which is very important for vision, is formed in the light-sensitive cells of the retina. Now your eyes are completely relaxed. The perception of darkness is the deepest relaxation for the eyes, during which they are restored.
Imagine looking at a dark surface (such as a lake or the night sky) and it fills your entire field of vision, being transmitted along the optic nerve to the center of your brain.
After a while, some images will appear before your eyes again, but do not resist this and gradually return to everyday life. Let your eyes remain closed. First, remove your hands from your eyes and feel the difference in brightness and temperature. And then, when you're ready, close your eyes and open your eyes.
Who needs eye tonometry?
Eye pressure is measured by an ophthalmologist according to indications - symptoms that the patient complains about. These include:
- Deterioration of vision;
- Veil before the eyes;
- Headache radiating to the eyes and temples;
- Rapid eye fatigue;
- Impaired twilight vision;
- Redness of the outer membranes of the eye;
- Painful tension when trying to concentrate the gaze on some object;
- Pain felt while blinking;
- Dry eye syndrome;
- Deformation of the pupils;
- Narrowing of the field of view or loss of its individual sections.
You should not postpone a visit to an ophthalmologist to measure intraocular pressure, since in the early stages it causes almost no discomfort, and in the later stages the chances of saving your vision are already low.
Now it is clear why to measure eye pressure - so as not to miss the favorable time for effective treatment of impaired IOP.
Types of intraocular pressure
The pressure inside the eye may be high. Possible reasons:
- Hereditary or congenital abnormalities of the structure of the eyeball;
- Fluid inside the eye capsule is secreted in excess;
- The outflow of intraocular fluid from the capsule is impaired.
IOP may be low for the following reasons:
- Pathological development of the eye;
- Trauma to the eyeball;
- Recently had ophthalmic surgery.
Additionally, increased pressure inside the eye is classified. There are three types in total:
- Stable . Dangerous and progressive appearance. IOP is constantly elevated;
- Labile . The pressure rises periodically, but drops to normal on its own;
- Transitional . The increase in intraocular pressure is episodic, but quickly normalizes.
If the pressure inside the eyes increased once, and this does not happen again, most likely you had nervous strain, or the visual apparatus was tired. IOP may temporarily increase during attacks of hypertension.
6.8. Intraocular pressure examination
The level of intraocular pressure (IOP) can be determined in various ways: tentatively (by palpation), using applanation or impression tonometers, as well as non-contact.
Indicative (palpation) examination. It is carried out with the head still and the patient looking down. In this case, the doctor places the index fingers of both hands on the eyeball through the skin of the upper eyelid and alternately presses on the eye. The resulting tactile sensations (compliance of varying degrees) depend on the level of intraocular pressure: the higher the pressure and the denser the eyeball, the less mobility of its wall. The IOP determined in this way is designated as follows: Tp - normal pressure; T+1 - moderately elevated (the eye is slightly dense); T+2 - significantly increased (the eye is very dense); T+3 - sharply increased (eye hard as a stone). When IOP decreases, three degrees of hypotension are also distinguished: T-1 - the eye is somewhat softer than normal; T-2 - soft eye; T-3 - the eye is very soft.
This method of studying IOP is used only in cases where it is impossible to measure it instrumentally: in case of injuries and diseases of the cornea, after surgical interventions with opening of the eyeball. In all other cases, tonometry is used.
Applanation tonometry. In our country, this study is performed according to the method proposed by A. N. Maklakov (1884), which consists of installing a standard weight weighing 10 g on the surface of the patient’s cornea (after drip anesthesia). The weight has the form of a hollow metal cylinder 4 mm high, the base which is expanded and equipped with platforms made of milky-white porcelain with a diameter of 1 cm. Before measuring IOP, these platforms are coated with a special paint (a mixture of collargol and glycerin), and then, using a special holder, a weight is lowered onto the cornea of the patient’s eye, which is wide open with the fingers of the doctor, lying on the couch ( Fig. 6.16).
Under the pressure of the weight, the cornea is flattened and the paint is washed off at the point of contact with the weight area. A circle devoid of paint remains on the weight area (Fig. 6.17), corresponding to the area of contact between the surface of the weight and the cornea. The resulting print from the weight area is transferred to paper pre-moistened with alcohol. Moreover, the smaller the circle, the higher the IOP and vice versa.
To convert linear quantities into millimeters of mercury, S. S. Golovin (1895) compiled a table based on a complex formula.
Later, B. L. Polyak transferred these data to a transparent measuring ruler, with the help of which you can immediately obtain an answer in millimeters of mercury at the mark near which the imprint of the tonometer weight is placed (Fig. 6.18).
Impression tonometry. This method, proposed by Schiotz, is based on the principle of indentation of the cornea with a rod of constant cross-section under the influence of a weight of various masses (5.5, 7.5 and 10 g). The magnitude of the resulting corneal indentation is determined in linear quantities. It depends on the weight of the weight used and the IOP level. To convert measurement readings into millimeters of mercury, use the nomograms supplied with the device.
Impression tonometry is less accurate than applanation tonometry, but is irreplaceable in cases where the cornea has an uneven surface.
Currently, the disadvantages of contact applanation tonometry have been completely eliminated thanks to the use of modern non-contact ophthalmic tonometers of various designs. They implement the latest achievements in the field of mechanics, optics and electronics. The essence of the study is that from a certain distance a portion of compressed air dosed in pressure and volume is sent to the center of the cornea of the eye under study. As a result of its effect on the cornea, its deformation occurs and the interference pattern changes. The nature of these changes determines the level of IOP. Such devices allow you to measure IOP with high accuracy without touching the eyeball.
Study of eye hydrodynamics (topography). The method allows one to obtain quantitative characteristics of the production and outflow of intraocular fluid from the eye. The most important of them are: coefficient of ease of outflow (C) of chamber humor (normally not less than 0.14 (mm3-min)/mmHg), minute volume (F) of aqueous humor (about 2 mm3/min) and true IOP Po (up to 20 mm Hg).
To perform tonography, devices of varying complexity, including electronic ones, are used. However, it can also be carried out in a simplified version according to Kalfa-Plyushko using applanation tonometers. In this case, IOP is initially measured using sequential weights of mass 5; 10 and 15 g. Then place a weight weighing 15 g with a clean platform on the center of the cornea for 4 minutes. After such compression, IOP is measured again, but the weights are used in the reverse order. The resulting flattening circles are measured with a Polyak ruler and two elastocurves are constructed using the established values. All further calculations are made using a nomogram.
Based on the results of tonography, it is possible to differentiate the retention (reduction of fluid outflow paths) form of glaucoma from hypersecretory (increased fluid production).
- < Back
- Forward >
Palpation for approximate determination of the degree of ophthalmotonus
Before using hardware diagnostics, ophthalmotonus is measured by palpation. This honey gives a rough estimate of intraocular pressure. The ophthalmologist can determine the degree of scleral density by pressing on it through the upper eyelid with his fingers:
- Excessively soft (the finger sinks into the eyeball);
- Very soft (the finger is slightly pressed into the sclera);
- Soft (the elasticity of the sclera is slightly below normal, but it is higher than with the “very soft” degree;
- Normal (intraocular pressure is normal);
- Moderate (during palpation, increased density of the sclera is felt);
- Increased (the eyeball feels very dense to the touch);
- Stone (the sclera is so hard that when pressed with a finger it does not press through at all - like a stone).
This method of assessing ophthalmotonus is imprecise, but quite informative. Subsequently, hardware ocular tonometry may be prescribed. But you can limit yourself to this method if the patient has pathologies of the cornea or retina. Palpation is also well tolerated by children.
Contact methods of ocular tonometry
There are several contact devices for measuring eye pressure. Their advantage lies in the high accuracy of the data obtained (up to 1 millimeter of mercury). The disadvantages of contact methods of ocular tonometry are the possibility of infection and the need for pain relief before the procedure. Such devices are suitable for measuring IOP only in adults, since children may resist, which will lead to eye injury.
Maklakov method
The most accurate readings of pressure inside the eye are given by the Maklakov method. The algorithm for measuring IOP is as follows:
- The patient is asked to sit comfortably on the couch. Special drops are put into his eyes as a local anesthetic;
- The Maklakov tonometer is prepared, consisting of two weights in the form of hollow metal cylinders - they are moistened in a safe dye solution;
- One weight is placed on the central zone of the cornea of the right eye, and the second - on the left eye;
- The weights are removed and placed on paper to obtain prints from the remaining ink;
- The patient is given antiseptic drops to prevent infection and asked to get off the couch.
The marks left by the weights on the paper are of a strictly defined size, which depends on how much paint is left on the cornea. If there is little ink printed, the pressure is low; if there is a lot, the pressure is high. The sizes of the spots are measured with a specially graduated ruler, with the help of which the degree of IOP is converted into millimeters of mercury.
Goldmann tonometer
Recently, they often do the procedure not according to Maklakov, but use the Goldman device, although the techniques for measuring intraocular pressure are similar. In both cases, anesthesia and a dye solution are required.
The Goldmann apparatus is mounted on the slit lamp. After instillation of anesthesia and a dye solution, a prism is applied to the patient's cornea. It presses on the shell, flattening it and forming colored half rings. The pressure is carefully adjusted until these half rings are aligned at one point. Then the exact IOP is determined using a special scale.
Schiotz method
In adults, intraocular pressure is often measured using the Schiotz method. It is also associated with pressing a load of some mass on a metal rod onto the cornea. The patient is also given local anesthesia, but there is no need to use dye solutions. A weight is applied to the eyeball, which is subject to eye pressure from the inside. It prevents the load from being pressed, as a result the device deviates towards the shooter. The needle has a special scale, the values of which are checked against those entered in the calibration table. As a result, the ophthalmologist receives an accurate value of ophthalmotonus.
Dynamic contour tonometry (DCT)
This is a contact diagnostic method that, unlike other methods of measuring IOP, does not allow the cornea to be deformed during the procedure. How is IOP measured using VCT? The tip of the device is applied to the eyeball: it is made in the shape of a hollow figure corresponding to the patient’s cornea. In the center of the tip is a small pressure sensor.
The advantages of DCT are the independence of the sensor readings from the curvature and thickness of the cornea. Moreover, the sensor allows you to dynamically monitor intraocular pressure throughout the entire procedure, which typically takes only 8 seconds, and its readings are stored in computer memory.
Eye pressure in glaucoma: methods for measuring hydrodynamics
Measuring eye pressure in glaucoma is called tonometry, and measuring the speed (ease) of aqueous humor outflow is called tonography.
Tonometry
Eye pressure in glaucoma is a key indicator. It is measured by contact method - with weights of 5-10 grams (Maklakov tonometry) under local anesthesia with drops or non-contact - pneumotonometry. Anesthetic is not used for pneumotonometry. In the first case, tonometric pressure (Pt) is obtained, in the second - true pressure (Po).
When measuring, contact tonometers put a little pressure on the eye, and the IOP in it increases. The norm of eye pressure for Рt, determined with a weight of 10 g, is from 17 to 26 mm Hg. Art. When measured with a tonometer weighing 5 g, the norm of eye pressure is in the range from 11 to 21 mm Hg. Art.
Non-contact ocular pressure measured by pneumotonometry (Po) has a normal range of 9-21 mmHg.
Tonometry numbers are significantly affected by the rigidity (elasticity) of the membranes of the eye and the thickness of the cornea. To clarify the individual norm of eye pressure, pachymetry is performed - measuring the thickness of the cornea at several points. For thin corneas, add a few mm Hg to the obtained IOP values. Art., and if thick, subtract.
Table for determining the individual IOP level depending on pachymetry
| Corneal thickness, microns | IOP |
| 405 | +7 |
| 425 | +6 |
| 445 | +4 |
| 485 | +3 |
| 505 | +2 |
| 525 | +1 |
| 565 | -1 |
| 585 | -2 |
When the corneal thickness is over 585 microns, 2 mm Hg is subtracted. Art. for every 20 µm excess.
| Intraocular pressure is symmetrical in both eyes, with a difference in measurements of more than 2 mm Hg. Additional examination is indicated. |
During the day, eye pressure in glaucoma, as well as in normal conditions, is not the same. It is highest in the early morning hours, then gradually decreases and reaches a minimum at night. The amplitude of daily IOP fluctuations should normally not exceed 4-5 mmHg. Art.
Tonography
Tonography in the diagnosis of glaucoma allows one to evaluate the hydrodynamics of the eye in more detail. It is carried out using Maklakov tonometers, making several prints with weights of different weights, or an electronic tonograph. Both types of examination require local anesthetic drops. The hydrodynamics study lasts several minutes. It allows you to evaluate the true pressure in glaucoma, the minute volume of fluid produced by the eye and the coefficient of ease of outflow.
Normal values for this type of examination:
- minute volume (F) – from 1.1 to 3.58 cubic mm/min;
- outflow ease coefficient (C) – from 0.16 to 0.48 mm3. For glaucoma it is from 0.14 and lower;
- Becker coefficient (KB) – 27-98.
This examination is carried out both to verify the diagnosis and to assess the effectiveness of conservative or surgical treatment of glaucoma.
Methods for measuring IOP without contact with the cornea
In patients with pathologies of the ocular membranes and in children, it is more convenient to determine intraocular pressure in a non-contact manner. Its main advantage is that the procedure is painless and eliminates the risk of infection in the eye. However, the readings provided by a non-contact blood pressure monitor are less accurate. But in most cases they are sufficient to diagnose and monitor the condition of the patient’s eyeballs.
Air flow blood pressure monitors
Among non-contact devices for measuring ophthalmotonus, devices that supply air flow to the cornea are popular. The essence of the technique is as follows:
- The patient keeps his eyes open and focuses on a light point;
- The device turns on and it begins to deliver an air stream directly to the center of the cornea;
- Under air pressure at the site of exposure, the cornea is deformed;
- A special sensor assesses the degree of corneal deformation and provides an assessment of ophthalmotonus.
At low pressure, even a very light stream of air can deform the cornea. And with increased ophthalmotonus, the cornea is practically not pressed through. These changes are recorded by the device. However, its readings are inaccurate at low IOP, but allow a fairly high estimate of high pressure.
Optical coherence tomography (OCT)
This is a non-contact technique that helps to very accurately examine various tissues of the eyeball. An infrared beam is directed into the eyes of the patient, who is asked to focus on a specific point. It is projected on the retina. As a result, an interference pattern appears. During one procedure, the ophthalmologist receives several such pictures; for diagnosis, he selects the best one (where everything is clearly visible). Based on the selected picture, the doctor draws up tables, protocols and maps, and from them judges the value of ophthalmotonus.
Important! OCT makes it possible to diagnose glaucoma, pathologies of the retina and optic nerve in the early stages. But the method has a high risk of false negative and positive conclusions. Therefore, it is advisable to conduct additional diagnostics to confirm or exclude the suspected diagnosis.
Indicators of eye pressure in glaucoma
In the classic variant of the development of the disease, ophthalmotonus indicators are increased, there are other symptoms of glaucoma, changes in the fundus and visual fields.
In accordance with the level of pressure in glaucoma in the diagnosis, the degree of hypertonicity is coded using the letters of the English alphabet:
- A – normal IOP (not higher than 21 mm Hg);
- B – moderately elevated (22-32 mmHg);
- C – high (over 33 mm Hg).
In some cases, the upper limit of normal eye pressure is exceeded by 2-3 mmHg. interpreted as the individual IOP level. But such patients require clinical observation by an ophthalmologist and a thorough diagnosis to exclude early glaucoma.
Reduced eye pressure in glaucoma
The main goal of glaucoma treatment is to reduce IOP levels to values at which glaucomatous atrophy of the optic nerve fibers does not progress. This is called "glaucoma eye pressure tolerance." Its level is individual. Average tolerant IOP values for patients with primary open-angle glaucoma:
- with a central corneal thickness of less than 520 µm – 15.8 mm Hg (Po);
- from 520 to 580 µm – Po = 16.5 mm Hg;
- over 580 µm – Po = 17.6 mm Hg.
| When the disease is initially detected, a decrease in eye pressure in glaucoma by 20-30% of the initial value is shown. |
Subsequently, the level of ophthalmotonus, perimetry, and the thickness of the layer of nerve fibers around the optic disc are monitored according to optical coherence tomography data and conclusions are drawn about the effectiveness of treatment.
Portable blood pressure monitors
For people suffering from severe glaucoma, it is important to determine ophthalmotonus several times a day. How to measure eye pressure at home without visiting a doctor every time? There are special portable devices for this. They determine IOP by contact method.
The ICare device is often used to measure eye pressure at home. It has replaceable sensors that need to be momentarily applied to the cornea of the eye. Since the sensor is disposable, infection is practically excluded. A short contact time ensures that the procedure is painless and can be done independently or with the help of loved ones.
Important! The pressure inside the eye is constantly changing. It depends on breathing, heartbeat and other factors. Therefore, for more accurate readings, it is advisable to take several readings at a time, and take their average value as the true one.
The amount of intraocular pressure is an important indicator of the health of the visual organ. It allows us to judge the presence of a disease such as glaucoma, which constantly progresses and, if left untreated, leads to blindness. With regular violations of ophthalmotonus, it is important to determine their cause. Perhaps some chronic disease contributes to this. Then treatment of the underlying disease will help normalize the pressure inside the eye.
How is intraocular pressure measured?
The ophthalmotonus of an adult can change when taking coffee, alcohol, drugs, smoking, excessive physical and emotional stress, and intense work of the visual apparatus. Therefore, a few hours before the procedure, it is necessary to abandon these factors.
There are several ways to measure eye pressure levels:
- palpable;
- contact;
- contactless.
All methods are suitable for tonometry in both adults and children. However, in children they often resort to painless diagnostic methods.
Details in the video:
Palpation method
The finger, or palpation, method of measuring the approximate level of intraocular pressure is carried out by pressing with the pads of the fingers on closed eyelids. Subjective sensations are assessed: the doctor makes a conclusion based on the density of the sclera. If the sclera is soft, this indicates a decreased IOP, if it is dense, this indicates an increased one. The method is unreliable and is rarely used.
Contact methods
Contact methods include:
- applanation technique according to Maklakov;
- electronic tonography;
- tonometry using the iCare device.
Contact techniques are those in which the cornea of the eye is touched. Therefore, they are contraindicated after surgery and in the presence of inflammatory processes.
1. The essence of tonometry using a Maklakov tonometer is to determine the density of the eye using weights. Before measuring intraocular pressure according to Maklakov, the person is instilled with drops to anesthetize the cornea and placed on a couch. Then, one by one, special weights are placed on the cornea of each eye. Next, the weights are transferred to paper and a conclusion is made based on the diameter of the print.
2. Electronic tonography is a method that allows you to track the dynamics of changes during the procedure. The procedure time is 4 minutes. Methodology: after anesthesia, electronic sensors are installed that evaluate and record the obtained indicators graphically.
3. The iCare device allows you to obtain data on IOP by instantly touching the sensor to the cornea of the eye. The contact is practically not felt by the person. The device is easy to use and ideal for home use.
Non-contact tonometry
IOP can be measured without contact with the cornea using a pneumotonometer, TVGD and IGD.
- To perform a non-contact measurement with a pneumotonometer, you need to fix your head and look at the light point with your eyes wide open. The device delivers a stream of air to the surface of the cornea, after which it detects a change in its shape. The results are displayed on the screen.
- The TVGD device provides for the determination of intraocular pressure through a closed eyelid. TVGD-1 is intended for medical use, TVGD-2 is also approved for home use.
- A portable IOP (ocular pressure indicator) device has been developed that determines IOP by touching the device to the eyelid. Does not require pain relief.
The advantages of a non-contact tonometer for measuring intraocular pressure are the absence of the possibility of infection, painlessness, quick results, and ease of use.
Devices for non-contact measurement of intraocular pressure can be used both in medical institutions and at home.