For the normal functioning of the organ of vision, many special components are necessary. The orbicularis oculi muscle is one of these. It differs from other groups of muscle tissue in its location, fiber thickness and versatility. Without this element of the visual organ, a person is unable to fully see, so it is important to know how this component works, its functions and possible pathologies.
Closing the eyes. Functional muscle tests
- With central paresis of the facial nerve, the orbicularis oculi muscle, innervated centrally and bilaterally, is affected to a lesser extent.
- Patients with orbicularis oculi paresis are unable to close the eye on the affected side (lagophthalmos). When trying to close the eye, the eyeball rolls upward (Bell's sign).
Issues and comments
- When you close your eyes, the orbital part of the orbicularis oculi muscle is mainly activated; When the eyelids close slightly, the eyelid part is mainly activated.
- Wrinkles formed by the orbicularis muscle at the outer corner of the eye can become permanent with age; in this case they are called "crow's feet".
Source
Causes and signs of muscle pathologies
When the functions of the CMG are impaired, various diseases develop - lagophthalmos, blepharospasm, hypertonicity of the lower edge of the muscle.
Lagophthalmos is incomplete closure of the eyelids even during sleep. Causes: paresis of the facial or trigeminal nerve at the site of innervation of the orbicularis oculi muscle. There is a downward shift of the lower eyelid, the conjunctiva dries out. Symptoms are pain, burning, increased tearfulness.
Blepharospasm is a periodic uncontrolled tension of the CMG. The exact reasons for the development of pathology are unknown. Signs are involuntary closing of the eyes, contraction of muscles; a person cannot stop this process on his own, since the muscle does not respond to commands from the brain.
With increased tone of the edge of the orbicularis oculi muscle, bags form under the eyes. The cause of edema is not associated with overwork or dysfunction of internal organs. Expression wrinkles occur due to an increase in the size of muscle fibers. The reason is prolonged eye work without rest and special exercises to maintain tone.
To confirm the diagnosis, the ophthalmologist prescribes ultrasound, MRI, CT, and electroneuromyography. Treatment is carried out using special gymnastics, physiotherapy, and massage. In the presence of infectious pathologies, antibacterial or antiviral drugs are prescribed.
Orbicularis oculi muscle insertion site
a) Internal rectus muscle of the eye
. The internal rectus muscle arises from the ring of Zinn, runs forward along the medial wall of the orbit and is attached to the nasal surface of the sclera 3-6 mm posterior to the limbus. Because the internal rectus muscle runs close to the medial wall of the orbit, it can be damaged during operations on the ethmoid sinuses. The width of the attachment of the internal rectus muscle is 9-11 mm, the length of its tendon is 4-6 mm. The total length of the muscle is 40 mm.
The internal rectus muscle is innervated by the inferior branch of the third cranial nerve, which enters the muscle through its internal surface at the border of the middle and posterior thirds. In the primary position, the muscle comes into contact with the eyeball in an arc approximately 5 mm long.
b) External rectus oculi muscle
. The external rectus muscle extends from the ring of Zinn for 40 mm along the lateral wall of the orbit until its very long (8-10 mm) and thin tendon attaches to the temporal surface of the sclera 6-9 mm from the limbus. The width of the attachment varies from 7 to 9 mm. In the primary position, the muscle comes into contact with the eyeball in an arc approximately 7-8 mm long. Innervation of the external rectus muscle is carried out by the VI cranial nerve.
c) Superior rectus oculi muscle
. The superior rectus muscle starts from the ring of Zinn and runs for 40 mm to its attachment to the upper surface of the sclera, 7-9 mm from the limbus. The width of the attachment varies from 9 to 12 mm, the line of attachment is beveled in such a way that its medial edge is located closer to the limbus, and the lateral edge is shifted back. The length of the tendon is approximately 6 mm. The superior rectus muscle is innervated by the superior portion of the third cranial nerve. The muscle stretches forward, outward and upward and forms an angle of 23° with the anterior-posterior axis of the eyeball. This angle explains the different movements of the eye during contraction of the superior rectus muscle in different initial positions of the eye in the horizontal plane; only upward movement occurs when the eyeball is abducted by 23°.
Theoretically, with the eyeball adducted to 67° (in the horizontal plane the eye can typically deviate 50° to each side), contraction of the superior rectus muscle would cause only intrusion. In the primary position, contraction of the superior rectus muscle causes upward movement of the eyeball, intrusion and slight adduction; the more the eyeball is adducted, the more the superior rectus muscle becomes an adductor and incycloductor, and the less it becomes an elevator.
The superior rectus muscle is closely related to the levator palpebrae superioris muscle through a common facial sheath. Because of this connection between the levator and superior rectus muscles, hypogropia is often accompanied by pseudoptosis. Extensive recessions or resections of the superior rectus muscle may cause upper eyelid retraction or ptosis, respectively.
On topic: Massage for the muscles of the uterus
d) Inferior rectus oculi muscle
. The inferior rectus muscle extends forward for 42 mm from the apex of the orbit to its attachment to the sclera 6-8 mm from the lower edge of the limbus. The length of its tendon is approximately 6 mm, width - 8-10 mm. The attachment to the sclera is also beveled, the difference in distances from the limbus of the anterior medial and posterior lateral edges is 2 mm. Since the direction of the muscle forms an angle of 23° with the anterior-posterior axis of the eyeball, its contraction in the position of abduction of the eyeball by 23° causes only lowering. If the eye was adducted to 67°, only adduction would be observed; in the position between these two points, the inferior rectus muscle performs the functions of lowering, adducting and ex-cyclotorsion. The inferior rectus muscle is innervated by the inferior portion of the third cranial nerve.
The inferior rectus muscle is connected to the cartilage of the lower eyelid through the capsulopalpebral ligament and the lower eyelid retractors. Recession of the inferior rectus muscle may cause widening of the palpebral fissure; resections can lead to elevation of the lower eyelid and narrowing of the palpebral fissure. The capsulopalpebral fascia of the lower eyelid begins 5 mm from the insertion of the inferior rectus muscle, splits, surrounds the inferior oblique muscle, converges in front of it and forms the ligament of Lockwood. Anterior to Lockwood's ligament, the fascia thickens and forms the inferior tarsal muscle, which attaches to the cartilage of the lower eyelid.
e) Superior oblique muscle of the eye
. The superior oblique muscle originates from the periosteum of the lesser wing of the sphenoid bone above the ring of Zinn. It runs in a superomedial direction parallel to the medial wall of the orbit in its own compartment of fatty tissue and reaches the trochlea after approximately 40 mm. The trochlear is a saddle cartilage attached to the frontal bone in the superonasal part of the orbit. The superior oblique tendon bends and changes its direction back at an angle of 55° to the medial wall of the orbit. The superior oblique muscle has the longest tendon of all the extraocular muscles. It starts 10 mm behind the block, its length is approximately 18-20 mm. The part of the tendon that goes around the trochlea goes under Tenon’s capsule 2-3 mm nasal to the medial edge of the superior rectus muscle and passes under it 3-5 mm posterior to the medial edge of its attachment when the eyeball is in the primary position. If the eye is turned inferiorly, the superior oblique tendon is displaced and is located 8 mm posterior to the insertion of the superior rectus muscle.
Passing under the superior rectus muscle, the superior oblique muscle tendon expands like a fan and attaches to the sclera along a concave line of 10-12 mm. The anterior end of the attachment is 4 mm posterior to the lateral end of the attachment of the superior rectus muscle, and the most posterior portion of the tendon ends 5-6.5 mm from the optic nerve, on the temporal side of the superior temporal vorticosis vein. Because of this wide attachment, the eye will rotate downward from a 55° adduction position, and from a 39° abduction eye position, contraction of the muscle causes incyclotorsion. In the primary position, muscle contraction causes a combination of incyclotorsion, lowering and slight abduction. The width and angle of insertion of the superior oblique muscle are extremely variable. In addition, abnormalities of the superior oblique tendon are common. It may be excessively long or stretched, have an abnormal direction, be absent, or be abnormally attached to the sclera nasal to the superior rectus muscle or to Tenon's capsule.
The superior oblique muscle is innervated by the fourth cranial nerve. A peculiarity of the course of the nerve is that the nerve penetrates the muscle not from the internal, but from the orbital surface of the muscle. The anterior half of the superior oblique muscle tendon that wraps around the trochlea has the greatest intrusion effect. The rear half is mainly used for lowering. This “division of labor” of the fibers of the superior oblique muscle allows for the intervention described by Harada and Ito, in which, in order to correct excyclotorsion, the anterior half of the tendon was moved forward and the intorsion function of the muscle was enhanced. Conversely, selective tenotomy of the superior oblique muscle selectively weakens its vertical action. With these techniques, A-pattern deviations can be treated without causing torsional diplopia.
The posterior edge of the superior oblique tendon is closely connected to the inferior surface of the overlying superior rectus muscle by thin transparent adventitial connections (superior oblique frenulum). The location of this frenulum is optimal to connect the movements of the superior oblique and superior rectus tendons; As a result, when the superior rectus muscle recedes, the superior oblique tendon moves posteriorly. The frenulum limits the amount of recession during suspension surgery, since in large recessions (10-14 mm), if the frenulum remains intact, the superior rectus muscle sags.
On the subject: What is the topography of skeletal muscles
e) Inferior oblique muscle of the eye
. The inferior oblique muscle arises from the periosteum of the maxilla, immediately behind the edge of the orbit and lateral to the lacrimal fossa, in the anteronasal part of the lower wall of the orbit. The tubular muscle passes laterally and posteriorly under the inferior rectus and attaches to the sclera under the external rectus muscle in front of the macula, forming an angle of 51° with the anteroposterior axis of the eye in its primary position. Contraction of the inferior oblique muscle at a position of 39° relative to the anteroposterior axis would cause only extortion, and with adduction of 51° it would only cause elevation. In the primary position, contraction of the inferior oblique muscle causes excyclotorsion, elevation, and slight abduction.
The inferior oblique muscle pierces Tenon's capsule near the ventral surface of the inferior rectus muscle. Its length is 37 mm; the length of its short tendon is 1-2 mm. The inferior oblique muscle is innervated by the inferior branch of the third cranial nerve, which enters the muscle 14-15 mm from its insertion along the posterior lateral edge on its globular (scleral) side, accompanied by an artery and vein (neurovascular bundle) (Fig. 71.6). Parasympathetic innervation of the sphincter of the pupil and the ciliary muscle occurs through the same branch of the third cranial nerve as the innervation of the inferior oblique muscle. During operations on the lower wall of the orbit, these parasympathetic fibers can be damaged.
The neurovascular bundle of the inferior oblique muscle in the orbit runs straight, from the apex to the inferior oblique muscle, close to and lateral to the inferior rectus muscle. Its anterior part has a fibrocollagen capsule in which collagen fibers run parallel to the neurovascular bundle; fibrous bands extend back and connect the capsules of the inferior oblique and inferior rectus muscles. This structure has the character of a ligament. Stager described the neuro(fibro)vascular bundle of the inferior oblique muscle as an additional zone of fixation, which, after anterior transpositions and preequatorial recessions, becomes a functional insertion point for the inferior oblique muscle. The neurofibrovascular bundle holds the posterior portion of the inferior oblique muscle fixed in the orbit; after anterior transpositions, the function of elevating the eye by the inferior oblique muscle is limited due to its ligament-like qualities.
After cutting this bundle, the muscle sags forward; Total sub-Tenon's dissection of the muscle requires denervation.
g) Anatomical options
. Abnormalities of muscle and tendon structures have been described in cases of nonconjugate restrictive strabismus. These structures can be attached in various areas of the eyeball, around or directly to the attachment of the extraocular muscles. Strands of fibrous tissue have also been described. Patients with unusual strabismus should undergo radiation examination of the orbit. An attempt should be made to cut off abnormal structures; this usually brings good results and improves eye mobility.
Absence of the extraocular muscles occurs sporadically in the general population and can affect any muscle. Patients with craniosynostosis syndromes have a high incidence of absence and other abnormalities of the extraocular muscles, but they may also co-occur with other conditions. The abnormalities may affect one or both eyes or one or more muscles.
Anterior insertion of the internal rectus muscle.
Internal rectus muscle with two large anterior ciliary arteries.
a, b — Relationships between the superior rectus muscle and the tendon of the superior oblique muscle (view from the surgeon’s side). (A) The attachment of the superior oblique muscle is visible under the superior rectus muscle of the right eye (hooked). (B) The superior rectus and superior oblique muscles are placed on muscle hooks and a suture is placed on the nasal portion of the superior oblique tendon. c — Attachment of the inferior oblique muscle under the external rectus muscle (view from the surgeon). d — The attachment of the neurofibrovascular bundle to the lateral posterior edge of the inferior oblique muscle separated from the sclera is visible (view from the surgeon’s side).
a - The inferior rectus muscle and its relationship with the retractors of the lower eyelid, perforating Tenon’s capsule and attaching to the cartilaginous plate of the lower eyelid.. b - White fibrous cords marking the place of attachment of the orbital layer to the trochlea of the internal rectus muscle..
Source
Smile for your health!
The work of facial muscles is closely related to the activity of the brain. The richness of facial expressions indicates the active state of the nervous system. There is also a feedback: the activity of certain facial muscles activates certain areas of the brain. Therefore, smile more often, laugh, enjoy life, but do not get angry or sad, even if you have reasons for it. You will feel a surge of strength, a positive attitude towards current affairs, and a kind attitude towards others.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor of the Department of Human Anatomy of the RUDN University
Structure
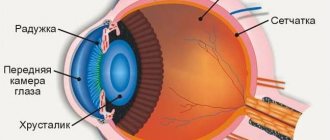
The functionality and structure of these amazing muscles should be studied in detail. The eyelids cover the outer part of the eyes and protect from external factors. Main functions:
- protection against the ingress of small particles and foreign objects;
- uniform distribution of tear fluid;
- responsible for moisturizing the cornea and conjunctiva;
- washes away small particles from the surface of the mucosa;
- protect eyes from drying out during sleep;
- are responsible for the blinking process.
The edges of the eyelids are 2 mm thick. The lower and upper eyelids close tightly when closing the eyes. Eyelashes grow on the smoothed anterior rib. The inner one is sharper and fits tightly to the eyeball. The intermarginal space is located along the length of the eyelids, between the anterior and posterior parts. The skin is thin, so it tends to gather in folds. When the eyes open, it folds inward with the help of the muscles that are responsible for raising the eyelids. This creates a deep crease. Another, less pronounced one is located on the lower eyelid.
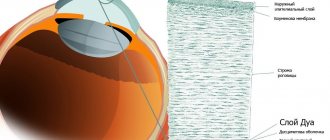
There is also a circular muscle, which is located under the skin in the orbital or palpebral part. In the process of closing the eyelids, both muscles contract. The dense tuft that emanates from the frontal origin of the maxilla is the internal ligament of the eyelid. It bifurcates and connects to the ends of the cartilage of the eyelids.
A set of exercises for the eyes by W. Bates
W. Bates was one of the first to develop eye exercises to stop the progression of myopia. The scientist named the main cause of myopia as overexertion, which occurs as a result of trying to look at objects distant from a person after prolonged stress on the visual organs, for example, after reading. Because of this, pressure on the eye caused by tension in the oblique muscles causes it to stretch. Complete relaxation, according to Bates, can be achieved through exercises that use the OM card. The card is a design resembling a sun with small triangular rays along the outer surface of the circle. In the center of the circle is a hieroglyph similar to the letters “O” and “M”. The hieroglyph is surrounded by other unusual symbols.
The following tasks are performed with the OM card:
1. Place the card at a distance of 30 cm to 3 m from your eyes. Focus on the center of the picture and slowly move your gaze along the hieroglyph. During the exercise, you will notice that the clearest and blackest point of the hieroglyph is the one to which your gaze is directed. You need to repeat the exercise 3 times. With each repetition, the hieroglyph will appear darker than at the very beginning. 2. The OM card should be placed from the eyes at a distance of 30 cm or 1.5 m. This time you need to look not at the hieroglyph, but at the rays of the sun, moving your gaze along them. In this case, movement along the segment is carried out by turning the head, not the eyes. At each ray you need to hold your gaze and blink lightly. Each ray should appear darker than the previous one. 3. Leave the OM card at the same distance from your face. Now focus on the circle and move your gaze around it while moving your head. After this, you need to close your eyes and continue moving in an imaginary circle. 4. For the fourth exercise, you will need a Sivtsev table with optotype letters to test visual acuity. It should be hung on a wall or cabinet at arm's length. Keep your gaze on the letters that are clearly visible. After this, dim the lights in the room. Take a book and read a few pages, holding the book 25 cm from your face. It must be difficult to read due to poor lighting. After this, you need to increase the brightness of the light again in order to read the letters on Sivtsev’s poster again. This exercise, according to Bates, improves visual acuity. 5. Read the vision test table while being at a distance of 3-5 m from it. Gradually you need to increase the distance between you and the table. Start at 3 meters and work your way up to 5 meters. 6. Another exercise can be performed directly on the street or in the passenger seat of a vehicle. You need to watch moving objects that rush towards you. The eyes should be relaxed, half-open.
Also, complete relaxation of the eye muscles can be achieved, as stated by Bates, using the following techniques:
1. Palming method, which consists of closing the eyes from direct light. 2. Rocking and moving method. This includes any exercise during which the gaze moves left and right.
Exercises with the OM card are aimed at normalizing central gaze fixation, while the other two techniques allow you to relax the eye muscles as much as possible. They can be performed alternately.
Not all ophthalmologists fully accept the complex developed by Bates, therefore it is not recommended to perform these exercises without examination by a doctor.
Functions
The circular muscles are an irreplaceable part of the visual apparatus, on which the functioning of the eyelids depends. They perform very important functions:
- responsible for the blinking process;
- active muscle is responsible for wakefulness;
- moisturize the mucous membrane;
- prevent drying of the cornea during sleep.
The condition of the eyelids is very important for healthy eyes. Control of the width of the palpebral fissures is also determined by them. Subject to various pathological diseases and processes. The most common is a pathology called ptosis. It can manifest itself in varying degrees of damage and cause severe complications.
During sleep, the eyes have the opportunity to relax and rest. The eyelids provide this rest. They control the distribution of tear fluid, moisturize the mucous membrane, and prevent drying out during sleep. In addition, they protect the eyes from small particles and foreign objects.
If unpleasant eye symptoms occur or occur against the background of endocrine or neurological diseases, then they must initially be cured. Drug therapy is prescribed by a doctor only after confirmation of the diagnosis. In addition, self-medication is prohibited.
Symptoms of pathologies of the orbicularis oculi muscle
Ptosis is a pronounced pathology, which is accompanied by drooping of the eyelid (mainly the upper one). In most cases, the pathology is unilateral. Bilateral lesions are rarely observed. Asymmetry of the eyelids not only causes an aesthetic defect, but can also impair vision. In a pronounced form, severe ophthalmological diseases can develop.
The muscle is attached to the orbit of the superior cartilage. The beginning is the area of the optic opening. It passes into a tendon, the width of which is much greater. Its anterior part is attached to the cartilage and goes to the orbicularis muscle. The fibers, which are located on the back, connect to the conjunctiva and pass into the upper fold.
The fibers located on the middle part of the tendon complete the structure of the muscle. The muscle that raises the eyelid is closely related to the levator muscle. It is located near its front end. In addition, this structure ensures the elevation of not only the eyelid, but also all its parts: cartilage, skin, conjunctiva, which passes into the upper fold.
The innervation of the middle part of the upper eyelid has smooth fibers. Therefore it is considered a sympathetic nerve. The posterior surface is completely covered with conjunctiva connected to cartilage. If the levator tone is normal, then the upper eyelid covers the cornea by about 2 mm. The function that is responsible for raising it is impaired with ptosis.
This ligament passes under the oblique muscle at the back. It then mixes with the fascia and covers the area above the eye. From the outside it is attached to the capsule of the lacrimal gland. The main function limits muscle displacement on the posterior side. This theory is confirmed by the localization of such functionality. When tense, the ligament supports the upper eyelid. If this function is not performed, ptosis will appear.
Clamps of the muscle located around the mouth
If we are talking about functional clamps in this area, then they occur quite often, but can still be corrected with diligence and the right approach. In contrast to organic lesions, when in 99% of cases it will not be possible to do anything.
The functional clamps of this area are directly related to the psycho-emotional state of a person, his dislike for anything in question. As a result, a person expresses a certain emotion with his lips: resentment, disappointment, disgust, and so on.