Megalocornea in a child
The normal diameter of a newborn baby's cornea is 9 millimeters. With megalocornea, the parameters of the child’s cornea increase by 2 millimeters or more. At the beginning of the disease, the cornea remains transparent, as in its normal state. At the same time, the anterior chamber of the eyeball increases and becomes deeper. This stage is not characterized by the appearance of congestion in the eye itself. Intraocular pressure also remains normal.
Megalocornea may be a sign of hydrophthalmos. To determine the disease, you need to do an examination that will help identify congenital glaucoma.
The main distinguishing feature of megalocornea from hydrophthalmos is the absence of opacities of the cornea in the first case. With this disease, the corneal limbus does not expand or become thinner. No ruptures of the posterior limiting membrane are observed. With megalocornea, ophthalmotonus and glaucomatous excavation increase. A detailed analysis of the presenting symptoms will help establish a specific diagnosis.
With an increase in the volume of the anterior chamber of the eye, megalocornea is often accompanied by ametropia. If the process is unilateral, then the clinical picture may be supplemented by anisometropia, which leads to the progressive development of amblyopia (lazy eye) and concomitant strabismus. If such symptoms appear in a child, it is necessary to be examined by specialists and subsequently observed by an ophthalmologist.
A comprehensive examination includes examination of the fundus, determination of the refractive power of the optical system of the eye and measurement of intraocular pressure.
Experts prescribe preventive measures to help prevent the development of amblyopia and strabismus. If congenital glaucoma of the newborn is confirmed, treatment begins. Therapy helps to avoid secondary irreversible changes in the eyeball and dysfunction of the visual organs.
Features of the disease
Until the beginning of the 20th century, megalocornea was considered an abortive type of glaucoma. The idea of the disease was radically changed by the German researcher B. Kaiser, who discovered the genetic nature of the disease. In 90% of cases, the pathology is transmitted along the X-linked chromosome, so megalocornea is diagnosed more often in boys. In all other cases, inheritance is autosomal recessive, meaning a person can be a carrier of the gene but not suffer from the disease.
The disease is congenital, so the first signs are detected in the maternity ward. In most cases, there is no disruption of the normal transparency of the cornea, although the anterior chamber may be larger than normal. In addition, the eyeball and ophthalmic tone are also not affected. The primary task of doctors when detecting typical signs of the disease is to differentiate the disease from congenital glaucoma (hydrophthalmos). There are several characteristic differences between megalocornea and other similar diseases:
- There is no severe thinning or deformation of the limbus;
- There are no defects in Descemet's membrane;
- Functional disorders typical for glaucoma do not occur;
- Intraocular pressure is always normal;
- The disease does not progress, except for an increase in corneal diameter in proportion to age.
Megalocornea is diagnosed during the initial examination of a newborn, so it is possible to control the course of the disease from the first days of the child’s life.
Causes of megalocornea
The causes of megalocornea are that the pathology is transmitted from the owner of the defective gene or directly from mother to baby. The disease appears in the first trimester of pregnancy during the formation of the visual apparatus in the fetus. During normal development, the optic cup changes from a bell shape to a sphere. Changes occur at 6 weeks. In a fetus with megalocornea, transformation is observed later. Therefore, the diameter of the ciliary belt and adjacent structures increase in size. The anatomical distribution of the structural elements of the cornea does not differ from normal. However, it increases in diameter and becomes thinner.
Causes and mechanism of occurrence
In 1914, the disease was described by Kaiser, who first identified it as an independent clinical entity. He proved that the development of the anomaly is associated with the pathology of the X chromosome. Until this time, macrocornea was considered a type of congenital glaucoma. The disease is inherited in a recessive or autosomal recessive manner. Since only the X chromosome is affected, boys are more often affected. The carrier of the altered gene can be either a man or a woman.
At the stage of formation of the visual apparatus of the embryo, when the shape of the cornea should change from bell-shaped to spherical, in patients with megalocornea, the diameter of the opening of the eyeball for a long time continues to correspond to its equatorial size. This leads to an increase in the size of the anatomical structures of the anterior segment of the eyes. In this case, the corneal cells are distributed correctly, but over a larger area, and the membrane becomes thinner in the center.
Symptoms of megalocornea
Megalocornea is a bilateral disease that often does not progress. The main symptom of megalocornea is a transparent cornea, which significantly increases in diameter. The clinical picture of the disease directly depends on the progression of pathological disorders of the cornea. If no changes are observed, then the functions of the visual organ remain normal.
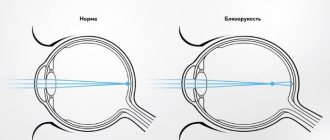
If a patient develops a bilateral lesion of the cornea, dystrophy and pigment dispersion may occur. In patients, visual acuity decreases, the outlines of objects are distorted. Myopia and astigmatism may appear. Sometimes eye disease is aggravated by partial dislocation of the lens, which occurs from stretching of the ligamentous apparatus. In this case, symptoms of iridodonesis arise - trembling of the iris, which appears with a sudden movement of the eyes. {banner_horizontalnyy2}
In the presence of pigment dispersion syndrome with further progression of secondary glaucoma, ophthalmotonus may increase. The pigment is redistributed from the pigment epithelium of the posterior layer of the iris. Melanocytes accumulate on the structures of the posterior part of the eyeball, which can cause disturbances in the trabecular network of the anterior chamber angle with changes in the outflow of intraocular fluid. The patient complains of haze before the eyes, a decrease in visual acuity is observed, unpleasant sensations arise in the eye and “rainbow circles” when looking at a light source. The severe course of the disease is accompanied by stretching of the iris, followed by the development of hypoplasia of the main substance of the cornea and increased pigmentation of the trabecular meshwork. When such changes occur, the Krukenberg spindle is formed.
Megalocornea mainly develops as an independent disease. The most common concomitant pathologies are lens displacement, pigment dispersion syndrome, congenital pupillary constriction, and cataracts.
Diagnosis of megalocornea
Megalocornea is diagnosed by conducting a thorough comprehensive examination of the patient. The main distinguishing feature of this eye disease from hydrophthalmos is that the disease does not progress, the cornea remains transparent.
With megalocornea, no functional disorders are observed, and glaucomatous excavation does not appear. Intraocular pressure is often normal.
To establish a diagnosis, specialists carry out differentiated diagnostics, which makes it possible to exclude congenital glaucoma or hydrocele of the eye.
Swelling of the cornea can occur due to birth trauma. The increase occurs in an oblique or vertical direction. With megalocornea, there is a horizontal increase in the cornea by more than 1 millimeter. Dystrophic changes are not observed: the corneal layer does not thin, Descemet's membrane remains intact, and the limbus does not expand.
Diagnostics
To identify the disease, the ophthalmologist performs a comprehensive examination, which includes:
- study of the fundus;
- measurement of IOP (intraocular pressure);
- ultrasonography;
- pachymetry (diagnostic method in which the thickness of the cornea is measured);
- visometry;
- biomicroscopy.
How is biomicroscopy performed?
This disease is characterized by an increase in the horizontal size of the cornea. If a patient’s cornea size is 2 mm larger than normal (which is determined depending on the patient’s age), then he is given an appropriate diagnosis. For example, for newborns the norm is a cornea of 9 mm, therefore, if the baby has a cornea larger than 11 mm, then he will be diagnosed with megalocornea.
Treatment of megalocornea
If visual acuity, refraction and intraocular pressure remain within normal limits, then no special therapy is required. If refractive errors such as astigmatism, myopia and farsightedness are detected, correction of visual perception is necessary using contact lenses or glasses. With megalocornea, surgical treatment is not always possible due to the constricted pupil and possible partial dislocation of the lens. There is also a possibility of rupture of the posterior lens capsule. If secondary cataracts occur due to the disease, then experts recommend phacoemulsification. After this, a special intraocular lens (artificial lens) is implanted. Surgery is performed through a corneoscleral incision. Retrobulbar anesthesia is used as anesthesia.
Treatment
Megalocornea currently requires absolutely no treatment, because it is not capable of having a possible negative effect on the general condition of vision. It does not matter when the patient was diagnosed with the disease; at any age, there are no unpleasant prognoses associated with vision loss for the patient.
The stage of the disease and the age of the patient do not affect its course and the occurrence of possible complications. To avoid possible worries for parents when a child is diagnosed with a disease, they should be advised to regularly undergo a full examination by an ophthalmologist.
Complications of megalocornea
If pathology occurs, you should immediately seek help from a specialist.
Megalocornea is dangerous due to complications that appear due to an increase in the size of the anterior ocular chamber:
- the liquid level between the chambers increases;
- cataracts occur;
- retinal detachment occurs;
- pigmentary glaucoma appears;
- the lens moves.
Also, against the background of megalocornea, spastic miosis may appear.
{banner_horizontalnyy3}
Possible complications
As a rule, this disease is characterized only by an increase in the horizontal size of the cornea (there are no other pathological changes).
However, due to the increased size of the cornea, an increase in the amount of interchamber fluid is possible, which can lead to disruption of the lens and retina. As a result, the following complications may occur:
- displacement or dislocation of the lens, phacodonesis (tremor of the lens), iridodonesis (tremor of the iris);
- development of cataracts;
- pigmentary glaucoma;
- possibility of retinal detachment;
- the appearance of astigmatism or myopia (this is in cases where there is also curvature of the cornea);
- embryotoxon development is an abnormal clouding of the cornea in a circle;
- the development of miosis (constriction of the pupil) is possible.
Prevention of megalocornea
There are no effective methods for preventing the development of megalocornea. If one of the parents has the disease, during pregnancy you must strictly follow all the specialist’s instructions, undergo an ultrasound examination and take care of your health. If there is a genetic mutation and the disease occurs, the first step is to differentiate the disease from other diseases, since megalocornea is rare. The disease does not endanger the patient's health, but after 30 years the chances of developing secondary cataracts increase. Experts advise periodically visiting an ophthalmologist and undergoing a detailed examination in order to notice the progress of the disease in time. Prof. The examination consists of procedures such as vision and tonometry. If you suspect an increase in the diameter of the cornea, it should be measured as quickly as possible.
Megalocornea is a fairly rare disease. Every little patient who is diagnosed with an illness is registered with a specialist and monitored throughout his life. The difficulty in preventing and treating the disease is explained by its genetic nature. However, even in the most difficult cases of megalocornea there is a possibility of partial recovery. A complete decrease in visual perception or blindness occurs only against the background of complications in the form of glaucoma or cataracts. Effective treatment methods help eliminate possible secondary diseases in this eye pathology.
Prevention
Unfortunately, today there are no sufficiently effective methods for prevention. Therefore, it is impossible to completely prevent the development of such an unpleasant eye disease as megalocornea, because it is congenital.
Because, in most cases, this disease is detected in newborns and during pregnancy, a woman should be especially attentive to her health. Prevention of the disease includes following the recommendations of a specialist and following all his indications. In this case, the consequences may be completely harmless to the patient.
The patient’s diet must be balanced and complete, and must also contain a sufficient amount of beneficial vitamins and minerals, which are required for the proper formation of a healthy fetus. It is also important to walk in the fresh air as much as possible, undergo regular scheduled examinations with a doctor, and also consult trusted specialists about the exact reasons that caused the onset of the development of this eye disease.
In this case, when during pregnancy a woman strictly follows all of the above recommendations, the likelihood of complications developing can be reduced to a very minimum.