The combination of neurological pathologies of the visual apparatus poses a great danger to humans, so it is important to monitor not only the state of vision, but also the health of the eye itself. One of the most serious diseases in this regard is paresis of the oculomotor nerve, which causes paralysis of the eyeball and other complications. In turn, the problem can only be a symptom of other diseases. It is difficult to treat and stop, so when you detect the first signs of a disorder, it is important to consult a doctor as soon as possible.
Description of the pathology, development mechanism
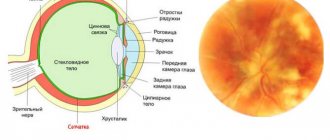
The oculomotor nerve is part of the third pair of cranial nerves and consists of viscemotor and somatomotor (motor) fibers. Its main function is to provide motor ability to the eyeball. The nerve controls the following systems:
- Ciliary muscles;
- Sphincter of the pupil (provides its ability to expand and contract depending on the lighting);
- Optical-kinetic nystagmus (the ability to follow moving objects);
- Muscles to regulate the movement of the upper eyelids;
- Vestibulospectral reflex (the ability of the pupil to move when the head turns);
- Accommodation (change in the curvature of the eye lens depending on surrounding objects and phenomena).
Thus, damage to the optic nerve always entails a limitation in the functionality of the visual apparatus. The movement of the eye and pupil is limited or lost. In turn, the lesion has its own reasons for occurrence or acts as a sign of another disease. Men and women of all ages are at risk, but statistics show that children are more likely to suffer from oculomotor nerve palsy.
Nerve pathology
Pathology of the abducens nerve
The fibers of the abducens nerve are located superficially, so during injuries they can easily be pressed to the base of the skull. Damage to the nerve is expressed in paresis - limited outward movement of the eye organ or complete paralysis.
https://www.youtube.com/watch?v=N9PkMdnhavE
With normal functionality of the abducens nerve, the edge of the cornea should touch the outer edge, the junction of the eyelids. If this is not observed, then there is nerve pathology. It has the following signs:
- movement of the eye organ is limited;
- objects inspected are split into two;
- repeated deviation of the eye;
- forced position of the head, which can be involuntary;
- dizziness, disorientation in space, staggering gait.
Nerve damage can be caused by infections:
- disease with encephalitis;
- previous syphilis;
- diphtheria disease;
- influenza and its complications.
As a result of intoxication:
- ethyl alcohol;
- toxic metals;
- combustion products;
- a consequence of botulism.
Paralysis of the abducens nerve occurs for the following reasons:
- previous meningitis;
- presence of tumor inclusions;
- the presence of hemorrhage, with pressure surges;
- thrombosis;
- purulent diseases of the nasal passages;
- eye socket injuries;
- temple bruises;
- metabolic disease;
- multiple sclerosis;
- stroke.
Nerve damage is distinguished by location:
- Cortical and conductive – diseases are localized in the medulla and brainstem.
- Nuclear defeat.
- Radicular lesions are observed within the medulla. This lesion is called Fauville's palsy, when, on the one hand, there is damage to the abducens and facial nerves, and on the other hand, there is damage to the limbs.
Peripheral paralysis is divided into:
- intradural is located inside the dura mater;
- intracranial is localized in the cranial cavity;
- orbital is located in a circle.
The oculomotor nerve is part of the third pair of cranial nerves and consists of viscemotor and somatomotor (motor) fibers. Its main function is to provide motor ability to the eyeball. The nerve controls the following systems:
- Ciliary muscles;
- Sphincter of the pupil (provides its ability to expand and contract depending on the lighting);
- Optical-kinetic nystagmus (the ability to follow moving objects);
- Muscles to regulate the movement of the upper eyelids;
- Vestibulospectral reflex (the ability of the pupil to move when the head turns);
- Accommodation (change in the curvature of the eye lens depending on surrounding objects and phenomena).
Thus, damage to the optic nerve always entails a limitation in the functionality of the visual apparatus. The movement of the eye and pupil is limited or lost.
In turn, the lesion has its own reasons for occurrence or acts as a sign of another disease.
Men and women of all ages are at risk, but statistics show that children are more likely to suffer from oculomotor nerve palsy.
In the early stages of oculomotor nerve paresis, there are practically no symptoms, which complicates its diagnosis and further treatment. With a longer course of the disease, the following symptoms gradually begin to appear:
- Drooping of the upper eyelid (partial or complete);
- Lack of reaction (constriction/dilation) of the pupil;
- Diplopia (double vision due to loss of motor ability of the eye);
- Divergent strabismus (occurs due to lack of resistance of the upper and lower muscles of the eyeball);
- Loss of focusing and adaptation to changes in the distance between the eye and the object;
- Loss of motor ability;
- Protrusion of the eye.
With extensive damage, immobility can become only part of the entire symptomatology of the disease if other cranial nerves are also damaged. In addition, oculomotor nerve palsy itself may be a symptom of a more serious systemic disease. Most often, the lesion affects only one eye.
In medical practice, there are two main forms of the disease:
- Congenital. Occurs as a result of intrauterine disorders of the development of muscles and nerves, as well as damage or damage to the facial and oculomotor nerves during development;
- Acquired. May have neurological, mechanical (traumatic injuries, consequences of surgical operations), aponeurotic prerequisites.
Paresis also occurs as a result of the progression of systemic diseases. In such cases, therapy should be aimed not only at eliminating paralysis, but also at relieving its causes.
Systemic pathologies that can cause paresis and paralysis:
- Diabetes;
- Arterial hypertension, instability of blood pressure;
- Benign tumors and oncology;
- Cervical osteochondrosis and other diseases of the spine;
- Aneurysm;
- Long-term use of Amiodarone, anticancer drugs and medications for the treatment of cardiovascular diseases;
- Hematomas;
- Traumatic eye injuries, foreign body entry;
- Inflammatory diseases of the brain (encephalitis, meningitis);
- Ophthalmoplegic migraine;
- Flu;
- Diphtheria;
- Syphilis;
- Brain hemorrhage, stroke;
- Vasculitis;
- Myocardial infarction.
The presence of at least one of the listed diseases is a reason for a systematic medical examination with a mandatory examination by a neurologist and ophthalmologist.
First of all, the examination should be performed by an ophthalmologist. During the diagnostic process, he must check:
- The presence or absence of deviation in the position of the eyeball;
- Absence or presence, strength of the pupil’s reaction to light exposure;
- The presence or absence of ptosis (paralysis of the upper eyelid);
- Eye focusing quality;
- The reaction of the pupil and eyeball to the movement of an object in space.
Thus, the doctor determines the probable site of the lesion, which further magnetic resonance imaging, superposition electromagnetic scanning, and X-ray examination will help to accurately determine. It is also necessary to collect anamnesis and information from the medical history. Additional research:
- Visometry;
- Ophthalmoscopy;
- Measuring intraocular pressure;
- Examination of the condition of the fundus.
Often, additional consultations with specialists in other areas are required: endocrinologist, neurologist, surgeon, infectious disease specialist, etc. In turn, they can prescribe additional hardware and laboratory tests.
One of the most important measures in the treatment of oculomotor nerve palsy is constant monitoring of the patient. In this case, a therapeutic effect on the root cause of paralysis is mandatory. If intervention is unavoidable, the doctor selects one of the more radical methods.
The main task of the computer program is to strengthen the muscles of the eyeball during the broadcast of special pictures. When viewing, patients experience increased nerve tension, due to which the body’s resources are mobilized and directed to improve their functioning. With systematic sessions, positive dynamics of treatment are observed.
Electrophoresis
Electrophoresis also gives good results of therapy. Before the session, electrodes are applied to the patient's closed eyes around the perimeter, as well as to the back of the head. The course of treatment consists of 15-20 sessions, the duration of which is no more than 20 minutes.
Surgery as a therapeutic method in the treatment of oculomotor nerve palsy is not always used. Typically, such a measure is required in two cases:
- If conservative therapeutic measures are insufficiently effective;
- With the progression of deterioration in the quality of vision, a decrease in acuity.
The operation is usually performed under local or general anesthesia (depending on the situation). After this, the patient must undergo a recovery period with a decrease in the load on the visual apparatus, as well as the introduction of a special regime of rest, sleep and physical activity. Additionally, the use of exercises and preventive medications is required.
Drug treatment in relieving paresis is ineffective. At the same time, to improve the patient’s condition, special eye drops that improve blood supply and tissue nutrition, physical therapy, and vitamin complexes can be used. Patients are also prescribed wearing bandages, sessions of viewing stereo images, proper rest and nutrition.
As a rule, it is possible to eliminate the pathology within three to six months with timely and correct therapy. First of all, conservative methods are used for this. If no improvement is observed during the specified period, other therapeutic measures are also added. Congenital pathologies, as a rule, cannot be completely cured.
In order to prevent congenital anomalies of the visual system, a pregnant woman must follow the prescribed regimen and undergo routine examinations by the attending physician and ultrasound examinations. To prevent acquired lesions, it is necessary:
- Observe safety precautions at work;
- Avoid traumatic situations;
- Avoid complications in the event of infectious diseases;
- Systematically undergo examinations by an ophthalmologist (at least once a year);
- Monitor and promptly treat systemic diseases.
If you experience discomfort, pain, or deterioration in focusing, you should consult a doctor as soon as possible. A positive treatment outcome is possible if the disease is detected only in the early stages of its development.
Conclusion
Paresis of the oculomotor nerve is one of the most dangerous diseases of the visual apparatus for humans. The disease is difficult to stop and treat, but its timely detection usually increases the chances of recovery. In addition, proper prevention of pathologies of the nervous system and visual organs will help to avoid complications.
Symptoms and signs of damage
In the early stages of oculomotor nerve paresis, there are practically no symptoms, which complicates its diagnosis and further treatment. With a longer course of the disease, the following symptoms gradually begin to appear:
- Drooping of the upper eyelid (partial or complete);
- Lack of reaction (constriction/dilation) of the pupil;
- Diplopia (double vision due to loss of motor ability of the eye);
- Divergent strabismus (occurs due to lack of resistance of the upper and lower muscles of the eyeball);
- Loss of focusing and adaptation to changes in the distance between the eye and the object;
- Loss of motor ability;
- Protrusion of the eye.
With extensive damage, immobility can become only part of the entire symptomatology of the disease if other cranial nerves are also damaged. In addition, oculomotor nerve palsy itself may be a symptom of a more serious systemic disease. Most often, the lesion affects only one eye.
Causes and symptoms
Symptoms of neuropathies are very varied and depend on which nerve is affected. It is customary to distinguish between cranial and peripheral neuropathy. With cranial nerves, any of 12 pairs are affected. Here we distinguish optic neuropathy (
with damage to the optic nerves
In peripheral neuropathy, the nerve endings and plexuses of the limbs are affected. This type of neuropathy is characteristic of alcoholic, diabetic, and traumatic neuropathy.
Also, the symptoms of neuropathy depend on the type of fibers that make up the nerve. If motor fibers are affected, movement disorders develop in the form of muscle weakness and gait disturbance.
In mild and moderate forms of neuropathies, paresis is observed, in severe forms - paralysis, which is characterized by a complete loss of motor activity. Moreover, after a certain time, atrophy of the corresponding muscles almost always develops.
So, if the nerves of the lower leg are affected, atrophy of the lower leg muscles develops; if the nerves of the face, then the facial and chewing muscles atrophy.
sensation of cold, warmth, goosebumps
Disruption of the exocrine glands (
for example, salivary
) is caused by damage to autonomic fibers, which also form part of various nerves or are represented by independent nerves.
Types of pathology
In medical practice, there are two main forms of the disease:
- Congenital. Occurs as a result of intrauterine disorders of the development of muscles and nerves, as well as damage or damage to the facial and oculomotor nerves during development;
- Acquired. May have neurological, mechanical (traumatic injuries, consequences of surgical operations), aponeurotic prerequisites.
Paresis also occurs as a result of the progression of systemic diseases. In such cases, therapy should be aimed not only at eliminating paralysis, but also at relieving its causes.
Diagnosis of neuropathy
The main method for diagnosing neuropathies is a neurological examination. In addition to it, instrumental and laboratory methods are also used. Of the instrumental diagnostic methods, electrophysiological study of peripheral nerves, namely electromyography, is of particular importance.
Laboratory methods include tests to detect specific antibodies and antigens that are characteristic of autoimmune and demyelinating diseases.
Neurological examination
It consists of a visual examination, examination of reflexes and identification of specific symptoms for damage to a particular nerve.
If neuropathy exists for a long time, then asymmetry of the face is visible to the naked eye - with neuropathy of the facial and trigeminal nerve, limbs - with ulnar nerve neuropathy, polyneuropathy.
Visual examination and questioning for facial neuropathy
The doctor asks the patient to close his eyes tightly and wrinkle his forehead. With neuropathy of the facial nerve, the fold on the forehead on the side of the injury does not gather, and the eye does not close completely. Through the gap between the non-closed eyelids, a strip of sclera is visible, which gives the organ a resemblance to the eye of a hare.
Next, the doctor asks the patient to puff out his cheeks, which also does not work, since the air on the affected side comes out through the paralyzed corner of the mouth. This symptom is called sails. When you try to bare your teeth, there is an asymmetry of the mouth in the shape of a tennis racket.
When diagnosing facial neuropathy, the doctor may ask the patient to do the following:
- close your eyes;
- frown;
- raise eyebrows;
- bare teeth;
- puff out your cheeks;
- try to whistle, blow.
Next, the doctor asks about the presence of taste disorders, and whether the patient has problems with chewing (
does food get stuck while eating
The doctor pays special attention to how the disease began and what preceded it. Was there a viral or bacterial infection? Since the third type of herpes virus can persist in the nerve ganglia for a long time, it is very important to mention whether or not there was an infection with the herpes virus.
Causes, prerequisites and risk factors for damage
Systemic pathologies that can cause paresis and paralysis:
- Diabetes;
- Arterial hypertension, instability of blood pressure;
- Benign tumors and oncology;
- Cervical osteochondrosis and other diseases of the spine;
- Aneurysm;
- Long-term use of Amiodarone, anticancer drugs and medications for the treatment of cardiovascular diseases;
- Hematomas;
- Traumatic eye injuries, foreign body entry;
- Inflammatory diseases of the brain (encephalitis, meningitis);
- Ophthalmoplegic migraine;
- Flu;
- Diphtheria;
- Syphilis;
- Brain hemorrhage, stroke;
- Vasculitis;
- Myocardial infarction.
The presence of at least one of the listed diseases is a reason for a systematic medical examination with a mandatory examination by a neurologist and ophthalmologist.
Causes of neuropathies
Why does the abducens nerve become damaged? What diseases can become provocateurs?
Some types of infections and intoxications have a very negative effect on the central system. As a result, the abducens optic nerve also suffers.
What infections pose a huge danger? These are diphtheria, encephalitis, neurosyphilis, influenza and others.
Alcohol, botulism, carbon monoxide and lead poisoning can also cause eye disease. Hypertension, tumors, diabetes mellitus, brain injuries and many others are factors in the onset of the disease.
Paresis is divided into two types: organic and functional. The second group usually causes difficulties in determining the cause of the disease.
Paresis of the abducens ophthalmic nerve associated with ischemic damage to small vessels is more common in adults. Diseases such as hypertension and diabetes have an impact here. The disease disappears on its own after three months.
Diagnosis of the disease
Treating oculomotor nerve palsy is quite difficult. However, timely diagnosis and identification of the cause of the disorder will help simplify the process and increase the chances of recovery.
First of all, the examination should be performed by an ophthalmologist. During the diagnostic process, he must check:
- The presence or absence of deviation in the position of the eyeball;
- Absence or presence, strength of the pupil’s reaction to light exposure;
- The presence or absence of ptosis (paralysis of the upper eyelid);
- Eye focusing quality;
- The reaction of the pupil and eyeball to the movement of an object in space.
Thus, the doctor determines the probable site of the lesion, which further magnetic resonance imaging, superposition electromagnetic scanning, and X-ray examination will help to accurately determine. It is also necessary to collect anamnesis and information from the medical history. Additional research:
- Visometry;
- Ophthalmoscopy;
- Measuring intraocular pressure;
- Examination of the condition of the fundus.
Often, additional consultations with specialists in other areas are required: endocrinologist, neurologist, surgeon, infectious disease specialist, etc. In turn, they can prescribe additional hardware and laboratory tests.
Treatment of paresis and abducens nerve palsy
The abducens nerve as a component of the nervous system
Recovery after paralysis occurs over a long period of time throughout the year. A well-known method of treatment is the use of physiotherapy - exposure to low-frequency electromagnetic field pulses and electric current stimulation.
https://www.youtube.com/watch?v=h_NgYBnbXpc
The treatment method has an analgesic, anti-inflammatory, calming effect. The disadvantage is that recovery is very slow, and in some cases does not occur at all.
The oculo-occipital method of administering the drug (neuromidin) is also used to increase muscle contractility and influence defects in the connective muscles.
The method of using electrophoresis with a solution of 15% neuromidine has proven itself well. The duration of the sessions is 15 minutes daily for 15 days. After completing the procedure, it is recommended to lie down with your eyes closed for 10 minutes.
If improvement and restoration of the functioning of the abducens nerve is not observed after treatment, and the lesion does not go away on its own, surgical intervention is used. The essence of the method is as follows: an injection of ultracaine is made under the conjunctiva, and a half-circumference incision is made.
The superior external and inferior straight nerves are split into two bundles lengthwise and the lower fibers are sutured to the upper fibers. This allows you to rotate the eyeball by more than 15–20° within a day after surgery, in some patients up to 25°; binocular vision was restored in every fourth person operated on.
To alleviate the condition of impaired binocular vision, Fresnel prisms are used, which are attached to glasses. Prisms have different angles and are selected individually. Possibly also closing one eye.
Most nerve diseases are associated with a disorder of the central nervous system, so treatment is prescribed accordingly. After suffering infections and successful treatment, the nerve damage is restored. In rare cases, when the tumor is inoperable, there is serious injury to the skull and the nerve itself, recovery may not occur.
Noticed a mistake? Select it and press Ctrl Enter to let us know.
A person is able to move the eyeball thanks to 3 cranial nerve pathways. The main role in this process is played by the oculomotor nerve, which goes under number 3. It is responsible for the movements of the eyelid and eye, as well as its reaction to exposure to light. The abducens nerve controls the abduction of the eyeball, and the trochlear nerve turns it outward and downward. These nerve pathways are numbered 6 and 4.
Any disturbances in the innervation of the extraocular muscles affect the ability to see fully. Among such disorders, one can highlight paresis of the eye muscles in children, since in addition to the main causes that are characteristic of adults, they often exhibit congenital anomalies.
They are usually treated using a whole range of procedures, and in especially severe cases, surgery is used.
Causes and symptoms
Abducens nerve palsy usually manifests as isolated paralysis. In this case, a person cannot fully avert his eyes and a double image of one object appears (diplopia).
This phenomenon occurs due to a violation of the innervation of the lateral muscle, for which the abducens nerve is responsible.
However, similar symptoms are characteristic of diseases of the orbit, so you should undergo a detailed diagnosis to make a diagnosis.
Damage to the trochlear nerve causes partial paralysis of the eye and the person has a double image in an oblique or vertical plane.
This symptom intensifies when the eye is lowered down, so people suffering from this pathology often walk with their heads tilted to the healthy side to reduce the manifestation of diplopia.
During diagnosis, myasthenia gravis (autoimmune pathology of nerve and muscle tissue) and diseases of the orbit should be excluded.
Oculomotor nerve palsy usually occurs in conjunction with disruptions of the facial, abducens, and trochlear nerve pathways. A separate form of pathology appears extremely rarely. The oculomotor nerve is damaged primarily due to an aneurysm. It often occurs on the posterior communicating artery and gradually compresses the nervous tissue.
The oculomotor nerve can be damaged by a growing tumor, as well as manifestations of stroke and multiple sclerosis. In most cases, such factors affect the nucleus of the nerve tract and the posterior longitudinal fasciculus.
Sometimes neuropathy of the oculomotor nerve, caused by the above reasons, manifests itself in the form of bilateral drooping eyelids (ptosis). In more rare cases, paresis of the superior rectus muscle of the eye is observed.
It is localized on the reverse side of the main site of damage.
According to statistics, the oculomotor nerve is often damaged due to a microinfarction. It can occur due to vascular pathologies, such as diabetes and hypertension. Such diseases usually do not immediately lead to disruptions in cerebral circulation and they should be predominantly in an advanced state.
Neuritis of the oculomotor nerve does not affect the reaction of the pupil to light, but in rare cases it is slightly weakened. A microinfarction occurs near the cavernous sinus or in the area of the interpeduncular fossa. It takes about 3 months for the oculomotor nerve to recover after suffering a disorder.
Diagnostics
It is easiest to recognize damage to the oculomotor nerve, since this pathological process is characterized by drooping eyelids, dilated pupils and abnormal eye deviations.
Based on such signs, making a diagnosis will not be a problem, but often they are combined with each other in various combinations, so the doctor suspects the secondary nature of the disease.
Sometimes a consultation with a neurologist may be required. If it was not possible to determine the cause of the pathology, then the patient should be registered with a doctor and periodically examined. To prevent the condition from worsening, your doctor may recommend special sets of exercises and other treatment methods.
Course of therapy
Treatment methods for paresis of the eye muscles in children are not particularly different from those in adults. However, it must be borne in mind that most congenital anomalies are corrected through surgery.
If the operation is successfully performed, the extraocular muscles are partially or completely restored.
If the problem is compression of the nerve pathway, then the main task is to eliminate the cause.
For this purpose, exercises that strengthen the oculomotor muscles are often used. They serve as the basis for the treatment of minor injuries and are a good preventive measure.
In severe cases of the disease, therapeutic exercises well complement the main course of therapy.
Drug therapy for paresis of the eye muscles may include the following:
- Vitamin complexes;
- Preparations for strengthening the extraocular muscles and restoring their innervation;
- Eye drops;
- Medicines that improve blood circulation;
- Corrective glasses and bandages.
The pathology can be treated with medications only according to the regimen prescribed by the doctor, so as not to aggravate its course and not to impair vision, especially if the child is sick. It is recommended to combine drug therapy with other methods, namely:
- Steriopictures. By watching them, the extraocular muscles are trained and blood flow improves. The nerve tissues that innervate the muscles of the eye are extremely tense during the procedure, due to this the lost innervation is restored. The procedure must be carried out under the supervision of a specialist so as not to cause complications;
- Electropheresis. This physiotherapeutic procedure is carried out with a 1.5% solution of Neuromidin. The duration of one session of electropheresis usually does not exceed 20 minutes, and it acts directly on the synapses (junctions) of the muscle and nervous tissue of the eyeball. After a course of such therapy, the patient’s severity of paresis decreases and the innervation of the eye muscles improves.
It is impossible to eliminate some causes of paresis of the eye muscles in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
Due to paresis of the extraocular muscles, many complications develop, such as strabismus, ptosis, etc. In children, this pathological process is often a consequence of congenital anomalies. It may not appear immediately, but only over time. This is why it is important to see an ophthalmologist and other doctors, especially in the first years of a child’s life.
The most common pathological conditions from damage to the abducens nerve are limited mobility (paretic state) or complete loss of motor ability (paralysis).
In a normal state, the edge of the iris of the eye is able to touch the commissure of the eyelids on both sides - the section of the eye is closer to the ear and to the nasal septum on the opposite side.
If this ability is impaired, a diagnosis of the onset of a pathological condition of the abducens nerve can be made.
Pathologies are characterized by the following conditions:
- The eyeball has limited mobility;
- Double vision, slight trembling of the eyelid;
- Peripheral deviation of one of the eyeballs;
- The position of the head is inclined towards the damaged eyeball;
- Damage to the vestibular apparatus, loss of coordination.
In a simplified way, the state of the abducens nerve is checked by an independent attempt to maximally abduct the eyeball: right-to-right, left-to-left. If it is impossible to abduct the right one, then a lesion of the right abducens nerve has occurred and similarly for the left nerve.
Therapeutic methods
One of the most important measures in the treatment of oculomotor nerve palsy is constant monitoring of the patient. In this case, a therapeutic effect on the root cause of paralysis is mandatory. If intervention is unavoidable, the doctor selects one of the more radical methods.
Computer program
The main task of the computer program is to strengthen the muscles of the eyeball during the broadcast of special pictures. When viewing, patients experience increased nerve tension, due to which the body’s resources are mobilized and directed to improve their functioning. With systematic sessions, positive dynamics of treatment are observed.
Electrophoresis
Electrophoresis also gives good results of therapy. Before the session, electrodes are applied to the patient's closed eyes around the perimeter, as well as to the back of the head. The course of treatment consists of 15-20 sessions, the duration of which is no more than 20 minutes.
Surgical intervention
Surgery as a therapeutic method in the treatment of oculomotor nerve palsy is not always used. Typically, such a measure is required in two cases:
- If conservative therapeutic measures are insufficiently effective;
- With the progression of deterioration in the quality of vision, a decrease in acuity.
The operation is usually performed under local or general anesthesia (depending on the situation). After this, the patient must undergo a recovery period with a decrease in the load on the visual apparatus, as well as the introduction of a special regime of rest, sleep and physical activity. Additionally, the use of exercises and preventive medications is required.
Adjuvant therapy
Drug treatment in relieving paresis is ineffective. At the same time, to improve the patient’s condition, special eye drops that improve blood supply and tissue nutrition, physical therapy, and vitamin complexes can be used. Patients are also prescribed wearing bandages, sessions of viewing stereo images, proper rest and nutrition.
Abducens nerve function
The nerve originates in the nucleus, located in the middle part of the medulla. Its fibrous structure crosses the pons and the brain center, passing its surface, called the basal. Then the path of the fibers flows along a groove located in the medulla oblongata.
Next, the fibrous threads of the nerve cross the membrane of the brain region, pass close to the carotid artery, move to the upper part of the orbital fissure and end their path in the orbit, firmly attached to the eye.
Nerve fibers control the rectus externus (lateral) muscle, which moves the eye outward and makes it possible to move the eyes to the sides without turning the head. The muscle is the opposite of the internal muscle tissue that pulls the eye toward the center. They balance each other out.
If one of the two muscles is affected, strabismus develops, since the other muscle pulls the eye organ towards itself, and the affected one cannot maintain balance. It is impossible to check the abducens nerve in isolation; it is examined together with the other two nerves.
Preventive measures
In order to prevent congenital anomalies of the visual system, a pregnant woman must follow the prescribed regimen and undergo routine examinations by the attending physician and ultrasound examinations. To prevent acquired lesions, it is necessary:
- Observe safety precautions at work;
- Avoid traumatic situations;
- Avoid complications in the event of infectious diseases;
- Systematically undergo examinations by an ophthalmologist (at least once a year);
- Monitor and promptly treat systemic diseases.
If you experience discomfort, pain, or deterioration in focusing, you should consult a doctor as soon as possible. A positive treatment outcome is possible if the disease is detected only in the early stages of its development.
Nuclear and peripheral palsy
What it is? What are the reasons for their appearance?
Nuclear palsy is often combined with peripheral palsy. This is due to the fibers of the facial nerve, which loop around the abducens nucleus. As a rule, when it is damaged, the pontine gaze center, the nucleus of the facial nerve and the pyramidal tract are attached.
The reasons for the formation of nuclear are:
Vascular disorders, encephalitis, multiple sclerosis, tumors.
Peripheral (flaccid) paralysis is a disease characterized by decreased muscle tone and paralysis of individual parts. Regardless of the reasons, it leads to the development of strabismus.
Factors causing the disease: meningitis, aneurysm, polymeolitis, botulism, diphtheria, injuries to the base of the skull, etc.
At the same time, the patient’s reflexes disappear and muscle tone decreases. In the paralyzed areas, a degeneration reaction occurs. The depth of electrical excitability indicates the degree of damage and further outcome.
The main distinguishing features of peripheral and central paralysis are the following:
- Complete/partial absence of reflexes.
- Muscle tone is noticeably reduced (hypotonia).
- Death of muscle tissue.
What tests are prescribed for the patient?
First, a general blood test. It allows you to determine inflammation in the body.
Secondly, toxicological, for the presence of toxic substances.
The following are used as instrumental diagnostic methods:
- Electroneuromyography (ENMG). Gives an assessment of the electrical activity of muscle tissue.
- Electroencephalography (EEG). Used to test different areas of the brain.
- CT.
- MRI. Magnetic resonance angiography to study the patency of arteries and identify tumors.