Severe myopia, or myopia, begins with a deterioration in the visibility of objects at a distance from minus 6 diopters.
As it develops, a person sees blurry silhouettes in the distance, and the quality of his life changes.
Such vision requires immediate correction. For this purpose, optical methods, surgical operations and adherence to recommendations are used. The choice of treatment method is influenced by the patient’s age, visual acuity, and individual characteristics. If you do not pay attention to problems in a timely manner, complications may arise - loss of vision, retinal dystrophy, glaucoma, disability.
Symptoms
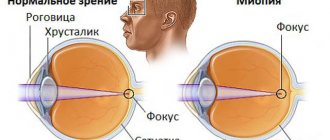
With any type of myopia, there is a pathological focusing of the image in front of the retina. This leads to decreased vision.
With a strong degree of myopia, a person sees blurredly in the distance, a clear picture is only in front of the eyes. The following symptoms occur:
- blurred image;
- headache;
- increased lacrimation;
- eye fatigue and discomfort;
- tension, visual fatigue over a short period;
- fogging, darkening before the eyes;
- increased reaction to light;
- diplopia, or double vision;
- distortion of the outlines and shades of objects;
- sensation of “floaters” before the eyes.
Features of grade 3 myopia in children
The average age at which myopia is diagnosed is 9-12 years. In adolescents, myopia increases. It is important to correct vision in a timely manner and eliminate the effects of negative environmental factors. Myopia in children is most often hereditary acquired type. At risk are children born with developmental anomalies, Down syndrome, severe prematurity and birth injuries.
You can suspect the development of myopia in childhood by the child’s habit of squinting his eyes while looking at distant objects, blinking frequently, wrinkling his forehead and bringing books too close to his eyes. When drawing, reading, or doing homework, such children tilt their heads strongly. They complain of a feeling of stinging and pain in their eyes, get tired quickly and are very tired at school.
If you suspect the development of myopia in a child, be sure to show the baby to a pediatric ophthalmologist. He will check your visual acuity, conduct the necessary studies and select the appropriate treatment. More often, specialists adhere to a wait-and-see approach, but it is recommended to limit physical activity and avoid visual fatigue. Highest myopia requires constant use of glasses. It is also recommended to use physiotherapy: laser therapy, electrical stimulation, electrophoresis, massage of the cervical-collar area.
Degrees
There are 3 degrees of myopia:
- weak – up to minus 3 diopters;
- average – up to minus 6 diopters;
- high – over minus 6 diopters.
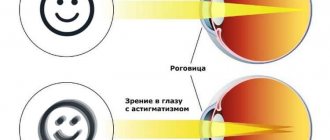
Depending on the degree of damage and changes in shape, there may be myopia of both eyes or one. The disease can also be accompanied by astigmatism.
Treatment is affected by different classifications of myopia. There are non-progressive and progressive types of the disease. In the first case, the same diopters must be maintained throughout the year.
Causes
Myopia greater than minus 6 diopters is called grade 3 myopia. For its reason, it is much more often acquired than congenital, inherited.
We recommend reading: Diopters for myopia
Risk factors that cause complicated high myopia are:
- excessive visual strain for a long time;
- ignoring the symptoms of visual impairment and the development of mild and moderate myopia;
- untreated infectious processes occurring in the organ of vision, leading to the development of complications.
Additional reasons for the development of the complex may include poor, unbalanced nutrition, premature or difficult births, poor ecology, and poor hygiene of the organ.
Treatment
The treatment of the disease is influenced by its degree and course. For more effective treatment, it is advisable to consult a doctor when the first symptoms appear, slight deterioration in vision, distortion of objects, or the appearance of darkening and flashing in the field of view.
For non-progressive types of myopia, treatment is not required. They resort to correction using optical lenses and glasses.
With a progressive type of disease, visual acuity quickly deteriorates over the course of a year, and irreversible consequences occur. Therapy is required aimed at stopping the pathology and partially restoring visibility. To do this, they use surgical intervention, additionally provide complete rest to the eyes, and organize proper and nutritious nutrition.
It is recommended to do eye exercises daily and, as prescribed by a doctor, take vitamin complexes and medications to improve metabolic processes and blood supply to eye tissue.
When myopia is combined with astigmatism, the second disease is treated with laser correction, and to improve visual acuity, surgery and implantation of intraocular lenses are performed.
Additionally, physiotherapeutic procedures and special methods are recommended to maintain eye health:
- use of computer simulators;
- laser therapy;
- magnetic therapy and electrical stimulation.
Optical correction
It is a conservative type of treatment without the use of surgery. Its principle is the selection and constant wearing of corrective contact lenses and glasses.
If contact lenses are worn by the patient mainly during the day, then for the purpose of optical correction it is necessary to additionally use corrective glasses in the morning and evening.
CLs are used to correct myopia up to minus 16 diopters. At the same time, they are selected by an ophthalmologist, taking into account the profession and individual characteristics.
The most effective are optical products made from highly refractive materials. It is also desirable to have additional properties that eliminate glare and transmit the maximum amount of light. This is facilitated by an anti-reflex antireflective coating.
Surgery
It is performed with a high degree of myopia and constant deterioration of visual acuity. There are laser treatment, implantation of intraocular and phakic lenses.
Laser correction is used to correct vision problems down to minus 13 diopters, with the maximum possible down to minus 15 diopters. For higher vision, an intraocular or phakic lens is implanted.
Their difference is as follows: the first is an artificial lens and is installed in place of the natural lens, and the second is installed directly in front of the lens without removing it, in the anterior and posterior chambers of the eye. These types of treatments are used when visual acuity is up to minus 25.
During laser correction, a device makes a small incision in the cornea and evaporates its cells to give it the correct shape and restore visual acuity. This is done using one of 3 methods - LASIK, PRK. The choice of technique is made by a specialist depending on the results of a comprehensive diagnosis of the patient and determination of his condition.
After laser correction, a long rehabilitation period is not required. However, you should follow the recommendations of a specialist, neglecting which can provoke further development and progression of myopia.
How is complicated myopia treated?
The treatment method for complicated myopia depends on concomitant eye diseases, the patient’s age and other factors. Before surgery, the patient undergoes a detailed vision examination. The following methods of vision correction have proven themselves to be the best:
- Refractive lens replacement. The method is effective for complicated myopia with changes in the optical power of the lens. An intraocular lens is implanted in place of the natural lens. Doctors practice the method of ultrasonic phacoemulsification - it is painless and has a minimal rehabilitation period.
- Laser correction. Considered the gold standard in the treatment of myopia. It involves deforming the shape of the cornea with a laser. There are different laser correction techniques - LASIK, EPI-LASIK, LASEK, PRK and many others. As a result of the operation, light rays passing through the lens are focused on the retina of the eye. Laser correction does not require hospitalization of the patient.
Complicated myopia is currently not a death sentence for the patient.
Modern methods and technologies make it possible to successfully correct this pathology. The sooner the patient seeks help from an experienced ophthalmologist, the easier the operation will be. During the postoperative period, the patient should be regularly checked by the surgeon who performed the operation. He will be able to track the recovery process and prevent the development of complications. Mironova Irina Sergeevna
Complications
High myopia can lead to dangerous complications, worsen the patient’s quality of life and make him visually disabled. Highlight:
- high myopia with astigmatism, when, in addition to impaired visual acuity, refractive pathologies are observed, accompanied by a deterioration in the clarity of the objects in question;
- detachment of the retina from the choroid due to changes in the shape of the eye and thinning of the components, which can lead to irreversible loss of vision;
- cataract – there is clouding of the lens, deterioration of visibility and blindness when overripe;
- glaucoma is a common disease in which the patient experiences increased intraocular pressure and pathological production and outflow of aqueous humor, leading to defects in the visual field, its decrease, and optic nerve atrophy;
- retinal dystrophy - a pathology when degenerative processes occur in the retina and the clarity of the visible image deteriorates;
- destruction of the vitreous body;
- retinal stretching and hemorrhages.
With a high degree of myopia, natural childbirth is prohibited - the woman is offered delivery only by cesarean section. Because pushing may increase intraocular pressure, deteriorate vision, and cause retinal rupture. This is affected by incorrect breathing technique and pushing.
Also, people with severe myopia should not serve in the army.
Pathological myopia: definition and classifications
The term “pathological myopia,” as noted above, was originally used to refer to myopia, which is accompanied by characteristic degenerative changes in the sclera, choroid and retinal pigment epithelium, leading to decreased vision [9]. Excessive elongation of the eyeball and posterior staphyloma are believed to be important factors in the development of these degenerative changes in pathological myopia. However, refraction or axial length alone cannot influence the formation of pathological myopia. Posterior staphyloma, which is a hallmark of lesions in pathological myopia, can also occur in eyes without high myopia [13]. V. Curtin and D. Karlin in 1970 were the first to propose a definition of “maculopathy” for myopia, which includes the following features: chorioretinal atrophy (CRA), central pigment spots, varnish cracks, posterior staphyloma and changes in the optic nerve head (ONH) [14 ]. Later, T. Tokoro [15] proposed a new classification of maculopathy in myopia, dividing lesions into four categories: mosaic fundus, diffuse CRA, focal CRA and macular hemorrhages. M. Avila et al. [16] developed a classification that divided retinopathy in myopia depending on severity: M0 - normal appearance of the posterior pole; M1 - choroidal blanching; M2 - M1 + addition of posterior staphylomas; M3 - M2 + adding varnish cracks to existing changes; M4 - M3 + changes in the central zones, including deep choroidal atrophy (severe); M5 - M4 + presence of large areas of deep CRA and scleral exposure. After B. Curtin and M. Avila, other researchers defined pathological myopia as “changes typical of myopia” without specific specifications. Some authors identified “degenerative myopia” with a myopic refraction of at least -6.0 diopters and atrophic changes associated with stretching of the macula [17]. T. Asakuma defined retinopathy in myopia as “the presence of at least one of the following features: diffuse CRA in the posterior pole, focal CRA, lacquer cracks or macular atrophy” [18]. Retinopathy in myopic eyes with pathological myopia, according to J. Vongphanit et al., includes staphyloma, varnish cracks, Fuchs' spot and chorioretinal thinning or atrophy [19]. The lack of a unified classification makes it impossible to directly compare or combine data from different studies to assess prevalence, incidence, and characterization of changes. K. Ohno-Matsui et al. defined pathological myopia as a condition in which patients are diagnosed with CRA, and created a classification system for pathological myopia, identifying 5 categories (from 0 to 4): 0 - no myopic lesions of the retina; 1 - mosaic fundus only; 2 — diffuse CRA; 3 - focal CRA; 4 - macular atrophy [20]. Three additions to these categories were made, denoted by a plus sign: (1) varnish cracks, (2) neovascular membranes, (3) Fuchs' spot. These 3 lesions are strongly associated with central vision loss, but they do not fit into any specific category and can develop in myopic eyes secondary to any of the categories of maculopathy described above. Pathological myopia is defined as one of the categories of this new classification, and if additional changes are present, a “plus” is indicated or an indication of posterior staphyloma is given [7]. E.S. Avetisov and L.P. Flick established a close relationship between the state of visual functions and the stage of fundus changes in high myopia and proposed a classification in which 5 stages reflect the degree of not only clinical, but also functional disorders [21]. Over the past two decades, advances in imaging technologies such as optical coherence tomography (OCT) and three-dimensional magnetic resonance imaging (MRI) have greatly enhanced our understanding of ocular complications associated with high myopia. However, there is a lack of information about the causes of these lesions, making it difficult to develop therapeutic interventions to reduce or prevent the development of these complications. High-resolution OCT in vivo allows assessment of optic nerve and macular lesions, as well as conditions such as traction syndrome [22] and domed macula [23], found in high myopia. The likelihood of developing these complications in pathological myopia in young people and their impact on vision and social adaptation increase the significance of this problem [7]. Effective treatment is available only for selected pathological changes, such as choroidal neovascularization and traction syndrome, and there is currently no available, effective restorative treatment for patients with progressive visual deterioration associated with the development of CRA or optic neuropathy.
Prevention
To reduce the risk of high myopia, you should adhere to the following recommendations:
- Organize the correct regime of visual stress: provide rest for the eyes every 40 minutes - an hour of working at the computer, small parts, and machine tools. This must be done when driving or reading for a long time.
- Provide good lighting during the day and in the evening. Try not to read while lying down or in the dark.
- Avoid deficiency of vitamins and minerals necessary for the functionality of the visual system: vitamin A, zinc, magnesium. Provide a balanced diet and take multivitamin complexes as prescribed by a specialist in courses.
- If you have a family history, visit your ophthalmologist more often for a preventive eye examination and early diagnosis of myopia.
- If you have any degree of myopia, monitor your indicators. With a high degree of myopia, you should not abuse alcohol or visit the sauna or bathhouse. Intracranial, arterial and intraocular pressure should be monitored and excessive physical and emotional stress should be avoided.
Limitations for complex myopia
High myopia often becomes a contraindication to military service and donation. A person may have difficulty obtaining a driver's license, lifeguard license, and similar statuses.
High myopia can cause blindness, which is the basis for receiving a disability group:
- first for partial or complete blindness;
- the second for poor vision, which makes it difficult to perform social and everyday functions;
- the third with a moderate decrease in visual acuity and the need for social protection of the person.
Complex myopia itself significantly increases the risk of retinal detachment, and alcohol abuse, visiting a bathhouse or sauna, attractions, surges in blood or intracranial pressure, and heavy physical and emotional stress can aggravate the situation. Therefore, people with a high degree of myopia need to exercise caution and avoid hazardous activities.
Having complex myopia, you need to maintain visual hygiene and constantly monitor the condition of the retina. When myopia stabilizes, surgical treatment is recommended, since severe visual impairment reduces the quality of life and imposes many limitations. High myopia is a constant risk, so it is always better to take care of your eye health.
Sources used:
- Kvasova M. D. Vision and heredity. - Moscow / St. Petersburg: Dilya, 2002.
- Radical restoration of vision. The power hidden in your eyes / R.M. Kaplan. - M.: IPL, 2021.
- The most important things about glaucoma, cataracts and other age-related eye diseases / I.Yu. Isaeva. - M.: Vector, 2014.
- Therapeutic exercises for the eyes. The latest developments of the American Vision Institute / Stephen Biresford et al. - M.: Potpourri, 2013.
- Sherwin, Justin (25 October 2011). “Lack of outdoor play linked to short-sighted children.” BBC News.
Useful video
Risk factors for the occurrence and progression of myopia in children and adults. Exercises to relax your eyes.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 2 ratings, average: 4.50 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.