What is sclera
The sclera is the membrane of the eye that performs a supporting and protective function. The thickness of this shell differs in different areas. In the equator zone it is approximately 0.4 mm, and in the area of the cornea and optic nerve head its thickness reaches 0.8 mm. The sclera is quite resistant to the negative effects of external factors. But even on this shell there are areas of thinning that can be injured under certain conditions.
There are very few blood vessels in the sclera. But vessels pass through it and go to the choroid from the inside. The outside of the sclera is covered with a special loose layer, which ensures good mobility of the eyeball in the orbit. But there is almost no innervation here.
The eye muscles, which are responsible for the movements of the eyeball, are attached to the sclera. The tunica albuginea protects the visual organ from mechanical injury.
There are several congenital and acquired diseases of the sclera that affect the quality of vision.
Signs and symptoms of scleral injection
Injection of the sclera always occurs with a number of characteristic symptoms. First of all, it is immediately noticeable that the white of the eye is very red. But besides this, other signs of inflammation are observed:
- There is pain in the eye of varying intensity. It can be either light and almost invisible, or shooting. Often the pain radiates to the temples, eyebrows and lower jaw.
- Pain when moving the eyeballs.
- Sensation of a foreign body in the eyes. A person has the feeling that sand is poured onto the mucous membrane.
- Tearfulness and photophobia.
- The eye appears red and swollen.
- If you look closely at the eye, you can see yellowish areas and dilated blood vessels.
- The eyelids are very swollen, with palpation the pain noticeably intensifies.
With scleritis, protrusion of the eyeball is often observed, the visual organ becomes as if bulging.
With scleritis, a decrease in visual acuity is almost always observed, which is explained by impaired blood circulation in the tissues.
Scleral vascular injection
The whites of the eyes turn red due to dilation of blood vessels in various structures of the eyeball.
In ophthalmology, the overflow of capillaries with blood is called injection.
The sclera is colored red or purple. The condition occurs as a symptom of infectious, viral diseases, injuries. Treatment depends on the cause of the redness.
Causes of scleral injection
Injection of the sclera causes:
- attack of glaucoma;
- infections;
- conjunctivitis;
- allergy;
- dryness;
- inflammation of the choroid: iridocyclitis, uveitis;
- inflammation of the cornea: keratitis;
- a tumor of the orbit that prevents the outflow of venous blood;
- allergy;
- hemorrhage after a blow, fracture of the base of the skull, orbit;
- measles;
- coughing attacks with whooping cough.
Rarely, congestive injection of the eyeball occurs in newborns with congenital glaucoma.
Kinds
Injections are classified according to the affected vessels in the structural elements of the eye.
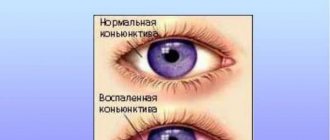
Conjunctival
Superficial hyperemia occurs in the outer membrane - the conjunctiva. Signs:
- short vessels do not touch the iris;
- the red color on the sclera fades closer to the center;
- as they move away from the cornea, the capillaries become wider;
- the branched blood network is clearly visible.
The vessels move along with the conjunctiva. Blood is retained and refills them when pressed.
Pericorneal
Deep or ciliary injection occurs from dilatation of the ciliary vessels of the looped network. Differences from surface form:
- long, wide capillaries reach the iris;
- purple, lilac blurry rim around the cornea;
- the vessels do not move;
- the movement of blood during compression is not traced.
The matte episcleral tissue hides individual parts of the vascular network, so the dark edging appears continuous. The width and color intensity of the injection ring depends on the thickness of the sclera and the stage of inflammation.
Mixed
Simultaneous dilatation of deep and superficial vessels caused by inflammation of the cornea.
Scleral
The injection affects the scleral, episcleral circulatory network. Signs:
- swelling of the sclera;
- blue, purple tint;
- lack of blood movement in the vessels during compression.
By nature it is divided into diffuse and limited.
Diagnostics
The degree of blood circulation in the vascular network is determined with a glass rod. The instrument is used to press the affected area and move the surface layer of the eyeball. During the procedure, immovable deep ones are visible under the movable upper vessels.
To determine the type of injection, a test is done with a solution of adrenaline, which is instilled into the eyes. Reaction on the sclera with different types of redness:
- disappearance of hyperemia after 2 minutes - conjunctival;
- lack of reaction - deep;
- narrowing of individual areas of the vascular network - mixed.
Dilatation of superficial vessels occurs with conjunctivitis. Uveitis, keratitis, and iridocyclitis cause a pericorneal appearance.
Studying the patient's medical history will help clarify the origin of the injection. Redness is caused by infectious respiratory diseases and inflammation of the cranial nerves.
Since vascular redness is caused by diseases of various etiologies, additional research is needed:
- biomicroscopy - the eye is examined with a slit lamp, in the light of which pathologies in the structure of the circulatory network are visible through the microscope;
- tonometry - high eye pressure dilates blood vessels, the procedure will determine glaucoma;
- fluorescein angiography - contrast injected into a vein will show changes in the vascular system on ultrasound;
- MRI - the affected area can be seen on a three-dimensional image of a tomograph.
Ophthalmoscopy and examination of the fundus are not informative, as they show the inner chamber of the eye, the retina.
Treatment
The main therapy is aimed at eliminating the primary disease and includes taking antibiotics and antihistamines. Injection caused by bacteria, viruses, goes away after treatment with eye drops:
- Albucid is an antibacterial drug for the treatment and prevention of inflammation of the conjunctiva, cornea, and eyelids;
- Ophthalmoferon - a drug with diphenhydramine and interferon acts as an anesthetic and promotes regeneration;
- Oftan Dexamethasone - relieves inflammation in keratitis, blepharitis, allergies;
- Ciprofloxacin is a universal antimicrobial agent.
Vasoconstrictor drops are used after making an accurate diagnosis:
- Visine - used for red eyes caused by external factors;
- Okumetil - the main component tetrazoline is supplemented with linden and chamomile extract to soothe the mucous membrane;
- Afrin - indicated for superficial injection caused by allergies;
- Visomitin - stimulates the formation of the tear film on the surface of the eye.
Redness caused by dryness can be relieved with artificial tears.
Was the article helpful?
Rate the material on a five-point scale!
( 3 5.00
Source: https://proglazki.ru/bolezni/inektsiya-sosudov-skler/
When does it occur
The causes of scleritis are quite varied. The following diseases and conditions can provoke dilation of blood vessels:
- Chronic tuberculosis.
- Syphilis.
- Chronic rheumatoid arthritis.
- Ankylosing spondylitis.
- Systemic lupus.
- Sarcoidosis.
- Corneal ulcer.
- Allergic reactions.
- Various infectious diseases.
Diseases in which metabolism is disrupted can also provoke scleritis. These also include diseases of an endocrinological nature. Inflammation of the sclera can be caused by various injuries to the visual organs. Redness is often observed in the postoperative period, after eye surgery.
In rare cases, the development of scleritis is associated with the entry of pathogenic fungi into the visual organs.
Causes of scleral icterus in humans
You may notice that when examining a patient, doctors always pay attention to the color and condition of the eye membranes. The interest of doctors is due to the fact that some diseases are characterized by signs that manifest themselves in changes in the color of the sclera (proteins). The color of the protein membrane changes as a result of congenital or acquired anomalies. More often in everyday life, icterus (yellowness) of the sclera occurs. The development of the anomaly is associated with a high level of bilirubin in the blood. Jaundice coloration is expressed in a faint shade or acquires a bright color of the protein shell.
Diagnostic measures
Diagnostic measures consist of studying the patient’s complaints and thoroughly examining him. In many cases, this allows the disease to be diagnosed. Additionally, a number of instrumental studies are prescribed to help confirm the diagnosis. In some cases, the doctor gives a referral for an ultrasound of the visual organs and computed tomography.
If there is a suspicion that scleritis has become a complication of some systemic disease, then a full examination and subsequent treatment are recommended.
Consequences and prevention
If scleritis is left untreated for a long time or is treated incorrectly, this leads to a number of serious complications:
- If the cornea is involved in the inflammatory process, keratitis may develop.
- If the iris and ciliary body are affected, iridocyclitis may begin.
- In some cases, suppuration begins, this indicates an abscess in the sclera.
- Secondary glaucoma may begin.
- Tissue healing with scleritis leads to the formation of a scar, which, in turn, leads to astigmatism.
- The nutrition of the eye tissues is disrupted, which leads to clouding of the cornea and impaired visual acuity.
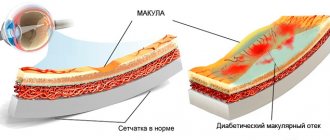
- Swelling and even detachment of the retina may occur.
Prevention of injection of scleral vessels comes down to timely treatment of infectious and ophthalmological diseases. You need to strengthen your immune system, for this you should eat well, exercise and walk a lot in the fresh air. Do not forget that scleritis can be caused by vascular diseases and metabolic disorders. To avoid vision problems, it is necessary to promptly treat all chronic diseases.
Source: oculistic.ru
Treatment
Scleritis requires complex treatment, which may include a number of medications and physiotherapeutic procedures. The patient may be prescribed the following medications:
- Broad-spectrum antibacterial drugs. They are prescribed only after the pathogen has been accurately identified. Antibiotics are prescribed for a course of at least 5 days.
- For tuberculosis, complex treatment is indicated, using various antimicrobial drugs and antibiotics.
- For rheumatism and other similar diseases, hormonal drugs and cytostatics are prescribed.
- Anti-inflammatory drugs, both local and systemic, are indicated.
- Complexes of vitamins and minerals are prescribed. It is also recommended to eat a lot of fresh vegetables, fruits and herbs.
All medications are taken in a course of at least a week. Anti-inflammatory eye drops are prescribed for a course of about a month. After treatment, the doctor conducts a re-examination to evaluate the effectiveness of the therapy.
Physiotherapeutic procedures are recommended after the patient's condition has stabilized. Most often, electrophoresis with various medications and UHF is prescribed. Such procedures are not prescribed in the acute phase of the disease.
In particularly difficult cases, when the deep layers of the sclera are damaged, surgery may be recommended. Surgery cannot be avoided if there is a scleral abscess, as well as if the iris and cornea are severely damaged.
If the sclera is very thin, then a sclera transplant is required. In cases where the inflammatory process has severely affected the cornea, a cornea transplant is also required. The most successful scleral and corneal transplant operations are carried out in Israel.
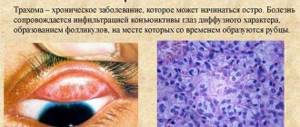
Scleritis
Scleritis is an inflammatory process that affects the entire thickness of the outer connective tissue membrane of the eyeball. Clinically manifested by hyperemia, vascular injection, edema, pain on palpation of the affected area or movements of the eyeball. Diagnosis of scleritis comes down to an external examination, biomicroscopy, ophthalmoscopy, visometry, tonometry, fluorescein angiography, ultrasound (US) in B-mode, computed tomography. Depending on the form of the disease, the treatment regimen includes local or systemic use of glucocorticoids and antibacterial agents. With purulent scleritis, opening the abscess is indicated.
Scleritis is an inflammatory disease of the sclera, characterized by a slowly progressive course. Among all forms, anterior scleritis is the most common (98%). Damage to the posterior parts of the sclera is observed in only 2% of patients. Options for the course of pathology without necrosis predominate over necrotizing ones, which is associated with a favorable prognosis. In rheumatoid and reactive chlamydial arthritis, diffuse variants of the disease are common. In 86% of cases of ankylosing spondylitis, nodular scleritis is diagnosed. In 40-50% of patients, pathological changes in the sclera are combined with damage to joints of inflammatory origin, and in 5-10% of cases, arthritis is accompanied by scleritis. The disease is more common in females (73%). The peak incidence occurs between the ages of 34 and 56 years. In children, the pathology is observed 2 times less often.
Scleritis
The etiology of scleritis is directly related to a history of systemic diseases. Triggers of scleral damage are rheumatoid arthritis, Wegener's granulomatosis, juvenile idiopathic, reactive chlamydial or psoriatic arthritis, polyarthritis nodosa, ankylosing spondylitis and polychondritis, characterized by a relapsing course. Less commonly, this pathology develops in the postoperative period after surgical removal of pterygium or traumatic injury. Clinical cases of infectious scleritis in patients with a history of vitreoretinal surgery are described.
Scleritis of infectious etiology is often caused by dissemination of the process from the area of ulceration on the cornea. Inflammation of the paranasal sinuses can also be a source of infection. The most common causative agents of the disease are Pseudomonas aeruginosa, Varicella-Zoster virus and Staphylococcus aureus. In rare cases, scleritis is of fungal origin. Drug-induced damage to the sclera more often develops when taking mitomycin C. Risk factors are a history of osteoarticular forms of tuberculosis, systemic inflammatory diseases.
From a clinical point of view, ophthalmology distinguishes anterior (non-necrotizing, necrotizing), posterior and purulent scleritis. Non-necrotizing lesions of the sclera can be diffuse or nodular. Necrotizing may or may not be accompanied by an inflammatory process. In some cases, the course of scleritis is characterized by short-term self-terminating episodes. At the same time, the pathological process in the sclera provokes its necrosis with the involvement of the underlying structures. This disease is characterized by an acute onset; indolent variants are less common. With diffuse scleritis, the entire anterior part of the outer connective tissue membrane of the eyeball is involved in the inflammatory process. Nodular lesions are accompanied by decreased visual acuity.
Anterior scleritis is characterized by a slowly progressive course. This form is accompanied by binocular damage to the organ of vision. Patients note severe pain when touching the area of edema projection, photophobia. The long course of the disease leads to damage to the sclera along the circumference of the limbus (ring-shaped scleritis) and the occurrence of severe keratitis, iritis or iridocyclitis. With purulent scleritis, rupture of the abscess membranes is possible, which leads to the development of iritis or hypopyon.
With necrotic damage to the sclera, patients note increasing pain, which later becomes constant, radiating to the temporal region, brow ridge and jaw. The pain syndrome is not relieved by taking analgesics. Necrotizing scleritis is complicated by perforation of the sclera, endophthalmitis or panophthalmitis. In the posterior form of the pathology, patients complain of pain when moving the eyeball and limited mobility. Postoperative scleritis develops within 6 months after surgery. In this case, an area of local inflammation is formed, which is replaced by necrosis. A decrease in visual acuity is observed only when the inflammatory process spreads to the adjacent structures of the eyeball or the development of secondary glaucoma.
Diagnosis of scleritis includes external examination, biomicroscopy, ophthalmoscopy, visometry, tonometry, fluorescein angiography, B-mode ultrasound (US), computed tomography. An external examination of patients with anterior scleritis reveals swelling, hyperemia and vascular injection. The area of edema has defined boundaries. On palpation examination, pain is noted. Carrying out biomicroscopy for “jellylike” scleritis allows us to identify the area of overhang of the chemosed conjunctiva over the limbus. This area has a red-brown tint and a gelatin-like consistency. Infiltrates with pronounced vascularization can be found on the surface of the cornea. The method of biomicroscopy with a slit lamp for diffuse scleritis determines the violation of the physiological radial direction of the vascular pattern. In the nodular form, viziometry indicates a decrease in visual acuity.
With purulent scleritis, external examination reveals a purulent infiltrate and vascular injection. Damage to the posterior parts of the sclera is accompanied by swelling of the eyelids, conjunctiva and slight exophthalmos. The ophthalmoscopy method is used to determine prominence of the optic disc, subretinal lipid exudation, retinal and choroidal detachment caused by the accumulation of exudate. Ultrasound in B-mode indicates thickening of the posterior part of the outer connective tissue membrane of the eyeball, accumulation of exudate in Tenon's space. Changes in scleral thickness can also be confirmed using CT.
In case of necrotizing scleritis, fluorescein angiography is used to determine the tortuous course, areas of vascular occlusion, and avascular zones. Carrying out biomicroscopy with a slit lamp allows you to visualize necrotic changes in the sclera and ulceration of the adjacent conjunctiva. The dynamics reveal an expansion of the necrosis zone. Tonometry in patients with scleritis often reveals an increase in intraocular pressure (more than 20 mm Hg).
The treatment regimen for scleritis includes the local use of glucocorticoid and antibacterial drops for instillation. If the disease is accompanied by increased intraocular pressure, then the therapy complex must be supplemented with topical antihypertensive drugs. The course of treatment includes taking non-steroidal anti-inflammatory drugs. If they are intolerant, it is recommended to prescribe medications from the group of glucocorticosteroids. For scleritis without necrotic lesions, glucocorticoids and antibacterial drugs must be administered in the form of subconjunctival injections. An alternative to this method of administration is taking long-acting forms of glucocorticoids.
With the development of scleral necrosis, combination therapy with glucocorticosteroids and immunosuppressants is indicated. In cases of an allergic reaction, antiallergic and desensitizing drugs are used in parallel with these medications. With the purulent form of scleritis, treatment tactics boil down to massive antibacterial therapy. In this case, oral and subconjunctival routes of administration of drugs from the group of fluoroquinolones, aminoglycosides and semi-synthetic penicillins are used. An additional method of administration is electrophoresis. If there is no effect of drug therapy, surgical opening of the abscess is indicated. Also, the treatment regimen should include drugs to treat the underlying pathology against which scleritis developed. If the etiological factor is Mycobacterium tuberculosis, anti-tuberculosis drugs for topical use are considered as auxiliary.
Forecast and prevention of scleritis
Specific prevention of scleritis has not been developed. Nonspecific preventive measures boil down to timely treatment of the underlying pathology, prevention of inflammation of the paranasal sinuses (sinusitis), compliance with the rules of asepsis and antisepsis during surgical interventions. Patients with a history of systemic diseases need to be examined by an ophthalmologist 2 times a year. The prognosis for life and ability to work depends on the timeliness of diagnosis, the adequacy of treatment, the type of pathogen in the infectious lesion and the form of the disease. The most favorable option is diffuse forms of the disease. Scleritis caused by Pseudomonas aeruginosa often has a poor prognosis.
www.krasotaimedicina.ru