A person perceives more than eighty percent of information coming from outside through the organs of vision. This is why it is so important to maintain eye health. However, environmental problems, poor nutrition, disruptions in daily routine, stress and bad habits, as well as the constant use of electronic gadgets lead to the fact that the load on the visual organs is constantly increasing. As a result, the main element of the eye structure, the retina, suffers.
The essence of the method
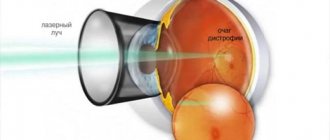
During preventive peripheral laser coagulation, a specialist treats thinned areas of the retina using a laser, soldering them in weak spots. This technique also allows you to improve blood circulation in the eye tissues, nutrition of the affected parts of the retina, and prevent fluid from penetrating under it.
The PPLC procedure cannot significantly improve vision. Its main goal is to reduce the risk of complications. The quality of a person’s visual perception after such an operation can improve in the absence of concomitant eye diseases that affect vision.
Possible contraindications
Strengthening is not carried out in the following situations:
- High myopia or hypermetropia;
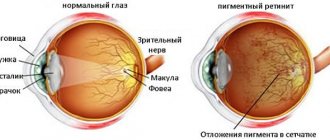
- Epiretinal gliosis. Epiretinal membranes are vascular cell proliferations on the surface of the retina, predominantly in the macula. Due to their dense structure, the laser passage process is disrupted;
- Hemorrhages in the fundus are considered a relative contraindication. Photocoagulation can be carried out only after they have been eliminated;
- Clouding of the stratum corneum and vitreous body, as well as the lens. Turbid media do not allow manipulation, as visualization of pathological areas is reduced.
Indications for PPLC
Often this operation is performed on patients who have been prescribed laser vision correction. According to statistics, about 60% of all people with visual impairments have problems with the retina and need to strengthen it. Therefore, before performing laser correction, the ophthalmologist may recommend PPLC to the patient.
Indications for its implementation are:
- Diabetic retinopathy.
- Tumor processes in the fundus of the eye.
- Local retinal detachment.
- Retinal angiomatosis.
- Retinal vein thrombosis.
- Peripheral retinal dystrophy.
Indications for implementation
The main goal of the technique is to create a strengthening adhesive between the retina and the choroid. The laser causes a burn ranging in size from 50 to 100 microns in duration for 0.05 - 0.1 seconds.
Laser coagulation is prescribed:
- Diabetic retinopathy. By influencing newly formed vessels, such dangerous conditions as hemophthalmos, traction detachment, and rubeosis of the iris are prevented;
- Retinopathy of prematurity (active phase). The technique stops the growth of venules and arterioles into the vitreous body, blocks the proliferation of connective tissue fibers;
- Rhegmatogenous detachment. This treatment method is effective only for fresh detachment;
- Formation of new vessels around the optic nerve head (if they occupy ? diameter). This increases the risk of multiple hemorrhages in the fundus and a sharp decrease in visual function;
- Peripheral dystrophy of the inner membrane. Laser photocoagulation carried out along the periphery stops further detachment;
- Benign and malignant tumors.
Technique
A person to whom a doctor has prescribed surgery must undergo a full examination of the eye organs and be tested by a local physician. To prepare for surgery, the patient may be hospitalized on the day of the proposed PPLC.
The procedure itself is carried out in the following order:
- The person being operated on is put on a sterile headdress and a medical gown. The entire operation must be carried out under perfectly sterile conditions to prevent accidental infection of the eye.
- Special drops are injected into the patient's eyes, which have an anesthetic effect and help dilate the pupil.
- Then a special lens is placed on the eye, the design of which resembles the eyepiece of a microscope. It is used to focus the laser beam and point it to the desired part of the eye.
- Next, using a laser, the specialist glues together weak and detached areas of the retina. The duration of the procedure is about 20 minutes.
- At the end of the procedure, the patient remains under the supervision of a specialist for 30 minutes.
During the operation, adhesions are formed on the retina, which prevent further detachment. Within 1–2 weeks after the procedure, the adhesions become fully formed and only after this the doctor will be able to judge how successful the operation was.
During the operation, the patient is in a sitting position. He feels the impact of the laser device as bright flashes of light or a barely noticeable tingling sensation. The procedure is not painful, but some patients may experience dizziness or a gag reflex. In order for the patient to undergo the operation more comfortably, the doctor recommends that he concentrate on the second eye.
The patient will be able to return home on the same day as the operation. Before discharge, the doctor gives him recommendations regarding further behavior and care of the operated eye.
How is the operation performed?
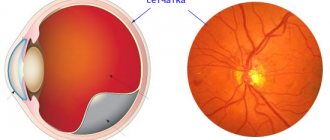
The basis of laser coagulation is the impact of argon laser beams on a limited area of the retina. Under their influence, a local increase in temperature occurs in this zone, as a result of which the process of coagulation (clotting) of tissue occurs. Since this process is very rapid, no hemorrhage occurs, and the treated areas are literally “soldered” to the choroid.
The procedure is performed under local drip anesthesia in a sitting position. An immediate anesthetic and pupil dilating drops are instilled into the patient's eye, allowing sufficient access to even the most difficult to reach areas of the retina.
After this, a special lens is installed on the patient’s eye, thanks to which the laser radiation can penetrate inside the eyeball and will be focused specifically on the problem area. At this stage, the patient may feel minor discomfort. It should be noted that the lens also securely fixes the eye so that the laser beam does not hit the healthy retina.
The surgeon controls the process of performing the intervention through a stereomicroscope. Coagulation can be performed both in limited areas of the retina and circularly, along its periphery - in each specific case it all depends on the indications. During the procedure, the argon laser heats the surface of the retina, “gluing” it to the vascular fundus. Coagulation points act as “nails” that keep tissue from tearing and peeling. In total, the doctor can perform up to three hundred cauterizations.
The patient himself will see the action of the laser as bright flashes of light. As a rule, patients do not experience any unpleasant sensations, although some complain of tingling, attacks of dizziness and nausea. After the operation is completed, the doctor removes the lens. The patient should sit quietly for a few minutes to recover.
Possible complications and rehabilitation
Most often, complications after surgery develop in patients who had contraindications to undergoing it. Complications may manifest as:
- Conjunctivitis.
- Cloudiness of optical media.
- Myopia.
- Corneal edema.
Complications can also arise as a result of an unsuccessful operation. Although such cases are extremely rare in ophthalmological practice, incorrect actions by the surgeon can still lead to negative consequences:
- If the ophthalmologist applies coagulants that are too large and have intense effects on the iris, inflammation may develop. As a result of the inflammatory process, posterior synechiae are formed on the retina, which lead to pupil deformation. To eliminate this complication, surgery is used.
- After PPLC, the angle of the anterior chamber of the eye may close, which leads to surges in intraocular pressure. This complication develops due to edema of the ciliary body or choroidal detachment, which can occur as a result of strong exposure to the laser beam.
- If the retina is exposed to a laser beam that is too narrow, the lens may be damaged and cataracts may develop.
Contraindications for surgery
Like any surgical intervention, laser coagulation has its own contraindications, in which the procedure is strictly not recommended or should be postponed to a later time.
With cataracts and other diseases that lead to disruption of the transparency of the eye, the ophthalmologist may simply not be able to clearly examine the affected areas. Therefore, before laser coagulation, the underlying disease must first be cured.
If retinal detachment is advanced, the procedure will simply be useless, so laser coagulation is not performed. Hemorrhages (bleeding) can also pose a serious obstacle to coagulation because they prevent the ophthalmic surgeon from viewing problem areas. If the hemorrhage is a one-time event, the procedure is performed after the blood has resolved.
Finally, with grade III gliosis and higher, when the light-sensitive cells of the retina are replaced by connective tissue, coagulation simply does not help solve the problem, so it does not make much sense.
It is noteworthy that pregnancy is not an absolute contraindication for laser coagulation. The procedure can be performed on patients almost until birth. Moreover, some women are recommended to have it if they decide to give birth naturally, without resorting to a caesarean section. In this case, when pushing, the risk of retinal tears increases, and therefore coagulation is an effective prevention. Of course, before undergoing the procedure, patients should consult a gynecologist.
Recovery period
The first time after surgery, the patient should be regularly monitored by an ophthalmologist, since complications may not arise immediately, but after 1–2 weeks.
In order not to provoke the development of complications, after the operation you should not strain, engage in intense physical activity or sports.
In addition, the patient should be aware of the following restrictions after surgery:
- Refrain from drinking alcoholic beverages for 1–2 months.
- Protect your eyes from hypothermia - try not to go outside in cold or windy weather. If such a need arises, you should try to spend as little time outside as possible.
- Avoid bending forward or standing in a vertical position.
- Protect your eyes from visual stress: refrain from driving a car, reading for long periods of time, or working at the computer.
Benefits of laser coagulation
Laser coagulation is performed on an outpatient basis. No special preparation is required. The procedure is non-contact, and therefore bloodless, and does not require a long time (one session lasts up to a maximum of twenty minutes). Since local drip anesthesia is used, pain relief does not put a strain on the patient’s internal organs and systems. Within a few hours after the operation, the patient can return to his normal lifestyle, observing only minor time restrictions.
Early period
In the early rehabilitation period, you must adhere to the following rules:
- after laser coagulation of the retina, you should not rub or frequently touch the organs of vision;
- it is advisable to reduce visits to crowded places to a minimum;
- do not overload the visual apparatus with reading and working with small particles;
- refrain from driving;
- on the day of coagulation, it is advisable to refrain from visiting the street;
- lifting weights is prohibited;
- do not consume caffeine;
- do not apply cosmetics to the eyes;
- refrain from removing makeup with products containing alcohol;
- eliminate emotional stress;
- do not lean forward.
In the first few days, it is advisable to adhere to bed rest. The recommended sleeping position is on your back. Vision is restored within 2 or 3 hours after the procedure as the effects of medications stop. The discomfort also disappears within a few hours.
Methodology for the PPLC procedure
PPLC is an outpatient procedure, performed under local anesthesia (drip), which is recognized as the most gentle at the moment. After anesthesia, the patient is comfortably seated in front of the laser device bar and his head is fixed with an arc. The person rests his chin on the bar, pressing his forehead as tightly as possible to the arch. PPLC includes several stages:
- The patient is asked to fixate his gaze while looking forward. A certain lens is placed on his eye, which prevents the eyelids from making involuntary movements.
- By directing the laser beam to the affected areas, the doctor applies coagulates.
- The lens is removed, the patient looks up, and drops with antiseptic properties are dropped into his eyes.
Typically, the procedure takes about 30 minutes.
There are several types of PPLC, which are divided according to the place and method of applying coagulates:
Peripheral . Coagulates are applied to the lateral areas of the retina to prevent its detachment.
Barrier . Coagulates are applied selectively in a certain amount, in rows, to the central region of the retina.
Focal . It is used for retinal lesions, which coagulate.
Panretinal . The entire surface of the retina is subjected to coagulation, with the exception of its central region.
Postoperative period
After surgery, it is very common to feel a slight discomfort and slight pain. In fact, vision may be hazy or blurry in the first 24 hours. On the second day after applying local adhesions, the patient must visit the clinic. An ophthalmologist evaluates the effectiveness of the minimally invasive treatment. In the postoperative period, fluorescein angiography is indicated to identify loci where additional strengthening is needed.
In the first 3-5 days, it is recommended to limit physical activity, as well as intake of liquid, sugar and salt. People suffering from diabetes need to control blood glucose, blood pressure and intraocular pressure.
Useful video
Due to laser vision coagulation, the development of complications is minimized. Only non-compliance with the ophthalmologist’s recommendations can lead to the development of pathological conditions. It is also mandatory to visit a doctor in the first six months, which helps to identify and eliminate inflammatory reactions of the conjunctiva in a timely manner. Particular attention should be paid to people with diabetes and hypertension.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.