Indications for tonometry
Often changes in IOP go unnoticed. The clinical picture, characterized by cephalalgia, asthenopia and redness of the mucous membrane of the eyes, is attributed to overwork. Most patients do not even suspect there is a problem.
Tonometry is prescribed and performed by an ophthalmologist. Indications for the procedure:
- neurological disorders;
- age over 40 years;
- complications after operations;
- spasm of accommodation;
- stress;
- fluid retention in the body;
- problems with the functioning of the endocrine system;
- presence of glaucoma in close relatives;
- glaucoma in the study patient.
There are also contraindications to the procedure. Measuring intraocular pressure using the Maklakov method is not carried out in cases of allergies to anesthesia, viral and bacterial infections, or a pathological condition in the structure of the cornea.
The examination is prohibited for patients under alcohol or drug intoxication, as well as for psychological disorders with increased aggression.
Features of tonometry according to Maklakov
Despite its age, the maklak method is very accurate, fast and inexpensive. One of the features of its implementation is that it is still a contact method, which means there is a risk of infection.
In addition, many people do not like the touch of a foreign object to the eye. But is this too high a price for an accurate result?
A good alternative to measuring intraocular pressure according to Maklakov is electronography. But since it is done using expensive equipment, which is not available in all clinics, measuring intraocular pressure according to Maklakov is still the most popular.
| It should also be remembered that the intraocular pressure measured by Maklakov will be higher than the result in other methods, so they cannot be compared with each other. |
Restrictions
- Recent eye surgery
- Allergy to anesthesia
- Inflammatory eye diseases
Evaluation of ophthalmotonometry results
The flatter the patient's cornea, the larger the diameter of the cylinder imprint. And the smaller the diameter of the light circle, the higher the pressure. The diameter of the print is measured with a transparent ruler, and the specialist places it with the scale down to avoid distortion. The ruler has already marked divisions in millimeters of mercury and there is no need to convert anything further.
Equipment and structure of the device
- Two 10 gram cylinders with flat ends made of frosted glass,
- Holder for carrying out the procedure,
- Ruler for measuring the diameter of the print. The Polyak ruler can also be used,
- Case for storing the tonometer.
Return to contents
IOP measurement methods
There are several ways to measure intraocular pressure:
- palpation - by touch;
- contact - Shiotz, Maklakov tonometer;
- non-contact - pneumometry, electronography.
The latter method is the most modern in ophthalmology. The contact method for determining intraocular pressure is most often used. With its help, IOP measurement is carried out by flattening the cornea. The Maklov method is the most common. Its advantage is low cost, simplicity and high accuracy of IOP determination.
Method for measuring intraocular pressure according to Maklakov
This is a method of contact measurement of IOP, which means contact of the weight with the cornea of the eye. Maklakov's tonometer is a mechanical device. These are 2 weights weighing 10 grams each.
To obtain an accurate result, it is necessary to strictly follow the measurement procedure.
Algorithm for tonometry to measure IOP according to Maklakov:
- The areas of the weights are wiped with a swab dipped in an alcohol solution. Then wipe dry with a sterile swab. Disinfection is carried out 2 times. Repeated use of alcohol after 15 minutes.
- The plates or weights are treated with a thin layer of special paint, which is not harmful to the eyes and is not toxic. The dye used is Collargol (contains 70% colloidal silver and 30% albumin protein) or Bismarck (a basic brown aniline dye used for staining histological and bacterial samples). Collargol (2 g) must be crushed in a mortar, then mixed with distilled water and glycerin. Bismarck brown is mixed in the same way, but in a volume of 1 gram.
- The tonometer is inserted into the socket of the support handle.
- The plate is touched to the stamp pad, which is pre-impregnated with paint. Then remove excess dye with a sterile swab.
- A solution of Dicaine or Lidocaine is instilled into the eyes. 2 drops into each organ of vision 2 times with an interval of 2-3 minutes.
- The patient is asked to lie down on the couch. The doctor is located at the head of the patient. The patient is asked to raise his hand and look up at the index finger.
- The ophthalmologist opens the eyelids with the thumb and index finger. The doctor widens the palpebral fissure. If there is excess tear fluid, remove it with a cotton swab or ball before applying the measuring device. With the second hand, the tonometer is installed on the central part of the cornea using a supporting handle. This should be done carefully, without pushing.
- Then the weight is lowered onto the cornea and under its weight it flattens. Contact of paint with the cornea is 1 second. The doctor immediately removes the measuring devices by lifting the holding handle. At the moment the device comes into contact with the cornea, the paint is washed off from the plate due to the circulation of tear fluid.
- Next, the doctor makes prints of the device’s platform on paper, which is pre-moistened with alcohol and ether or simply an alcohol solution. A colorless circle remains at the point where the device came into contact with the cornea.
- The ophthalmologist measures it using a ruler, the divisions on which represent millimeters of mercury. Measures the diameter of a colorless circle.
First, the study is carried out on the right eye, the doctor writes down the results on a piece of paper, which indicates the patient’s name, time and date of the procedure.
Measurements are then taken in the same way for the left eye. The action of Lidocaine is long-lasting. The ophthalmologist will have time to measure intraocular pressure for both organs of vision.
Intraocular pressure examination
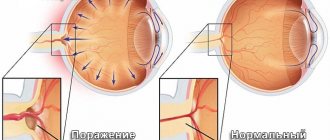
The eyeball is a spherical reservoir filled with liquid, incompressible contents. Intraocular pressure (IOP) is caused by the action of elastic forces that arise in the membranes of the eye when they are stretched.
The level of intraocular pressure (IOP) can be determined tentatively (by palpation) or using instruments (tonometers).
The following IOP options should be distinguished:
- statistical limits of normal pressure. Individual standards;
- fluctuations in IOP during the day, when the patient’s position changes, under the influence of other factors;
- tolerant pressure - tIOP;
- “target” pressure is cIOP.
The role of normal IOP in the physiology of the eye:
- IOP maintains the correct and stable shape and size of the eyeball;
- ensures a stable position of intraocular structures;
- supports the barrier function of the endothelium in the retinal vessels;
- promotes the removal of products of normal and pathological metabolism from the eye;
- reduces tension in the vascular walls, especially in capillaries and the possibility of their rupture;
- creates conditions for autoregulation of blood circulation in the vessels of the retina and optic disc.
Persistent hypotension and hypertension of the eye lead to serious consequences, including death of the eye.
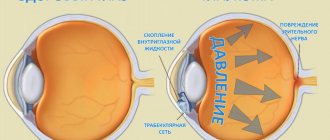
A distinction is made between the level of pressure in the eye and its fluctuations around the level. The IOP level is determined by the circulation of intraocular moisture in the eye and the pressure in the episcleral veins:
Po = F/C + Pv, where Po is IOP, F is the minute volume of intraocular humor, C is the coefficient of ease of outflow, Pv is the pressure in the episcleral veins.
The IOP level increases when moving from a vertical to a horizontal position and, especially, in the Trendelenburg position and when the veins of the neck are compressed due to an increase in venous pressure.
Fluctuations in IOP around the level depend on changes in the blood supply to the intraocular vessels and on external pressure on the eyeball. There are 3 types of rhythmic fluctuations of IOP around the level:
- ocular pulse with an amplitude from 0.5 to 2.5 mm Hg;
- respiratory waves from 0 to 1 mmHg;
- Hering-Traube waves from 0 to 2.5 mm Hg.
Blinking, squeezing the eye with the orbicularis muscle or the external muscles of the eyeball briefly increases IOP, massages the eye and reduces venous congestion.
Statistically normal IOP varies from 9 to 21 mm Hg. (on average 15-16 mm Hg). It has daily and seasonal fluctuations. The distribution of IOP in the population is asymmetrical (clustered to the right) and has two peaks at 15 and 17 mmHg. In old age, the asymmetry of the distribution increases. More than 3% of healthy individuals have IOP above 21 mmHg.
Regulation of intraocular pressure
Each eye is set to a certain level of IOP (equilibrium pressure), which is maintained using passive and active mechanisms. When IOP increases, the outflow pressure and filtration of fluid from the eye increase; when IOP decreases, the outflow of intraocular moisture decreases and equilibrium pressure is restored.
The active mechanisms of IOP regulation have not been sufficiently studied. The hypothalamus, adrenal glands, autonomic nervous system and local autoregulatory mechanisms may be involved.
Ophthalmotonometry
IOP measurement is based on obtaining the deformation of the eyeball under the influence of external influences
In this case, the values of deformation (S), force acting on the eye (W) and IOP (Pt) are related to each other by the following relationship:
Pt = W/S.
Classification of tonometers. All blood pressure monitors are divided into devices:
- With constant and variable pressure forces on the eye;
- With a constant or variable amount of eye deformation
- For corneal, scleral and transpalpebral
- For applanation, impression, transfiguration and ballistic
Ophthalmotonometers used in the Russian Federation:
- Maklakov tonometer and Filatov-Kalf elastotonometer;
- Goldmann applanation tonometer (reference);
- Perkins and Draeger applanation tonometers;
- non-contact applanation tonometer, Grolman, 1972;
- Schiotz impression tonometer;
- transpalnebral tonometer THz-01 “PRA”
Measurement techniques
Indicative (palpation) examination. It is carried out with the head still and the patient looking down. In this case, the doctor places the index fingers of both hands on the eyeball through the skin of the upper eyelid and alternately presses on the eye. The resulting tactile sensations (compliance of varying degrees) depend on the level of intraocular pressure: the higher the pressure and the denser the eyeball, the less mobility of its wall. The IOP determined in this way is designated as follows:
- Tn - normal pressure;
- T+1 - moderately elevated (the eye is slightly dense);
- T+2 - significantly increased (the eye is very dense);
- T+3 - sharply increased (eye hard as a stone).
- T-1 - the eye is somewhat softer than normal;
- T-2 - soft eye;
- T-3 - the eye is very soft.
This method of studying IOP is used only in cases where it is impossible to measure it instrumentally: in case of injuries and diseases of the cornea, after surgical interventions with opening of the eyeball. In all other cases, tonometry is used.
Applanation tonometry. In our country, this study is performed according to the method proposed by A. N. Maklakov (1884), which consists of installing a standard weight weighing 10 g on the surface of the patient’s cornea (after drip anesthesia). The weight has the form of a hollow metal cylinder 4 mm high, the base which is expanded and equipped with platforms made of milky-white porcelain with a diameter of 1 cm. Before measuring IOP, these platforms are coated with a special paint (a mixture of collargol and glycerin), and then, using a special holder, the weight is lowered onto the cornea of the patient’s eye, which is wide open with the fingers of the doctor, lying on the couch.
Under the pressure of the weight, the cornea is flattened and the paint is washed off at the point of contact with the weight area. A circle devoid of paint remains on the weight area, corresponding to the area of contact between the surface of the weight and the cornea. The resulting print from the weight area is transferred to paper pre-moistened with alcohol. Moreover, the smaller the circle, the higher the IOP and vice versa.
To convert linear quantities into millimeters of mercury, S. S. Golovin (1895) compiled a table based on a complex formula. Later, B. L. Polyak transferred these data to a transparent measuring ruler, with the help of which you can immediately obtain an answer in millimeters of mercury at the mark near which the imprint of the tonometer weight is placed.
Impression tonometry. This method, proposed by Schiotz, is based on the principle of indentation of the cornea with a rod of constant cross-section under the influence of a weight of various masses (5.5, 7.5 and 10 g). The magnitude of the resulting corneal indentation is determined in linear quantities. It depends on the weight of the weight used and the IOP level. To convert measurement readings into millimeters of mercury, use the nomograms supplied with the device.
Impression tonometry is less accurate than applanation tonometry, but is irreplaceable in cases where the cornea has an uneven surface.
Currently, the disadvantages of contact applanation tonometry have been completely eliminated thanks to the use of modern non-contact ophthalmic tonometers of various designs. They implement the latest achievements in the field of mechanics, optics and electronics. The essence of the study is that from a certain distance a portion of compressed air dosed in pressure and volume is sent to the center of the cornea of the eye under study. As a result of its effect on the cornea, its deformation occurs and the interference pattern changes. The nature of these changes determines the level of IOP. Such devices allow you to measure IOP with high accuracy without touching the eyeball.
Study of hydrodynamics of the eye (tonography). The method allows one to obtain quantitative characteristics of the production and outflow of intraocular fluid from the eye. The most important of them are: coefficient of ease of outflow (C) of chamber humor (normally not less than 0.14 (mm3-min)/mmHg), minute volume (F) of aqueous humor (about 2 mm3/min) and true IOP Po (up to 20 mm Hg).
To perform tonography, devices of varying complexity, including electronic ones, are used. However, it can also be carried out in a simplified version according to Kalfa-Plyushko using applanation tonometers. In this case, IOP is initially measured using sequential weights of mass 5; 10 and 15 g. Then place a weight weighing 15 g with a clean platform on the center of the cornea for 4 minutes. After such compression, IOP is measured again, but the weights are used in the reverse order. The resulting flattening circles are measured with a Polyak ruler and two elastocurves are constructed using the established values. All further calculations are made using a nomogram.
Based on the results of tonography, it is possible to differentiate the retention (reduction of fluid outflow paths) form of glaucoma from hypersecretory (increased fluid production).
Evaluation of results
The smaller the colorless disc after contact of the plate with paper soaked in alcohol, the higher the patient's intraocular pressure. If the diameter is large, then the pressure is low.
To measure IOP, a Polyak ruler is used. It gives results in mmHg. It is applied so that the light circle fits between the diverging lines of the scale and its edges exactly touch these lines.
Normally, the result should be 10–20 mmHg. This figure may change throughout the day. For example, in the morning, intraocular pressure is higher. Therefore, to obtain accurate results, ophthalmologists recommend performing the procedure 2-3 times a day at different times.
The boundaries of the circle may be unclear. This indicates poor quality paper used to make the print. The print will be clearer if you let the alcohol dry slightly, so the edges will not blur.
Algorithm for tonometry according to Maklakov
- Before starting the procedure, the holder and glass plates are disinfected with hydrogen peroxide or ethyl alcohol.
- Next, the prepared plates are covered with a thin, even layer of paint. Collargol or Bismarck-brown is usually used as a coloring agent.
- Since there is direct contact of the plate with the eye, anesthesia is used. The person lies down on the couch and a couple of minutes before the test, lidocaine, dicaine or proximetacaine is dripped into his eyes. When the anesthesia begins to take effect, the patient raises his hand and looks at his finger.
- The specialist carefully spreads the patient’s eyelids, tightly fixing his fingers on the periosteum. Then he lowers the tonometer onto the eye, which is fixed in the holder. The pressure of the metal cylinder causes the cornea to shrink. After the glass plates are removed, a certain amount of paint remains on the eye, which is washed off with saline solution.
- The doctor then performs the procedure on the other eye and then administers antibacterial disinfectant drops to the patient. Usually this is furatsilin, an aqueous solution of which has a detrimental effect on bacteria.
After the procedure itself, measurements and calculations are made. To do this, the paper must be moistened with alcohol and used metal cylinders placed on it. Circles of paint will be printed on the sheet. Using a ruler, the doctor must measure the diameter, which corresponds to millimeters of mercury. The normal pressure for this type of tonometry is 10-20 mm Hg.
These numbers may change during the day, because eye pressure is usually higher in the morning. Therefore, for a more accurate result, ophthalmologists advise carrying out the procedure several times a day and monitoring daily changes.
Preparing the paint is another necessary step for this procedure. Typically, the paint is collargol, which is mixed in a mortar with glycerin and distilled water. An analogue of collargol can be Bismarck-brown or methylene blue.
To cover the plates with prepared paint, you need a plug pad. But there is a safer treatment method in terms of possible infections - transfer the dye with a glass rod and rub it with a cotton swab.
Return to contents
| When using anesthetic drops, the procedure is absolutely painless and easily tolerated by patients. Reviews from people who have completed it are only positive. |