- Indications for surgery
- Contraindications
- Choosing a prosthesis
- Company manufacturer
- Progress of the operation
- Recovery period
- Vision change
- Possible complications
- Getting free help
- Cost of the operation
- Patient reviews
- Video
Lens replacement is a microsurgical procedure in which an artificial acrylic or silicone lens is implanted into the eye after the natural lens is removed. These devices are called intraocular lenses or IOLs. After implantation, a person does not feel them, and the prostheses do not require additional care or replacement after a certain period of time. Replacing the lens is the only way to get rid of cataracts and associated blurred vision. There are other indications for such an operation - for example, correction of refractive errors.
Indications for surgery
There are the following indications for surgical treatment:
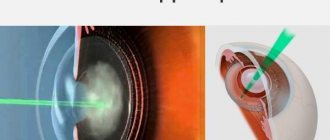
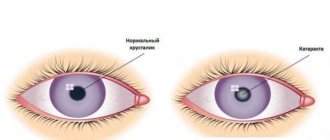
- Lens replacement is the most optimal treatment method for cloudy lenses – cataracts. Such operations are carried out most often. When cataracts occur, the cloudy lens becomes an obstacle to adequate light rays reaching the retina. In such a situation, the only option is lens replacement surgery, which involves removing the cataract using ultrasound or laser and implanting an intraocular lens. The IOL promotes adequate refraction of light, resulting in significantly improved vision.
- Refractive lens replacement is performed for presbyopia and farsightedness in patients for whom LASIK, photorefractive keratotomy, or phakic IOL implantation is not possible. For people who have a combination of presbyopia and moderate or severe hyperopia, lens replacement surgery is sometimes the only option to restore vision.
- Current lens replacement for myopia in case of contraindications to excimer laser vision correction or in case of high myopia.
- Astigmatism in complicated cases and with insufficient corneal thickness is also an indication for surgical lens replacement.
This operation is more complex and carries more risks compared to laser correction of refractive errors. Therefore, each case is assessed individually, the decision about surgery is made jointly by the doctor and the patient.
Replacement lens
Interview with ophthalmologist surgeon, candidate of medical sciences Anton Andreevich Abramov about new technologies in ophthalmology.
Abramov Anton Andreevich Ophthalmologist
Modern advances make it possible to restore the optics of the eye even in the most difficult cases and significantly reduce a person’s dependence on glasses. One of these most important achievements in medicine was the development of intraocular methods of vision correction, the essence of which is to replace the worn-out lens of the eye with an artificial lens. The development of intraocular optics and its subsequent improvement have given many patients a chance for recovery - even those who have finally come to terms with the dullness and blurriness of the world around them.
Anton Andreevich, what is the essence of the intraocular method of vision correction, and what ophthalmological disorders is it aimed at combating?
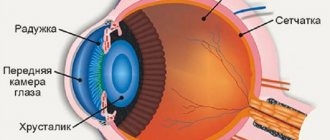
The optical system of the human eye is incredibly complex, and a special place in it is occupied by the lens, which resembles a biconvex lens, which, thanks to its accommodating properties, allows you to see equally well both far and near - a kind of natural photographic lens that induces sharpness. Due to a number of reasons, most often due to age-related changes, the lens becomes cloudy and ceases to perform its functions - focusing light on the retina. This phenomenon is known to everyone as cataracts. Before the invention of the artificial lens, after removal of the “cloudy” lens, patients were forced to wear very massive plus glasses, which made it possible to recreate at least some visual acuity acceptable for life. Today, an intraocular lens (IOL) can replace a failed lens. It is implanted inside the eye, does not require any personal care, is not noticeable to others, and is not felt by the patient himself.
It turns out that the need for glasses completely disappears?
Unfortunately, not always. In most cases, a monofocal artificial lens is used, which is suitable for almost all patients. The only downside to these single focus lenses is that they provide optimal vision either at distance or near. For example, if such a lens is selected for a patient for distance vision, then for reading or working on a computer he will need a slight correction with plus glasses. Another thing is multifocal (pseudo-accommodating) IOLs, the design of which allows you to create two foci on the retina, providing vision at different distances. On the surface of such artificial lenses there is a so-called diffraction zone, which consists of many ring-shaped micro-notches, gradually decreasing from the center to the periphery. They make it possible to focus light rays from objects that are located at completely different distances on the retina. The only drawback of such lenses is a rather impressive number of restrictions on their use due to the complexity of their optical design. In other words, they are not suitable for everyone and do not always provide the results that patients expect.
Are intraocular lenses aimed solely at combating cataracts or helping solve other vision problems?
A properly selected lens can not only replace a “foggy” lens, but also get rid of previously existing myopia, farsightedness, astigmatism, and even protect the retina from exposure to unwanted ultraviolet rays. It all depends on the model of the artificial lens. Thus, aspheric intraocular lenses are capable of transmitting images without any distortion, eliminating, first of all, spherical aberrations (blurred image contours or halos of different shapes around light sources). Toric IOLs allow the patient to free themselves from corneal astigmatism, and therefore from wearing special cylindrical glasses. In addition, phakic lenses can be used to correct severe myopia in young people for whom excimer laser correction is contraindicated. They are installed in addition to the natural lens (without the need to remove it), which allows you to preserve natural accommodation (from the Latin accommodatio - adaptation, adjustment).
Considering the variety of types of artificial lenses, an ophthalmologist can choose for each specific patient exactly the model that will ideally suit his lifestyle and professional activities.
How does the operation to replace or implant an artificial lens take place, and how long does the patient’s rehabilitation period last?
If earlier ophthalmologists had to be content with hard intraocular lenses, the implantation of which required large incisions and subsequent sutures, then with the creation of soft lenses, the procedure for replacing the lens has become completely atraumatic and painless. In modern clinics, including here in Scandinavia, when removing cataracts, a procedure such as phacoemulsification is used, during which a special ultrasonic tip is inserted through a puncture in the cornea, destroying and removing the clouded lens. In its place, when folded, an elastic intraocular lens is inserted, which then unfolds and is securely fixed inside the eye. The operation lasts no more than 20 minutes and does not require anesthesia - local drip anesthesia is used.
The undoubted advantage of this technique is the gentle nature of the surgical intervention: the resulting incision is so small that it seals itself, without requiring sutures. The patient returns home the same day, the rehabilitation period is about a week and consists only of limiting physical and visual activity.
What can the Scandinavia clinic offer its patients in terms of intraocular vision correction?
City clinics in St. Petersburg, operating under compulsory medical insurance, have a rather limited range of IOL models, while ophthalmologists at the Scandinavia clinic can offer their patients a wide range of the most modern artificial lenses from the world's leading manufacturers.
At the same time, the options differ not only in their functional characteristics, but also in price, so we can choose the type of treatment for people with different financial capabilities. Our specialists are armed with the highest quality equipment for both diagnostics and optics calculations, and the operation itself. All this, combined with the professionalism of doctors, allows us to achieve amazing results, which will be confirmed by many of our patients who have regained the happiness of full vision. Date of publication: 02/05/16
Contraindications
There are clinical situations in which lens replacement is contraindicated. Let's look at the main ones:
- Inflammatory processes of the eyeball in the acute or subacute phase. The decision about the potential possibility of intervention is made only after the acute inflammatory process has subsided.
- Retinal pathology, including detachment, tears, macular edema. These conditions are threatening and require urgent treatment. Planned surgical interventions, which include lens replacement, are not carried out in this situation.
- The small size of the anterior chamber of the eye or eyeball, which seriously complicates the technical execution of the operation.
- Concomitant general somatic diseases, including recent myocardial infarction or stroke.
This operation is planned, and therefore should be carried out against the background of compensation for somatic and concomitant ophthalmological pathologies.
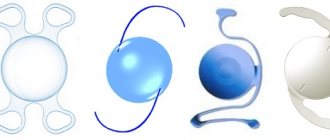
What it is?
An artificial lens (intraocular lens) is a lens made of artificial materials that is implanted into the eyeball as a replacement for a natural one during surgery. Any lens of this type consists of optical (provides good vision) and haptic (for fixation in the eye) parts.
In practice, two types of lenses are currently used:
- Soft - made of elastic polymer. They have the advantage of less trauma to the eye and do not require stitches after surgery.
- Hard – consist of organic glass. Implantation does not require many additional devices and involves suturing.
Any artificial lens must have flexibility, durability, sufficient refractive index and absolute transparency.
Installing a soft lens can be more expensive than implanting a hard lens. However, a soft lens has many advantages and carries a low risk of complications after surgery.
Choosing a prosthesis
There are many types of artificial lenses on the market today. The total cost of the operation directly depends on the material, properties and manufacturer of the lens. Depending on the model, intraocular lenses are divided into:
- Hard – used previously. Less practical - their implantation requires a large incision, requiring suturing and long recovery.
- Soft - implanted through a self-sealing puncture of the cornea several millimeters long. This is achieved due to the fact that the lens is introduced into the eye rolled up, and then straightened out and fixed.
Depending on the number of foci and the ability to accommodate, the following artificial lenses exist:
- Monofocal lenses provide good vision at only one focal length (near, far or intermediate distance). The advantage of such a device is its low price and, as a result, accessibility to a wide range of the population. Disadvantages include the need to use glasses or contact lenses for adequate vision at any distance.
- Multifocal lenses are an excellent option for correcting presbyopia. Such IOLs are classified as premium class in terms of functionality and price. They have magnifying power in certain areas, which allows you to clearly see objects at any distance without glasses or contact lenses.
- Accommodating IOLs. This type of lens, thanks to the combination of an aspherical shape and soft “hooks” - legs that support the position of the lens in the eye, provides good vision at various distances. “Hooks” allow the lens to slowly move forward when it is necessary to view an object up close, and when moving the gaze to distant objects, the intraocular lens moves posteriorly.
- Toric IOLs are suitable for the correction of astigmatism in combination with farsightedness or myopia. This happens due to different refractive powers on different meridians of the artificial lens. These IOLs also have special markings on the periphery that allow the surgeon to optimally position the lens during implantation.
Company manufacturer
When choosing a suitable prosthesis, the patient is often faced not only with many varieties, but also with variations in countries and manufacturing companies. Let's look at the most common ones:
- Domestic lenses. You can get such an IOL for free, provided that the operation is carried out under a quota (compulsory medical insurance policy). Russian artificial lenses are monofocal IOLs. Currently, the development and implementation of multifocal implants is underway.
- American lenses. These prostheses are among the most popular and reliable in the world. The most famous manufacturers are ALCON and CRYSTALENS, which produce a full line of artificial lenses. Such lenses are reliable, but they are distinguished by their high cost, which in some cases limits their use.
- German lenses. Companies such as Human Optics and Carl Zeiss are represented on the Russian market. These manufacturers produce high-quality prostheses, including aspherical and toric ones. They are used to correct complex astigmatism and other refractive errors.
Progress of the operation
Lens replacement surgery can be performed either on an outpatient basis or after preliminary hospitalization in a hospital. During preoperative preparation, a comprehensive examination of the organ of vision is performed, ophthalmoscopy is performed, and the fundus is examined. If necessary, ultrasound or optical coherence tomography is performed. This is necessary to identify diseases that affect visual acuity and potentially determine the outcome of the operation. In the preparation process, general clinical blood tests, electrocardiography, and radiography are performed.
30-40 minutes before the operation, a medicine is instilled into the eye to dilate the pupil. Local anesthesia is used in the form of anesthetic eye drops. Additionally, intravenous sedation is performed. If indicated, regional or general anesthesia is possible.
The patient is positioned lying on the operating table. The surgeon excises the anterior capsule of the lens through a puncture of the cornea, thus gaining access to the substance of the lens. Then a special titanium needle connected to an ultrasound source is inserted into the eye. Using ultrasound, the lens is crushed and phacoemulsification is performed. The crushed residues are removed from the eye cavity using an aspirator.
The next stage of the operation is implantation of an artificial lens. Modern intraocular lenses are soft and foldable, eliminating the need for large diameter incisions. After inserting the implant into the eye cavity, it is automatically fixed in the same place where the patient’s lens was previously located. No stitches are required. The eye is covered with a sterile bandage, which can be removed the next day. The entire operation takes 15-20 minutes.
Operational process
An intraocular lens (IOL) is a device that replaces the natural human lens. It is made of biocompatible materials that do not cause a reaction from the immune system. That is, after the introduction of an IOL, rejection does not occur.
First, the doctor examines the person’s eyes and selects an IOL individually for his vision. The following factors are taken into account:
- patient's visual acuity;
- the material from which the lens is made (hardness, presence of filters);
- the patient's work, the frequency of gaze transfer from one point to another is taken into account.
The surgical intervention takes place in several stages:
- Patient preparation. A person should report to a clinical facility in the morning on an empty stomach. It is not recommended to use a sedative before surgery to avoid side effects during the procedure. The doctor may ask the patient to apply antibacterial drops into the eyes a few days before surgery to prevent the spread of infection.
- Instilling an anesthetic into the patient's eyes. General anesthesia is not used, since after it the person’s well-being worsens.
- An incision on the cornea, detachment of the flap.
- Dissolving a person's own lens using a laser device.
- Placing an intraocular lens inside the eyeball, securing the cornea to the surface of the eye.
We recommend reading: Lens replacement
Immediately after the operation, the patient must remain in the clinic for several hours. Doctors are monitoring his condition. If no complications arise after the procedure, the person is sent home. It is important that he is accompanied by people, since the first day there may be a slight decrease in visual acuity.
If complications arise, the patient is prescribed additional diagnostic tests. The doctor identifies the cause of the deviation and carries out procedures to eliminate it. If the patient's condition worsens sharply, he is hospitalized.
Recovery period
During recovery after lens replacement surgery, the patient must carefully follow all medical recommendations. On the first postoperative day, rest and bed rest are necessary.
The operated eye is covered with a special protective bandage. In the following days, it is advisable to adhere to the following tips:
- Regularly apply eye drops to the operated eye according to medical recommendations.
- Avoid excessive sun exposure and use protective glasses in sunny weather.
- Avoid heavy lifting and intense physical activity.
- Do not rub or scratch your eyes.
- During hygiene procedures and while washing your hair, make sure that detergents do not get into your eyes.
- For 2-3 weeks, stop applying creams and decorative cosmetics to your eyelids.
- Limit reading, watching TV, working on the computer and other activities that require visual strain.
- Temporarily avoid visiting the bathhouse or sauna.
- Driving can only be resumed with the permission of the attending physician.
After operation
Replacing the lens for myopia is a fairly well-established operation. The postoperative period is usually well tolerated. The patient is discharged the next day after the follow-up examination, and vision is restored almost immediately. However, it is necessary to observe some precautions, which are mainly related to the need to protect the operated eye from damage. Recommended:
|
Vision change
The early postoperative period is accompanied by blurred vision and moderate pain. This is absolutely normal, there is no need to be alarmed. Subsequently, there is a smooth recovery of visual acuity. At first, double vision, flickering of spots, and color vision disturbances are acceptable.
As restoration progresses, the contours of objects become clearer, all artifacts disappear, and color perception and contrast improve. The duration of the recovery period varies from person to person. It is important to visit a doctor in a timely manner during this period for early diagnosis of complications and monitoring of the rehabilitation process.
Possible complications
Lens replacement surgery is one of the safest in the world. Tens of thousands of such interventions are carried out every year. There are still risks of complications.
Below we consider the most common variants of an undesirable scenario:
- Infectious inflammatory processes of the eyeball.
- Changes in the retina – detachment, macular edema.
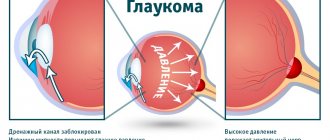
- Increased intraocular pressure. Diagnosis requires periodic measurement of intraocular pressure and the use of eye drops that relieve hypertension.
- Dislocation of the intraocular lens
- Formation of secondary cataracts, which can be removed with a laser.
All complications, if detected early, can be treated well. Therefore, if alarming symptoms occur, pain increases, or flashes of light appear, it is important not to postpone a visit to the doctor.
Complications after replacing the lens of the eye for cataracts
An effective and gentle method of phacoemulsification does not eliminate the risk of complications after replacing the eye lens for cataracts.
The advanced age of patients, concomitant diseases, and violation of sterility requirements by medical staff provoke undesirable consequences of the operation. Complications after cataract surgery occur in the form of swelling, astigmatism and other physical abnormalities.
People who have encountered such an unpleasant eye disease know firsthand that surgical intervention often ends badly, and there are complications after surgery.
Eye cataracts still require treatment. And unfortunately, the only way to get rid of the pathology is to perform an operation to remove the lens and replace it with an artificial one.
The procedure itself does not take much time and does not pose any threat to life and health, however, to avoid complications, you must adhere to certain rules and recommendations.
Types of complications
Complications that arise after the procedure include the following: Intraocular pressure in the eye increases. Inflammatory process. The retina of the eye peels off. Hemorrhage occurs in the anterior chamber.
The development of a disease such as secondary cataract. The new lens shifts slightly to the side. Below we will look at each type of complication in more detail. Inflammatory process.
After lens replacement, inflammation or swelling of the cornea and astigmatism almost always occur. That is why, after the operation is performed, the patient must be administered steroid drugs or antibiotics.
After two to three days, all symptoms of inflammation should subside. Hemorrhage. This complication is rare; in most cases, it is associated with damage to the membrane or cornea of the eye at the time of surgery.
As a rule, the patient does not hurt anything, he sees everything, and after a few days there will be no trace of blood left, it will simply resolve. If this does not happen, the doctor will have to forcefully flush the anterior chamber.
Additional fixation of the lens is also performed. Intraocular pressure increases. This type of complication can occur because the drainage system becomes clogged with drugs of a viscous consistency.
The doctor uses them to protect the cornea of the eyes. You can solve the problem by dropping drops into the eye. In rare cases, the specialist makes a small puncture through which the eyes are subsequently washed. Swelling of the eye or cornea and astigmatism are also observed, but it goes away quickly.
Retinal disinsertion. This complication can be considered one of the most severe; it occurs due to injury during lens replacement. People who develop astigmatism also experience this complication.
Many ophthalmologists insist on performing an operation during which the sclera is sealed. If the area of detachment is insignificant, then restrictive laser coagulation can be performed.
Retinal disinsertion
In addition, due to the fact that the retina is detached, another unpleasant problem arises - the lens moves. Patients complain of astigmatism, the eye hurts greatly, is constantly accompanied by a feeling of discomfort, and swelling occurs.
All symptoms last only for a while; after rest, this condition goes away. But with a significant displacement, visual discomfort will occur constantly. In order to solve the problem, it is necessary to perform repeated surgery.
The lens is completely displaced. Lens displacement is a dangerous and serious complication that requires immediate intervention from specialists. During the operation, the lens is lifted and then securely fixed in its new position.
Cost of the operation
| Service | price | |
| code | Name | |
| 20.08 Operations to replace the lens and for cataracts (per eye) | ||
| 2008001 | Ultrasound phacoemulsification without IOL implantation | 38500 |
| 2008002 | IOL explantation of category 1 complexity | 37500 |
| 2008003 | IOL explantation of category 2 complexity | 48000 |
| 2008004 | IOL explantation of category 3 complexity | 54000 |
| 2008008 | Ultrasound phacoemulsification with multifocal IOL implantation | 105900 |
| 2008010 | Ultrasound phacoemulsification with toric IOL implantation | 99000 |
| 2008012 | Cataract removal without phacoemulsification + IOL | 40500 |
| 2008013 | Ultrasound phacoemulsification with implantation of a multifocal toric IOL. | 120000 |
| 2008014 | Ultrasound phacoemulsification with implantation of a soft aspheric IOL of 1st category of complexity | 66360 |
| 2008015 | Ultrasound phacoemulsification with implantation of a soft aspheric IOL of category 2 complexity | 76000 |
| 2008016 | Ultrasound phacoemulsification with implantation of a soft aspheric IOL of category 3 complexity | 80000 |
| 2008017 | Ultrasound phacoemulsification with implantation of a soft aspheric IOL of category 4 complexity | 90000 |
| 2008018 | Fixation of a dislocated IOL of the first category of complexity | 35000 |
| 2008019 | Fixation of a dislocated IOL of the second category of complexity | 43000 |
| 2008020 | Fixation of a dislocated IOL of the third category of complexity | 49500 |
| 2008021 | Cataract extraction with implantation of an artificial lens of the first category of complexity | 33750 |
| 2008022 | Cataract extraction with implantation of an artificial lens of the second category of complexity | 38000 |
| 2008023 | Cataract extraction with implantation of an artificial lens of the third category of complexity | 42000 |
| 2008024 | Secondary implantation of an artificial lens of the first category of complexity | 42000 |
| 2008025 | Secondary implantation of an artificial lens of the second category of complexity | 48500 |
| 2008026 | Secondary implantation of an artificial lens of the third category of complexity | 54000 |
| 2008027 | Lensectomy of the first category of complexity | 30000 |
| 2008028 | Lensectomy of the second category of complexity | 38750 |
| 2008029 | Lensectomy of the third category of complexity | 40000 |
| 2008030 | Lensectomy for a dislocated lens of the first category of complexity | 40950 |
| 2008031 | Lensectomy for a dislocated lens of the second category of complexity | 48000 |
| 2008032 | Lensectomy for a dislocated lens of the third category of complexity | 51250 |
| 2008033 | Polishing the posterior capsule of the lens | 8000 |
| 2008034 | Discision of the posterior lens capsule | 7000 |
| 2008035 | Implantation of an intracapsular ring | 9000 |
| 2008036 | Posterior capsulorhexis | 8000 |
| 2008037 | Mechanical pupillodilatation | 9000 |
| 2008038 | Anterior vitrectomy of the first category of complexity | 19500 |
| 2008039 | Anterior vitrectomy of the second category of complexity | 22000 |
| 2008040 | Anterior vitrectomy of the third category of complexity | 24750 |
| 2008041 | Discision of secondary cataract | 7500 |
| 2008042 | Phacoemulsification for initial and immature cataracts, category 1 of complexity | 56000 |
| 2008043 | Phacoemulsification for initial and immature cataracts, category 2 of complexity | 58900 |
| 2008044 | Phacoemulsification for initial and immature cataracts, category 3 of complexity | 62500 |
| 2008045 | Phacoemulsification for complicated, mature and overmature cataracts, category 1 of complexity | 64500 |
| 2008046 | Phacoemulsification for complicated, mature and overmature cataracts, category 2 of complexity | 66360 |
| 2008047 | Phacoemulsification for complicated, mature and overmature cataracts, category 3 of complexity | 72400 |
| 2008048 | IOL made in USA/Germany | 28000 |
| 2008049 | IOL made in England | 22500 |
| 2008050 | Multifocal toric IOL | 85000 |
| 2008051 | Multifocal IOL | 65000 |
| 2008052 | Toric IOL | 35000 |
| 2008053 | Set of disposable consumables for phacoemulsification of cataracts. | 41000 |
| 2008054 | Navigation support for operations on the Verion system | 2000 |
| 2008055 | Domestic IOLs | 12500 |
| 2009001 | Ultrasound phacoemulsification of a transparent lens with IOL implantation for myopia and hypermetropia | 70350 |
| 2009002 | Implantation of a phakic IOL for myopia and hypermetropia (without removal of the native lens) {One eye} | 86400 |
| 2009003 | Optical-reconstructive intervention in the anterior segment of the eye for cataracts and post-traumatic and post-traumatic changes | 125000 |
| 2009004 | IOL implantation for aphakia | 62000 |
| 2009007 | Implantation of a phakic IOL for astigmatism (without removal of the native lens) {One eye} | 92300 |
In any private ophthalmology clinic, lens replacement can be performed on a commercial basis. The cost of the operation is influenced by the reputation of the clinic, its technical equipment and the specialists working there. The cost of an operation to replace a lens varies on average from 40 to 100 thousand rubles. The choice of implant model significantly influences pricing. Often, the actual cost of an artificial lens exceeds the cost of the operation by 1.5-2 times. Thus, the cost of a premium class intraocular lens is 45-85 thousand rubles, depending on the model and manufacturer.
Patient reviews
The majority of reviews from patients who have undergone lens replacement are positive. This type of surgery for cataracts or refractive errors allows people to see the world around them clearly. Negative reviews are often associated with discomfort during surgery or the recovery period. Not everyone is prepared for the fact that pain and blurred vision immediately after surgery are inevitable. Over time, the symptoms subside and vision improves.
Lens replacement surgery is a real chance for patients with cataracts and refractive errors not subject to laser correction to regain good vision. Modern possibilities of eye microsurgery help to quickly and comfortably restore vision.