What is a cataract?
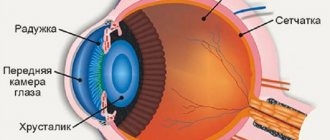
Eye cataract is a disease that is characterized by either complete or partial clouding of the substance of the eye lens or its capsule. The pathology is accompanied by decreased vision or loss of vision.
Despite the fact that cataracts most often occur in adults over 50 years of age, this disease is still characteristic of any age. There are several types of cataracts. These include traumatic, congenital, complicated and radiation cataracts.
The development of cataracts can be somewhat delayed, however, the older a person is, the greater the likelihood of detecting this vision pathology.
According to world statistics, there are about 17,000,000 people in the world with cataracts. And most of them are over 60 years old. At 75 years of age, 26% of men and 46% of women have cataracts. And among those whose age has already passed 80, the incidence of cataracts reaches 90%.
Content:
Symptoms of cataracts
Cataracts have several degrees of damage and depending on this the symptoms will vary, however, the main ones include:
- The occurrence of double vision in the case when the second one is closed at this time. This is an early symptom and disappears as the disease progresses.
- Blurry pictures, blurry images that cannot be corrected with contact lenses and glasses. At the same time, both close and far away objects are poorly visible. Patients characterize such vision as blurred, with the formation of a veil.
- The appearance of flashes and glare, occurring mainly at night.
- Increased light sensitivity of the eye at night. In general, night vision deteriorates. All light sources seem excessively bright to the patient, irritating the eyes.
- When viewing light sources, a person with cataracts sees halos around him. A person with lens opacity is unable to drive a car, or it is difficult for him to do so, as he is blinded by the headlights of oncoming traffic.
- The perception of color is impaired, they all become paler. It is especially difficult for a person to perceive shades of purple and blue.
- Improvement in vision that is temporary. This symptom is characterized by the fact that a person who previously wore glasses may abandon them as the disease develops. However, this time period is short-lived and vision will begin to deteriorate again.
- If a person often needs to change glasses for vision, there is reason to think about cataracts, since this disease tends to progress and quickly reduce visual acuity.
Symptoms of cataracts include the appearance of stripes and flickering spots or various balls. The ancient Greeks called this disease a waterfall, because with cataracts a person feels as if his eyes are covered with a veil, and he looks as if through foggy glass.
With cataracts, it is difficult to read, write, and work with small details. As the cataract matures, the color of the pupil becomes white instead of black.
Signs of cataracts: what to look out for?
Of course, in order to make an accurate diagnosis, it is necessary to undergo regular examinations with an ophthalmologist. This should be done annually, trying not to miss visits to the doctor, especially if you are already 40 - 45 or more years old.
It is difficult to independently detect cataracts at an early stage, but there are signs that allow you to suspect this disease in yourself or your loved ones:
Flickering before the eyes - strokes, spots
Difficulty performing fine visual work
The surrounding reality is turning yellow
The world appears blurry and distorted
Fog thickens in the field of vision
Rainbow halos around light sources
The quality of life decreases: it is impossible to drive a car, read newspapers, enjoy knitting sweaters, and so on, as before. The culprit is deteriorating vision.
And the state of health with cataracts also leaves much to be desired - the eyes get tired faster, and a person suffering from this disease may begin to be plagued by headaches. By the way, often the symptoms of incipient cataracts are attributed precisely to eye fatigue, without realizing that a dangerous disease may be hidden behind this.
Signs of cataracts
The first sign that allows a doctor to suspect a person has cataracts is the patient’s age over 60 years. In this case, the clinical picture has characteristic features. During examination, the ophthalmologist observes opacities that can be located in different parts of the eye: in the peripheral lobe of the lens, or opposite the pupil. The opacities are grayish in nature, sometimes with a white tint.
Depending on what type of cataract it is, the ophthalmologist will observe a varied clinical picture, accompanied by the following signs:
- An anterior cataract appears as a white spot with clearly defined boundaries. When it is slightly pushed forward and pointed, such a cataract is called anterior pyramidal.
- If the clouding is located at the posterior pole of the lens and is presented in the form of a round white ball, then it is said to be a posterior polar cataract.
- Central cataract is determined by such characteristics as: spherical appearance, location - center of the lens, diameter - 2 mm.
- A fusiform cataract can be judged by its shape. This clouding is presented in the form of a thin spindle, it is located along the entire length of the lens.
- Zonular congenital cataract has the appearance of a cloudy core with transparent layers.
- Cloudiness of the entire lens, liquefaction of its masses and further formation of a dense bag are signs of a dense soft cataract.
- Diabetic cataracts are characterized by the appearance of white opacities in the form of flakes. They are located over the entire surface of the lens, and changes in the iris often occur.
- Tetanic cataract is characterized by the same symptoms as its diabetic variety and is determined by the signs of the disease that caused it (hypofunction of the parathyroid glands).
- Toxic cataract most often manifests itself in the form of opacities located under the lens capsule, with subsequent spread to the cortical layers.
- Senile cataract has many symptoms and depends on the degree of progression of the disease: initial, swelling, mature and overripe.
These are the most common signs that allow us to characterize cataracts and attribute them to one type or another.
Varieties
Despite the fact that complicated cataract differs from the usual forms of the disease, the stage of its development remains unchanged. Each stage has its own characteristic manifestations.
- Initial stage.
Infiltration is observed in the internal structures of the eye, but the patient may not notice significant subjective changes in vision. A complicated variant of cataract can be suspected only in the case of known predisposing factors. - Immature form.
Typically, an ophthalmologist is consulted at this stage, when significant changes in visual acuity associated with clouding of the lens are noted. The cataract itself is just beginning to take on distinct outlines, but it may not be visible to the naked eye. - Mature cataract.
It is characterized by a visible change in transparency - the infiltrate appears as a light spot in the area of the pupil and iris. Cloudiness of the lens becomes noticeable to others - this determines significant discomfort and a cosmetic problem for the patient. - Overripe form.
Patients usually begin treatment before this stage, but in advanced cases, complete loss of vision is possible.
Forms are also distinguished depending on the location and characteristics of the pathological manifestations of cataracts:
- Swelling.
Clinical cases are characterized by less pronounced clouding over a fairly long period of time, as well as a decrease in the volume of the anterior capsule of the eye. - Posterior capsular.
Symptoms in this variant increase faster due to damage to the posterior capsule of the lens. Complicated cataracts, in contrast to the usual forms of pathology, are more often posterior capsular. - Incomplete complicated cataract.
The form of the disease implies the presence of cloudy spots that interfere with normal vision.
Complicated cataracts can be secondary - as a result of an operation performed to remove the damaged lens and its subsequent replacement with an intraocular lens (IOL).
Causes of cataracts
There are several positions that determine the etiology of the occurrence and development of cataracts. Among them are the following:
- Diabetes mellitus, leading to the development of diabetic cataracts and other thyroid pathologies. In particular, titania, muscular dystrophy and others.
- Smoking and long-term alcohol abuse.
- Eye injuries.
- Taking drugs belonging to the group of corticosteroids.
- Prolonged exposure to sunlight on the eyeball.
- The age of the person. The older he gets, the lower the body's ability to resist toxins coming from the external environment. In addition, the level of antioxidants provided by nature decreases.
- Retinal detachment, iridocyclitis, chorioretinitis, Fuchs syndrome, glaucoma and some other diseases lead to disruption of lens metabolism and the development of cataracts.
- Severe infections, for example, malaria, typhoid, smallpox and others.
- Anemia.
- Poisoning of the body, in particular with thallium, naphthalene and other toxic substances.
- Skin diseases, which include eczema, Jacobi poikiloderma, scleroderma, neurodermatitis.
- Eye burns.
- Myopia 3 high degree.
- A hereditary factor cannot be ruled out.
- Down's disease.
- Congenital cataracts often occur due to the fact that the pregnant woman has suffered severe infections, for example, rubella, toxoplasmosis, influenza, etc.
- Work in hot shops where the risk of eye exposure is high.
According to some sources, for more than 20,000,000 people in the world, this disease was the onset of blindness.
Cataracts can also be caused by poor ecology, poisoning by various toxic drugs, ultraviolet or radiation exposure, microwave radiation and smoking.
Prevention of cataracts
Cataracts are the aging of the lens of the eye, so prevention is achieved through general health measures that relate to lifestyle, nutrition and regimen. People who maintain physical activity and proper nutrition can, if not avoid, then significantly delay the aging of the lens and the body as a whole.
There are special recommendations. Cataract formation occurs under the direct influence of ultraviolet rays as a catalyst for free radicals. Sun damage to the cells of the lens is a trigger for lens clouding.
Hormonal drugs, corticosteroids and agents that increase sensitivity to UV rays have a similar effect on the eye. Tablet contraceptives and caffeine-containing drinks have a negative effect. After 40 years of age, blood glucose monitoring and a preventive examination by an ophthalmologist are mandatory.
What to do if cataracts appear?
First of all, when the first symptoms of cataracts appear, you should consult a doctor. An ophthalmologist diagnoses this problem. Using a slit lamp, he will examine and check the patient's visual acuity. This will help identify pathologies of the eye lens. To determine complications in the fundus, the ophthalmologist will examine it, first dilating the pupil with drops.
When diagnosing cataracts, you should not delay treatment, even if your vision is not impaired. It is worth understanding that this disease tends to progress, and the more cloudy the lens becomes, the worse the person will see.
Developing cataracts affect the patient's quality of life and will ultimately lead to complete blindness if treatment is not started. In addition, prolonged neglect of therapy can lead to the growth of opacities, increased intracranial pressure and the development of glaucoma. Next, the optic nerve dies and stops sending nerve impulses to the brain.
According to statistics, 12% of patients are susceptible to rapid progression of cataracts and the process of complete opacification takes an average of 6 years. A slightly larger proportion of patients, 15%, will lose their vision completely after 15 years. The main proportion of patients, which is 70%, will require surgical intervention on average after 6 to 10 years.
So, the only correct answer to the question: “What to do if cataracts appear?” is to go for a diagnosis to an ophthalmologist and begin treatment as quickly as possible.
Treatment of complicated cataracts
Conservative treatment of complicated cataracts is ineffective
and is extremely rarely used in the initial stages of the disease, when changes in the lens are considered reversible. Instillation of topical drops and taking systemic medications can improve blood circulation and nutrition of the affected eye structures.
Ultimately, surgery cannot be avoided. However, various types of complications can greatly complicate the operation and affect the tactics of its implementation and the choice of surgical techniques. Most often, the following technologies are used to treat complicated forms of cataracts:
- intracapsular extraction
– simultaneous removal of the lens and capsule. Most often used for severe subluxation of the lens, when the ligaments of Zinn, which hold the natural lens in the eye, are severely weakened and unable to perform their functions. In this case, an anterior chamber IOL lens is implanted - Artisan (Artisan, manufactured by Oftek Canada). - phacoemulsification of cataracts
- destruction of the lens using ultrasound, the procedure is quick and painless. The most modern modification of this well-known technique is phacoemulsification of cataracts with an active flow. - phacoemulsification of cataracts with femtosecond assistance
. This type of operation is preferable when removing complicated cataracts, since the destruction of the clouded lens is carried out remotely using a femtosecond laser, which significantly reduces the operation time and reduces the degree of energy impact on the eye. This type of surgery is safer and more gentle on the patient’s eyes.
After removal of the lens, the second part of the operation follows - implantation of an individually selected intraocular lens
– artificial IOL. The difficulty of treating complicated cataracts lies in the fact that concomitant diseases of the optic tract can negatively affect the outcome of the operation, and ophthalmologists cannot guarantee complete restoration of vision after treatment in this case.
It is important to see a doctor on time - only early treatment, correct actions by the doctor and full compliance with all recommendations by the patient can lead to successful treatment of a complicated form of cataract.
Stages of age-related cataracts
There are 5 stages of cataracts:
- anterior and posterior capsular cataracts;
- perinuclear layered cataract;
- nuclear cataract;
- cortical cataract;
- complete cataract.
The initial stage of cataract is characterized by the appearance of clouding of the lens not in the optical zone.
Cloudiness completely covers the lens in mature cataracts. With this form of the disease, a person can only distinguish between light illumination. Clouding of the lens occurs along the periphery, that is, outside the optical zone.
There is an immature cataract, which is characterized by clouding in the central part of the optical zone of the eye. In this case, visual acuity is impaired. Immature cataracts manifest themselves in such a way that the opacities move into the central optical zone. With immature cataracts, clouding of the lens leads to a noticeable decrease in visual acuity.
There is also an overripe type of cataract. In this case, the lens becomes milky white in color as the substance of which it is composed liquefies.
How quickly does a cataract mature?
Research shows that on average, twelve percent of people who have cataracts progress to a very serious stage within four to six years. Fifteen percent of patients experience a slow progression of the disease over ten to fifteen years. Seventy percent of patients experience cataract progression within 6 to 10 years. Mandatory surgical intervention is required.
Complications of cataracts
If cataracts are not diagnosed and treated in time, they can lead to complications such as:
- Complete blindness or amaurosis. It is cataracts that rank first among diseases leading to absolute loss of vision. In this case, blindness does not occur suddenly, it approaches gradually. If treatment is started on time, this complication can be avoided. The diagnosis of amaurosis is made when vision is completely lost.
- Lens luxation. This complication is characterized by the fact that it is completely displaced and separated from the supporting ligament. In this case, vision sharply deteriorates, and the lens itself must be removed.
- Phacolytic iridocyclitis, which manifests itself in inflammation of the ciliary body and iris. A person experiences severe pain in the eye and head, the vascular network becomes bluish or red, and the pupil moves poorly. When the acute process is eliminated, the question arises of removing the lens.
- Phacogenic glaucoma is characterized by a secondary increase in pressure inside the eye due to the fact that the lens increases in size. The lens requires removal and therapy is carried out to reduce pressure.
- Obscurational amblyopia. This complication often occurs in children and is a consequence of congenital cataracts. It is characterized by the fact that the retina, which does not receive signals from the outside, atrophies and ceases to function, although it was previously healthy. The only treatment for this complication is surgery.
To avoid such dangerous complications, the disease must be diagnosed and treated in time under the guidance of professional doctors. You should seek help when the first symptoms appear.
How to cure cataracts?
In order to cure cataracts, you should not delay visiting a doctor. Therapy can be conservative, in some cases surgical intervention is indicated. As for medicinal treatments, doctors prescribe drops to the patient that improve metabolism inside the lens. Stimulation of metabolism helps slow down the formation of cloudiness. If there is a break in the therapeutic effect, the disease begins to progress again.
In most cases, surgery is used to treat cataracts. Modern medicine has reached such heights that a person does not even have to go to the hospital. Most of the operations are performed in an outpatient setting and after a short period of time the patient is sent home.
The methods used for surgical treatment of the disease are varied. The previously used method of intracapsular extraction of turbidity has become history, as it is fraught with the development of complications and often led to injury to patients. A more modern method of surgical intervention is extracapsular cataract extraction, during which the cloudy masses are completely removed. In this case, the lens capsule is preserved and replaced with a flexible and rigid intraocular lens.
An even more modern method is the removal of cloudy masses using ultrasound. After which an intraocular lens is inserted. This surgical procedure is called phacoemulsification. The procedure itself takes little time and is completed in 10 minutes. In this case, the person does not require general anesthesia; local anesthesia is sufficient. After phacoemulsification, the patient is prescribed drops and observation by an ophthalmologist at the place of residence.
In order for the postoperative period to end faster and not cause complications, the patient is prescribed special drops:
- Floxal, Oftavix, Torbex have an antibacterial effect.
- Helps relieve inflammation Diclof, Indocollir.
- If the eye experiences increased dryness, then tear substitutes, for example, Oxyal or Systane, are prescribed.
- Drops containing hormones include Maxidex and Oftan-dexamethasone.
To avoid complications, it is necessary to follow the recommendations of the ophthalmologist, which boil down to a ban on lifting heavy objects and staying in dusty rooms. You should also be wary of hypothermia and walking in windy weather.
Do not let your disease progress, because in advanced forms of the disease, complete loss of vision is possible, which cannot be returned. With advanced cataracts, the lens swells, and this becomes an obstacle to the outflow of fluid inside the eye.
On the subject: Restoring vision - how to improve vision naturally?
Eye drops for cataracts
To treat cataracts, a variety of drops are used to stop the development of the disease and prevent complications after surgery. All of them can only be prescribed by an ophthalmologist. Self-treatment of the disease is unacceptable.
Catalin
Catalin - developed and produced in Japan, is a unique medicine for the prevention and treatment of age-related and diabetic cataracts.
Thanks to the active substance of the drops - Pyrenoxine, the process of converting water-soluble lens proteins into opaque substances (creating the feeling of a veil over the eyes) - stops and thus maintains its transparency.
Due to the regression of clouding of the lens, during the use of drops, there is a decrease in blurred vision, normalization of light sensitivity, and the sensation of double vision of objects in the eyes disappears. The drug is well tolerated.
Catalin is used continuously, 1-2 drops per eye up to five times a day.
A significant therapeutic effect of Catalin is noted after 3 months. after starting use.
Catalin is suitable for people diagnosed with early age-related cataracts; people with the appearance of cataracts as a consequence of complications from diabetes mellitus; people who are contraindicated for cataract surgery; as a prevention of complications after cataract surgery.
Oftan Katahrom
These are eye drops with an antioxidant and metabolic effect that slow down the development of cataracts due to their combined composition. The drug is produced in Finland and has been sold on the Russian market for more than 10 years. Contains substances such as nicotinamide, citrom C, adenosine and others. The use of this remedy helps to normalize metabolism in the lens and activate the processes of reduction and oxidation. Drops act as an antioxidant. The advantages of using the product are that they are not absorbed into the bloodstream, and the effect occurs in less than a minute.
You can use drops while pregnant, but only after consulting a doctor. The most common side effects include allergic reactions, some tingling and a burning sensation in the eyes. Very rarely, dizziness, increased blood pressure and nausea may occur. Sometimes a person suffers from fainting and shortness of breath.
The product should not be used in children under the age of majority, or if they are hypersensitive to the components included in the drops. It is important to avoid wearing soft contact lenses. If irritation occurs, you should not drive a car or operate other potentially dangerous equipment until it disappears.
Quinax
Drops used to treat cataracts, promoting the resorption of proteins that form in the lens of the eye. In addition, Quinax promotes the activation of enzymes contained in the moisture of the anterior chamber of the organ of vision. The advantage of the drops is that they have low absorption, have no side effects and do not interact with other medications. Drops can be used during pregnancy and in children only after consulting a doctor.
It is important to use the product for a long time, even if the therapeutic effect occurs in the shortest possible time. You should not instill Quinax without first removing your contact lenses. After applying the drug, you should wait at least 15 minutes and only then put the lenses back in place. If temporary visual impairment occurs after instillation, you should refrain from work associated with eye strain. The use of drops is indicated for senile, congenital, traumatic and secondary cataracts.
Taufon
Drops used for the treatment and prevention of cataracts, triggering regenerative processes in the tissues of the eye. Taufon helps normalize metabolism in the eyeball and improves metabolic processes. For cataracts, the course of treatment should be at least 3 months. Side effects include the possible occurrence of allergic reactions.
Drops can be used for traumatic, senile, radiation and other types of cataracts. It should not be used in childhood, or if there is hypersensitivity to the main active ingredient (taurine). Can be purchased at the pharmacy without a prescription.
Vizomitin "Skulachev Drops"
Drops are used to prevent dry eye syndrome and are often prescribed in the postoperative period. They help produce your own tears and improve the composition of the tear film. The duration of use depends on the severity of symptoms and is determined by the attending physician. If necessary, the drug can be used with other eye drops, including for the treatment of cataracts. However, you should maintain an interval between deposits of at least 5 minutes.
There are no side effects other than allergic reactions. Should not be used during breastfeeding or pregnancy. After opening the bottle, the drops remain usable for 30 days. The age limit is 18 years. A prescription is required to purchase.
Eye drops 999 for cataracts and glaucoma
A preventive and therapeutic agent that can relieve visual tension from the eyes, remove cataracts, tone the elements of the eye, and reduce intraocular pressure. Should not be used if there is severe eye pain or if an allergic reaction occurs. If you have eye infections, you should first consult an ophthalmologist.
It is worth understanding that the drug is not able to replace drug treatment, and serves as a prophylactic agent that has some healing effect.
Treatment
In cases where a complicated cataract leads to a significant decrease in vision that interferes with the patient’s usual activities, surgery to remove it is recommended.
The essence of the operation is the surgical removal of the cloudy lens, replacing it with an intraocular lens (IOL). An intraocular lens is an optical system that will subsequently assume the function of refraction. During the operation, a micro-incision is made on the capsule, then the lens substance is crushed with ultrasound and removed from the eye. An intraocular lens is implanted into the remaining capsular bag.
The right moment for surgery is the time of stabilization of complicated cataracts, with simultaneous compensation of the underlying disease (ophthalmological or general). For this purpose, they relieve the acute inflammatory process in the tissues of the eye, achieve remission of rheumatoid arthritis, compensate for the level of glycemia in the case of diabetes, etc. Contraindications to surgical intervention for complicated cataracts may include:
- Blindness. A complete lack of light perception gives an unfavorable prognosis for vision, even if the operation is successfully performed.
- IOP instability. Before performing phacoemulsification, it is necessary to achieve stabilization of IOP figures.
When contacting the Moscow Eye Clinic with complicated cataracts, the patient is guaranteed a comprehensive diagnosis with determination of the root causes of the disease and the development of an individual treatment plan, which will include the participation of doctors of other specialties.