One of the reasons for decreased visual acuity is clouding of the internal refractive media.
If this occurs in the vitreous, vision may be reduced or remain normal.
This depends on the degree of spread of the pathological process and areas of accumulation of various fractions of substances. This condition should not be tolerated; it develops over time. The sooner therapy begins, the greater the patient’s chances of fully maintaining vision function.
Why does cloudiness occur?
There are many different reasons why vitreous opacities can develop:
- age over 50 years, at which physiological processes associated with the accumulation of various substances occur;
- severe myopia, in which the patient develops vision from -6 diopters;
- inflammatory conditions of the eyeball that develop periodically, becoming chronic;
- diseases spreading to the endocrine glands (hyperthyroidism, diabetes mellitus, pancreatitis);
- temporary disruption of the endocrine background, which occurs during pregnancy, adolescence, menopause, andropause;
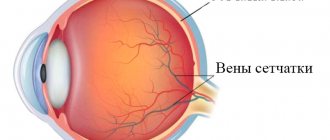
- pathological conditions of the microcirculation vessels of the eye, which develop due to systemic diseases (hypertension, atherosclerosis, coronary disease, vascular fragility);
- Excessive strain on the eyes, which occurs with frequent exposure to cramped spaces, prolonged use of a computer and other electronic devices;
- mechanical damage to any parts of the visual organs;
- lack of vitamins and other beneficial substances from food, which leads to hypovitaminosis or vitamin deficiency;
- stress, depression, neuroses, psychoses;
- the effect on the body of infections, viruses, fungi, toxins, especially if pathological processes occur in the organs of vision.
It is not enough for a doctor to simply clear the vitreous body of accumulated substances. He needs to identify the root cause to completely eliminate the risk of recurrence of the condition.
Functions
CT begins to work immediately after the birth of the fetus. The main functions of the vitreous body are:
- Maintaining correct eye shape.
- Ensuring the tone and incompressibility of eye tissue.
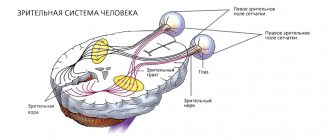
- The light-conducting and light-refracting function of the vitreous body is that it conducts light rays directly to the retina and then refracts them.
- Ensuring the normal position of the retina and lens.
- Nutritional function of ST.
- The outflow of intraocular fluid and maintaining a constant normal intraocular pressure is also a function of the vitreous body.
- Carrying out metabolic processes in the tissues of the eye.
Diagnostics
If the patient’s visual acuity has sharply decreased, or clouding occurs in only one or both organs of vision, it is recommended to consult an ophthalmologist. He will conduct several diagnostic tests to make a reliable diagnosis:
- Anamnesis collection. The doctor will ask the patient when vision loss began and whether there were such conditions in the past. The patient may complain of spots before the eyes, multiple opacities that progress over time.
- General inspection. If the pathological condition is at an early stage of development, no symptoms will be visually detected. In the presence of severe clouding of the vitreous body, the accumulated fractions of substances can transfer to the cornea, which causes white spots inside it.
- Visometry. This is a study using diagnostic tables. The more lines the patient sees in them, the better his visual acuity.
- Autorefractometry. This is a test that can be used to determine the refractive ability of the eyeball. The vitreous body refracts rays, transmitting them to the retina. If this structure is broken, the autorefractometer will show this data.
- Ultrasound examination of the eyes. Using the test, you can identify the shape of the eyeball and the condition of the intraocular elements.
- Optical coherence tomography. The patient sits in front of the tomograph and focuses his gaze on the mark. The device scans the organ of vision, producing layer-by-layer image results.
- Fundus examination. The patient is first instilled with Atropine or similar agents that dilate the pupil. The doctor determines the quality of the structural elements; vitreous opacities are always visible through examination.
Based on these data, it is possible not only to identify vitreous opacities, but also other pathological conditions of the eyeballs. Only after making a diagnosis can the doctor begin treatment.
Symptoms:
- floating opacities in the form of transparent or black dots, lines or figures with inertial movement, which arise when the eyes turn and settle, like “a mule in a glass of water.” Patients often describe their complaints as the appearance of “floaters” in their field of vision. Blurred vision does not affect vision; rather, it is irritating. They are clearly visible against the background of snow cover, a white wall, and a cloudless sky. Such complaints arise over time in almost all people.
- flashes or lightning that are clearly visible in a dark room. They are caused by the fact that when the vitreous body detaches from the retina, it stretches and stimulates the photoreceptors. Actually, the appearance of these complaints indicates the beginning of posterior vitreous detachment. Over time, the brain identifies these phenomena as additional and cuts off the unnecessary image.
Methods of therapy
The doctor selects the treatment method depending on the severity of the patient’s visual condition. There are several ways in which the eyeball can be treated conservatively. But the doctor can also choose surgical or laser therapy.
Treatment is not always carried out. Often the patient has a partial vitreous opacification that does not develop over time. But such patients need to periodically visit an ophthalmologist to determine the condition of the eyeballs. If the clouding develops and fills all structures, conservative and surgical therapy is necessary.
Conservative therapy includes the following types of drugs:
- medications that normalize the state of microcirculation of the blood vessels of the eyes (Emoxibel, Emoxipin), they are used in small courses to periodically stimulate the blood flow of the eyeball;
- medications that normalize blood circulation in the central nervous system (Cinnarizine), they are prescribed both orally and intravenously; in addition, they promote the resorption of thromboaggregates;
- drugs that prevent the accumulation of insoluble protein fractions in the refractive structure of the eyes (Quinax);
- local vitamin therapy using medicinal drops, which enhance metabolism, leading to increased regenerative capacity (Okovit, Taufon).
Even with the use of conservative therapy, the patient’s condition progresses, the doctor immediately performs surgery to eliminate opacities in the vitreous body:
- Vitreolysis. This is a laser procedure that is aimed at eliminating vitreous opacities. The technique is used for patients who have severe myopia and a high risk of retinal detachment. Anesthetics are first instilled into the patient's eyes. The entire procedure is performed without general anesthesia. Using a laser, areas of accumulation of fractions of various substances are removed. But the technique is applicable only if the clouding does not form strongly and is focally distributed throughout the vitreous body.
- Vitrectomy. This is a major surgical procedure in which the vitreous humor is removed completely or partially. The first option is suitable for those people whose clouding has spread throughout the entire structural element of the eyes. The internal structure of the vitreous body is easily replaced by an artificial environment that fully corresponds to its own element. Partial removal of the vitreous is only suitable if the clouding has developed in a certain area and greatly reduces visual acuity. With partial removal, the doctor does not need to replace the fluid with an artificial medium; it will recover on its own, since the eye medium circulates constantly.
Most often, silicone oil, saline solution, and gas elements are used to replace the structure of the vitreous body. They are identical in composition and do not form a negative reaction of the immune system, which can lead to an inflammatory condition.
Gradually, the fluid necessary to replace the internal component of the vitreous body is replaced by the eye’s own secretion. This is due to the fact that fluid in the organs of vision constantly circulates. But the effect is observed only when using saline solution or gas bubbles. If the doctor chose silicone oil, the patient will need a second operation after 5 years.
Role of ST
A substance such as the vitreous body is already actively functioning in the fetus, because the nutrition of the lens and the anterior segment of the eye occurs due to the hyaloid artery passing through the VT.
After birth, this artery gradually reduces and disappears. Sometimes it may remain in the form of residues, like tender cords. The structure and functions of the vitreous body in physiological terms are such that the vitreous in humans and some animals is a very active tissue, which is richly supplied with blood, with intensive nutrition and metabolism.
It is not for nothing that ST is produced in the form of a drug and is classified as a biostimulant. After the birth of a person, the CT becomes an inert tissue, and the rate of exchange in it decreases, although processes do occur. The ST itself is fed from the vessels of the retina and uveal tract.
In case of injury, it does not regenerate and is partially replaced by intraocular fluid.
TS does not have independent diseases; changes in it are secondary. But at the same time it can store exudates and blood.
The consistency of ST is not the same everywhere: in the central part it is more liquid. Although outwardly it appears transparent, in the light of a slit lamp the gel glows, and this indicates that its substance is colloidal.
The colloidal micelles appear to be arranged in parallel and appear as thin wavy stripes of light and darker colors. They resemble moire ribbons that hang like a curtain and slowly sway with the movements of the eyeball.
Prevention
There are many different prevention methods that can be used to prevent the formation of cloudiness in the optical media of the eye:
- timely treatment of viral, infectious, fungal diseases of the eyeball;
- timely treatment of systemic diseases that can lead to complications for the eyes, causing visual impairment due to the accumulation of insoluble substances;
- normalization of nutrition, which should include all useful substances, and also reduce the amount of insoluble proteins;
- treatment of endocrine diseases through hormone replacement therapy;
- taking medications prescribed by a doctor;
- In case of mechanical eye damage, consult a doctor and avoid self-medication, which may worsen the situation.
The preventive measures used will not completely eliminate the risk of developing vitreous opacities. This is due to the fact that the pathological condition may be a consequence of the physiological process that forms aging in people after 50 years of age. But the use of preventive measures will significantly reduce the possibility of complications.
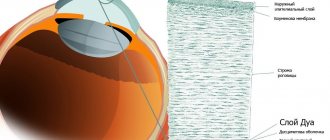
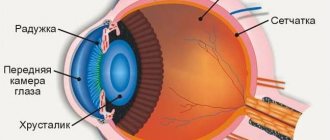
Composition and structure
99.7% of the eyeball consists of water, which allows the eyeball to maintain a constant shape. Its volume is about 4 ml, weight - 4 g.
CT contains hyaluronic acid and is produced by its cells. Its anterior surface is adjacent to the lens, forming a small fossa at the point of contact. On the sides, the vitreous body borders on the ciliary body of the eyeball, and along the entire remaining length - on the internal limiting membrane of the retina.
The ciliary body is located in the middle part of the retina and serves to suspend the lens. The body itself has its own limiting membrane. It is missing only in 2 places: in the area of the optic nerve head, and also where the gel is fixed at the dentate line. From there, special membranes run inside the eye, dividing the cavity into separate chambers.
Inside, the vitreous body is divided into tracts. Its skeleton consists of a thin network in the form of intertwined collagen fibers of different shapes (here these collagens are specific to ST and are called vitrosins).
Liquid CT floats between the fibers, which gives it a gelatinous character. At the boundaries of the ST there are cells - hyalocytes. They secrete hyaluronic acid, collagens and CT proteins. They have macrophagocytic activity.
What is the danger of vitreous destruction?
An alarming symptom, which should serve as a reason for an immediate visit to an ophthalmologist, is a rapid increase in the number of “floaters” with a simultaneous and equally rapid decrease in visual acuity, distortion of the shape and/or size of the observed objects, the addition of light effects - flashes, lightning, sparks, etc. .P. Such symptoms indicate mechanical irritation of the photoreceptors of the retina and may be a harbinger of its detachment, which already poses a threat to vision as such. Accordingly, this is the most dangerous variant of the development of DST, subject to immediate intervention and specialized intensive care.
By contacting our ophthalmological center when the first signs of destruction appear, you can be sure of high-quality diagnosis and effective treatment of the disease (if necessary) by recognized doctors, using modern equipment and at reasonable prices in Moscow!
Possible complications of vitreolysis
Usually there are no complications after vitreolysis, but sometimes unwanted side effects occur:
- Increased intraocular pressure;
- Retinal disinsertion;
- Choroidal microhemorrhages;
- Cataract.
It should be noted that most negative consequences can be predicted in advance, so it is very important to conduct a full examination before surgery. This will allow the doctor to predict all possible risks during the procedure.
Vitreolysis
Vitreous destruction can also be treated with laser. Currently, this is the most effective method of influence. As a result of laser radiation, conglomerates are broken into small pieces, and they no longer interfere with vision.
For the first time, Frank Franhoser proposed using a YAG laser to treat destruction of the vitreous body. He became the author of a number of studies on vitreolysis. The first results of his work were published back in 1985. Currently, a large number of foreign articles have been published proving the effectiveness and safety of this technique.
Contraindications
Vitreolysis is not recommended for:
- Luxation of the lens into the vitreous;
- Reduced transparency of optical media or the appearance of other obstacles to the laser beam (suspension in aqueous humor, hyphema, edema and clouding of the cornea, cataracts);
- The presence of pronounced neovascularization;
- Retinal disinsertion;
- High risk of hemorrhage, which is diagnosed based on a blood test;
- Detachment of the choroid.
Sometimes these contraindications become relative, that is, the operation is performed under certain conditions.
When performing effective treatment of vitreous destruction, the patient’s quality of life significantly increases, and the risk of possible complications and vision loss is reduced.