Symptoms
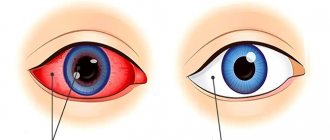
The only visual sign of hemophthalmos is the saturation of the vitreous body with blood and ophthalmological disorders in the form of loss of visual acuity. There are no direct nerve endings on this structure, which means that the occurrence of pain or a feeling of compression is simply impossible. The external manifestations of the disease depend entirely on the volume of hemorrhage. All forms of hemophthalmos occur in several stages:
- Internal bleeding. Lasts no more than a day. Blood cells penetrate the vitreous body and its nearby structures, settle on the surface and dissolve in the liquid medium;
- The appearance of a hematoma. Associated with the occurrence of blood clots on the structural elements of the visual apparatus. The process lasts no more than 2 days;
- Toxic-hemolytic stage. Lasts from 1 to 2 weeks. Blood clots begin to spontaneously break down, as a result of which their breakdown products begin to affect the visual apparatus. This is what causes clouding of the vitreous body;
- Proliferative-dystrophic period. It can last up to six months. At the site of the destroyed blood clot, connective tissue is formed, which triggers dystrophic and atrophic processes in the eyeball and retina;
- Intraocular fibrosis. The most severe stage of development of hemophthalmos. Retinal detachment occurs, the fluid inside the vitreous body changes to connective tissue, and the organ itself becomes very dense. Complete atrophy of the eyeball or irreversible blindness often occurs.
In addition to a visual examination of the eyeball, subjective ophthalmological disorders, which may not occur in all cases, also help determine the development of hemophthalmos. These include the appearance of floaters or dark spots before the eyes, blurred vision, and photophobia.
How to treat hemophthalmos?
As soon as you notice the first slight redness in the eye or disturbances in the quality of vision, you should immediately consult a doctor
This is important to do both in case of traumatic hemorrhage and in case of a suddenly burst vessel. After all, if the vessel burst from an impact, other internal organs could also be damaged
Sudden causeless hemorrhage is even more dangerous. As a rule, it indicates the fragility of blood vessels throughout the body, and not just in the eye. This may be the first sign of a serious illness or hormonal changes in the body. If, after a hemorrhage in the retina, you do not go to the doctor in time and prescribe treatment, then hemophthalmos can lead to complete blindness.
After conducting an examination and finding out the cause of the hemorrhage, the ophthalmologist will select the correct treatment. The format of therapy will depend on the stage at which the disease is detected and how large the extent of tissue and vascular damage is.
If we are talking about large-scale hemorrhage, the patient is immediately hospitalized. In the first few hours after the appearance of hemophthalmos, a cold compress is applied to the eye in the same way as to a regular bruise. But if the healing process of a bruise can be accelerated with the help of creams and ointments, then there is no way to influence the restoration of the appearance of the eye. Hemophthalmos gradually resolves without outside interventions. There are no ways to speed up this process from the outside.
Patients diagnosed with vitreous hemorrhage are prescribed the following treatment:
- a course of vitamins C and K, which strengthen the walls of blood vessels and normalize blood circulation;
- blood transfusion (in some cases) for faster resorption of blood clots;
- sodium chloride and glucose for intravenous administration;
- prescribing medications such as emoxipine.
If it is difficult to eliminate the cause of hemophthalmos using therapeutic methods, the doctor will refer the patient for surgery. Surgery is performed to remove blood clots and damaged parts of the vitreous. The excised areas are filled with hyaluronic acid, which helps accelerate the regeneration of the vitreous body and restore its functionality.
Whatever the cause of the hemorrhage, it is better to consult a doctor immediately. After all, self-medication and delaying examination can end extremely sadly. Hemophthalmos is a characteristic symptom of many serious diseases. Prompt identification of the disease will help quickly eliminate the causes of vascular fragility and avoid vision problems.
Prevention of hemophthalmos
The specifics of the disease do not imply mandatory measures to prevent hemophthalmos.
Healthy people, without signs of pathology and degenerative changes in the retina, are recommended to follow safety rules at work and avoid eye damage. When engaging in dangerous sports, you should wear a protective helmet and goggles.
The risk group includes people over 35-40 years of age who suffer from diseases that can cause hemophthalmos. Such patients should monitor blood pressure and blood sugar, and periodically monitor intraocular pressure. Patients with eye diseases should visit an ophthalmologist regularly and undergo a complete ophthalmological examination. If signs of retinal detachment are detected, laser interventions can be performed to reduce the risk of hemophthalmos.
In premature babies, prevention of hemophthalmos consists of careful handling. In case of congenital pathology, surgical intervention is performed - vitrectomy.
Prolonged intraocular hemorrhage can lead to serious complications, including complete loss of vision and disability.
Most often, destructive processes are observed in the vitreum, the formation of connective tissue and its proliferation. Hemophthalmos can cause a disease such as amblyopia in children, and lead to secondary glaucoma in adults.
How to prevent and prognosis?
Prevention of hemorrhage into the vitreous cavity does not have clear rules. Ophthalmologists recommend regularly monitoring your health. For patients suffering from diabetes, it is important to maintain normal glucose levels. These people are at risk for many diseases, in particular ophthalmological ones, so regular examinations are required - at least 2 times a year. For patients over 40 years of age, it is important to keep blood pressure levels normal and undergo an annual examination with an ophthalmologist to determine intraocular pressure. The main measures in prevention are considered to be measures to maintain the normal condition of blood vessels.
The prognosis depends on the stage of development of the pathology. Partial hemorrhage, which does not exceed 12%, in most cases resolves on its own and does not pose a great danger. Damage to a quarter of the vitreous complicates the treatment process and increases the risk of retinal detachment. The total type of hemophthalmos involves irreversible blindness. In 95% of such patients, disability awaits.
Causes
Destructions of the blood vessels of the eye are divided into several types:
- filling the anterior chamber of the eyeball with blood;
- hemorrhage behind the conjunctiva;
- vitreous hemorrhage;
- ruptures of retinal vessels.
Bleeding between the cornea and iris is called hyphema. With this pathology, blood fills the anterior chamber of the eye. Most often, such hemorrhage occurs as a result of injury or ophthalmic surgery. Less commonly, the cause of this disorder is herpes, a blood clotting disorder, or cancer. In this case, you can visually observe the blood behind the cornea, in addition, the patient experiences painful sensations in the eyeball.
Subconjunctival hemorrhage is clearly visible on the white mucous membrane of the eye. It occurs due to the destruction of blood vessels. Quite often, tiny capillaries burst from physical stress of the body. This can happen when you sneeze, have strong and prolonged coughing spells, or do heavy work. Injuries and damage to the eye also cause the formation of hemorrhages on the membrane of the eye.
Since the vitreous body itself does not have a circulatory system, blood enters it when the retinal vessels are destroyed. There may be several reasons for this pathology:
- detachment of the retina from the vitreous body;
- the patient has high blood pressure;
- eye tumor;
- retinal damage during surgery.
When blood enters the vitreous body, the patient may observe a slight haze in the field of vision, formations in the form of a cobweb and a reddish tint in the observed objects. In severe cases, severe deterioration of vision, up to complete blindness, is possible.
- hypertonic disease;
- vasodilation associated with an aneurysm;
- eyeball injuries;
- traumatic brain injury;
- strong changes in atmospheric pressure.
High blood pressure is a very common cause of burst capillaries in the eyes. Vascular aneurysms and thrombosis can also cause destruction of a blood vessel and hemorrhage into the retina. Eye injuries and craniocerebral disorders are necessarily accompanied by intraocular bleeding. Dangerous retinal hemorrhages occur in professional divers, but most often in inexperienced divers who do not follow the decompression regime when ascending from depth.
Types and differences of hemorrhages in the eye
In young people, any bleeding in the eye is associated with an accidental blow or fight. Older people will most likely think about a jump in blood pressure and will begin to strongly advise urgently going to see a therapist or at least using a blood pressure monitor.
Hyposphagma
This is the entry of blood from the vessels under the conjunctiva. In the diagnosis made by the doctor in the medical history, such blood spillage in the sclera is also referred to as “subconjunctival hemorrhage in the eye.”
People will make the diagnosis “a vessel has burst,” which will also be correct, because such an accumulation of blood is caused by ruptured capillaries, from where the blood enters that part of the white of the eye that is located around the iris.
Possible reasons
- Traumatic impact to the eye; its long and strong friction; a sharp jump in atmospheric pressure (working in tanks, hyperbaric chambers, sealed enclosed spaces, etc.), a blow to the cornea with a foreign object (a large insect at high speed), exposure to aggressive chemical reagents.
- Poor blood clotting caused by congenital or acquired hemophilia, uncontrolled and excessive use of blood thinners in the form of aspirin, dipyridamole, heparin, ticlid, etc.
- A surge in pressure during vascular spasms, childbirth with its attempts, constipation, sharp, “heartfelt” sneezing, blowing a very stuffy nose, an attempt to lift an unbearable weight, suffocation, vomiting, convulsive cough.
- Eye infections.
- Consequences of eye surgery.
- Fragility of blood vessels caused by vitamin deficiency with deficiency of vitamins K and C; diabetes, atherosclerosis, systemic connective tissue lesions (vasculitis, lupus).
Hyposphagma, when viewed as a cosmetic defect, is considered the most harmless and quickly passing disease. Compared to subcutaneous hematomas (bruises), it does not change in color, but simply turns pale, gradually dissolving.
The feeling of an obstacle in the eye in the presence of such a hemorrhage can be attributed, rather, to psychological inconvenience, as an obstacle it is perceived more at the level of self-hypnosis.
Thus, the disappearance of the blood stain inside the sclera occurs without drug intervention.
We advise you to read: How an eyesore forms in a person’s eyes and how to treat it.
Although the resorption of the red spot can be accelerated with potassium iodine eye drops. And if you detect the beginning of the formation of a bruise in the sclera, and it continues to expand, then stop this process by instilling the popular drip products “Vizin”, “Naphthyzin for the eyes”, “Octilia”, etc.
Hyphema
The location of the hemorrhage is the compartment between the iris (which gives our eyes their unique color) and the convex outer lens of the clear cornea. This place is called the anterior chamber of the eye.
In the normal state, the chamber is filled with a transparent substrate of complex composition. Hyphema is the leakage of blood into this chamber.
The accumulation of such blood looks like a segment in the lower part of the iris, and the larger the hemorrhage, the larger the area this segment occupies.
The anterior chamber, as a result of extensive hemorrhage, may even be completely filled, giving the iris, whatever color it was previously, a pure bloody color.
Why do eyes turn red, and how to prevent diseases of the organs of vision?
The cause of the pathology is always a rupture of the vessel. What are the most common causes of breakups?
Injuries
Types of injuries:
- Penetrating - with eye damage starting from the cornea and further inward, forming a through channel between the internal cavity of the eyeball and the external environment. The most common injuries are caused by piercing sharp objects. Less often - from blunt blows, but then the blow must be strong.
- Non-penetrating. With such an impact, the eye may remain intact, but the impact results in consequences reminiscent of a contusion, up to and including dynamic destruction of the internal structures of the eye. This type of injury is almost always caused by blunt force trauma. May be accompanied by a concussion.
- Trauma also includes all surgical manipulations of the eyes.
Eyeball diseases
Diseases of the eyeballs associated with the appearance and growth of defective blood vessels in the eye (neovascularization). New vessels always have some structural defects, which makes their walls more fragile than normal ones. When these walls rupture with minimal impact, hemorrhage occurs into the cavity between the cornea and the iris.
Neovascularization occurs from:
- Diabetic angiopathy in diabetes
- Defects of the venous network in the retina and the beginning of its detachment
- Tumors in the eye and inflammation of intraocular structures.
Diagnostics
The obviousness of the signs of the disease does not raise doubts about the diagnosis, and the doctor can only prescribe treatment, based on the very fact of hematofilling of the anterior chamber and the amount of blood in it. The diagnosis is made based on simple steps:
- Examination of an eye with hyphema
- Measuring pressure inside the eyes with a special tonometer
- Determination of visual acuity percentage
- Examination of the eye using a hardware method (using an ophthalmological microscope).
Before treating hyphema, it is necessary to accurately determine the causes of its appearance and eliminate the external factors that caused such a pathology, such as:
- Cancellation of blood-thinning drugs (if they were prescribed)
- Vitamin deficiency, if present
- Ophthalmic infections
- Bad habits, especially heavy smoking
However, if the hyphema occupies up to 1/3 of the iris segment, its resorption is only a matter of time. To speed up this process, use 3% drops of potassium iodide and medications designed to reduce intraocular pressure (Azopt, Timolol, Latanoprost).
If the course of the hyphema is complicated, surgical intervention is indicated.
Hemophthalmos
The vitreous body is normally a gel of ideal transparency, in which the light flux passing through the aperture of the pupil and focused by the lens must freely reach the retina in the posterior hemisphere of the eye. Any foreign inclusions, including blood, interfere with the passage of light, causing sensations of an obstacle of varying degrees of density and opacity in front of the eyes.
Cases of hemorrhage into the vitreous body, or hemophthalmos, are most often associated with painful inflammation of the retina. Or rather, with ruptures of the microvessels covering this inner hemisphere under the photosensitive elements.
Causes
Vascular ruptures are possible from:
- Concussion impact (a strong blow to the head with symptoms of a concussion) against the background of intracranial pressure caused by such impact, which goes far beyond normal limits.
- Rupture of the membranes of the eye from a penetrating wound
- Blood clots in the retinal vessels
- Retinal vascular abnormalities
- Hematopathologies associated with low coagulation
- hypertensive crises
- Diabetes
- Oncological problems of the eye.
- An abrupt increase in pressure in the sternum from coughing, labor, with strong vomiting spasms, extreme strength loads, sneezing).
The use of potassium iodide leads to rapid results in the treatment of bacterial and fungal infections and resulting mechanical damage to the eye, eliminating hemophthalmos.
There are no nerve receptors in the glassy gel, so a person with hemophthalmos does not experience pain. Hemophthalmos can manifest itself only in the form of decreased vision, sometimes to complete blindness.
Kinds
These hemorrhages are:
- Total, when the internal volume of the eye is filled with blood by more than ¾. They almost always occur as a result of traumatic effects on the eye. Characterized by blindness with the presence of light perception, but without distinguishing the details of the surrounding world.
- Subtotal, with a volume of blood filling from 1/3 to ¾. The most common cause is diabetic vascular damage. Vision in this case is the discrimination of silhouettes and general contours of objects.
- Partial, with a lesion volume of less than 1/3. It is observed in cases of the onset of retinal detachment, with arterial hypertension or progressive diabetes. Manifestations – black dots, a red streak or a red veil in the eyes.
Prevention
Preventive actions for hemophthalmia depend on the patient’s pathological diseases.
Some conditions, such as posterior vitreous detachment, cannot be prevented. The administration of antiplatelet agents (acetylsalicylic acid, tiplopidine) reduces the risk of recurrence of retinal vein thrombi, both in the diseased and healthy eye.
Patients suffering from diabetes need constant monitoring of blood sugar levels to prevent microvascular damage. In case of primary visual manifestations of the disease, an urgent visit to a specialist is required.
An original drug to solve problems with vascular tone
To prevent the occurrence of such dangerous conditions, you should be careful about your health. Regularly undergo preventive examinations with doctors, monitor your diet and level of physical fitness.
Symptoms and classification
There are no nerve fibers in the internal environments of the organs of vision; when they are damaged, there are no standard clinical manifestations: discomfort, pain, itching. The only sign of the disease is a sharp drop in the level of vision, up to absolute blindness.
Clinical features of the disease make it possible to divide hemophthalmos:
- Total type - when filled with biological fluid more than three quarters. Similar problems arise after trauma to the visual organs. Symptoms are manifested by an almost complete absence of vision, with preservation of sensitivity to light. The patient cannot distinguish objects located in the field of view or freely navigate in space;
- In subtotal - the internal cavity is filled with blood from one third to three quarters. It is provoked by diabetic damage to the blood vessels of the fiber. The patient sees with the affected eye vague outlines of things and silhouettes of people;
- Partial – when less than a third of the vitreous glass is filled with blood. It is one of the frequently recorded types of hemorrhage; it occurs under the influence of diabetes mellitus, retinal detachment, and hypertension. Characterized by flashing black dots, reddish stripes in front of the eyes or nebula.
This form affects both organs as an exception; mainly one eyeball is affected. The main goal of therapy is observation without specific treatment; partial forms disappear spontaneously.
If primary symptomatic manifestations of hemorrhage in the scleral area appear, the patient should immediately seek medical help. Timely identification of the source of the deviation will allow you to prescribe an adequate course of therapy and prevent the formation of complications.
Vitreous hemorrhage
The vitreous body is a transparent substance with a gel-like structure. Placed behind the lens. Its main function is to support the shape of the eye and transmit light to the retina from the pupil. Bleeding in this structure is a relatively rare phenomenon, because this structure does not have blood vessels, so bleeding occurs when the blood vessels located in the retinal area burst.
The following reasons can provoke the appearance of hemorrhage in this case:
- Eye injury.
- Hemorrhage.
- Vitreous detachment.
- The appearance of pathological vessels in the retinal area (if a person has diabetic retinopathy).
- Damage to retinal vessels due to hypertension, atherosclerosis and other diseases.
- Neoplasms in the eyeball area (if this area swells and adjacent tissues are damaged).
- Carrying out various ophthalmological procedures and operations (including laser).
Preretinal hemorrhage in the retina and vitreous body leads to blurred vision, dots, “spots”, etc. are formed. When you look, the world around you becomes reddish, objects seem a little reddened. The disease usually affects one eye (left, right), is unilateral and rarely spreads to the adjacent eye.
The disease is diagnosed by an ophthalmologist, who examines the eye using a slit lamp and prescribes an ultrasound examination. The patient must undergo a general blood test (to exclude the infectious nature of the disease). In difficult cases, people are sent for a computed tomography scan.
Therapeutic tactics for this disease will depend entirely on the reasons that caused the hemorrhage:
- At the first stage, the main source of the bruise is accurately determined.
- After which the bleeding stops.
- Next, procedures are carried out aimed at restoring the structure of the retina so that the person does not lose his vision.
- At the last stage, everything necessary is done to restore normal visual acuity.
If the blood accumulated in the vitreous body covers other structures of the eye, continues to flood and interferes with therapy, then surgical intervention is indicated to remove the vitreous body, which will stop the bleeding (the structure is completely removed). After the operation, a special silicone substance is injected into the area of the eyeball to keep the retina in its usual place. Operations of this type are performed in special ophthalmology clinics. Despite their complexity, they are relatively safe and cannot harm human health (regardless of his age).
Useful video
Useful information can be found at the following links:
Hemorrhages in the tissue of the eye are dangerous lesions of the organ of vision. Timely contact with an ophthalmologist helps maintain the ability to clearly see the world around you.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
Treatment
Most often, subconjunctival hemorrhage goes away on its own and does not require special treatment.
At the same time, you want to remove the cosmetic defect as quickly as possible, and therefore gentle therapy is carried out using folk remedies.
In case of III degree of damage, the need for specific treatment is determined by the doctor. If the identified causes are associated with internal pathologies, then it is necessary to treat the underlying disease.
Drug therapy
For your information! If there is growth of the affected area and the risk of complications, drug therapy is carried out with the following drugs:
- Angioprotectors – Doxium, ascorbic acid, Rutin, Troxevasin, Etamzilat, Divascan, Parmidine. They are used to strengthen vascular walls, improve the rheological properties of blood, and provide antispasmodic effects.
- Preparations for resorption of bruises - Chymotrypsin, Fibrinolysin.
- Anticoagulants - iodine preparations, Heparin. Prescribed to normalize blood composition and reduce lipid and cholesterol levels.
- Moisturizers. Preparations based on hydroxypropyl cellulose are taken. They can improve the condition of the tear film, as well as speed up the resorption of the hematoma.
- Antibacterial drugs. They are prescribed for infectious lesions and the appearance of pronounced inflammatory reactions. The type of remedy is determined by the doctor based on the type of infection.
- Vitamins. Vitamin therapy is aimed at strengthening the vascular system. The most popular vitamins are C and P.
Drug therapy is carried out only as prescribed by a doctor and after conducting the necessary diagnostic tests.
Note! Preparations for local action (eye drops) and systemic effects (tablets, capsules, injections) can be used.
ethnoscience
To speed up the resorption of a hematoma in the eye, traditional methods are most often used. Arnica-based products are popular:
- Mountain arnica tincture. The flowers of the plant are crushed and infused in alcohol for at least 3 days. The proportion is 1:10. The tincture is taken orally before meals in the form of a mixture - water or milk (200 ml) and tincture (35 drops). Take 3 times a day.
- Arnica infusion. Crushed flowers (3 tablespoons) are poured with boiling water (250 ml) and left to cool. Take 1 tablespoon 3 times a day. When used, it can be diluted with water or milk.
Another effective medicinal plant is sophora. For hemorrhage, you can use an alcohol tincture of this plant.
For reference! Fruits are used, which are crushed, filled with alcohol or vodka (equal ratio) and infused for 15-20 days.
Taken orally 3 times a day, 1 teaspoon (diluted)
Another remedy is chicory decoction. The roots of the plant (3 tablespoons) are boiled in water (500 ml) and infused for 20 minutes. A decoction of 100 ml is taken 2-3 times a day.
Compresses on the eye are good for resolving bruises.
Particularly highlighted for them are remedies such as aloe or cabbage juice. You can apply a compress of willow leaves.
How to treat and what drops are best to use
The first desire that arises when identifying a bloody spot on the eye is how to remove it quickly. This is especially true for women, for whom the issue of aesthetics plays a fundamental role.
Treatment is selected taking into account the degree of damage.
In mild cases, drug therapy is not prescribed. A cosmetic defect can be eliminated using folk remedies.
If the third degree of pathology is detected, the help of a doctor is required. Only a specialist can figure out the cause of the hemorrhage. If it lies in the dysfunction of internal organs, treatment is aimed at eliminating the underlying disease.
If the bloody spot grows or relapses occur, the ophthalmologist recommends drug therapy.
Drops for rapid resorption of bruises:
- Emoxipin;
- Emoxy-Optic;
- Vixipin.
Agents from the group of angioprotectors for correcting blood microcirculation and reducing the permeability of vascular walls:
- Troxevasin;
- Rutin;
- Doxium;
- Etamzilat.
To stabilize cholesterol and lipid levels and normalize blood composition, the following drugs are recommended:
- Heparin;
- medications containing iodine.
They are also used to dissolve blood stains.
The need for antibacterial agents arises when there is an infectious lesion or signs of an inflammatory process are detected. Medicines are prescribed by the attending physician, taking into account the type of infection.
- It would not be superfluous to supplement therapy with vitamins, which also help strengthen the vascular wall. The vitamin complex should include: ascorbic acid and flavonoids (vitamin P).
- The consequences of serious injuries and pathologies sometimes require drastic solutions. To remove a bruise from the anterior chamber or vitreous, surgical intervention is performed and laser coagulation of the retina is prescribed.
- Any drugs are prescribed only after diagnostic measures have been carried out. You should not try to remove a cosmetic defect yourself, as this can lead to deterioration in visual function.
Treatment
The prognosis during treatment by any of the possible methods is always ambiguous. Currently, no technique has been developed that is guaranteed to relieve the patient of the problem. Existing methods are very often combined with each other and replaced in the absence of the desired effect. The most important thing is to contact medical professionals at the first manifestation of symptoms and not self-medicate. It is also possible to be observed by specialists in several areas at once, depending on the causes of the disease.
Before prescribing treatment for a disorder of the structure of the vitreous body of the eye, the ophthalmologist must conduct a thorough diagnosis, which includes:
- Fundus examination;
- Analysis of vision quality;
- Inspection and analysis of the disorder using a slit lamp;
- Anamnesis.
Next, the examination results are compared with the patient’s complaints and the ophthalmologist prescribes treatment.
In some cases, treatment for disturbances in the structure of the vitreous body is not required and the problem disappears on its own. The decision to prescribe treatment or not can only be made by a qualified doctor. The scheme and methods for removing pathology are also established on an individual basis. It is also worth noting that the effectiveness of treatment largely depends on the correct identification of the causes and the possibility of eliminating them, which is what actions are aimed at in the first place.
By medication
- Absorbable: Wobenzym, Traumeel-S, potassium iodide solution;
- Normalizing blood circulation: Cavinton, Cinnarizine;
- Normalizing microcirculation: Emoxipin.
Surgically
Surgical treatment of the disease cannot always lead to relief from the problem and in some cases causes complications in the form of retinal detachment, inflammation, cataracts, and hemorrhages. Surgeries are especially difficult for older people; the risk of complications in their case can increase significantly.
Currently, two forms of surgical intervention are used:
- Vitreolysis – splitting of opacities in the eyeball using a laser device;
- Vitrectomy – replacement of the vitreous body with artificial analogues (full or partial).
Folk remedies
If the disease is mild, you can use folk remedies:
- Eye drops made from honey and water (two parts honey, one part water);
- Drops of honey and aloe juice;
- Propolis solution;
- Massage the eyeballs with your fingertips.
Also, these funds can be combined with basic medications prescribed by the doctor.
Symptoms and varieties
Bleeding in the eye can be accompanied by a variety of symptoms and signs. This largely depends on the location of the damaged blood vessel. In this regard, several types of pathology are distinguished:
- hyphema;
- complete and partial hemophthalmos of the eye;
- retinal hemorrhages;
- hyposphagma.
Each of these types occurs due to different reasons, and therefore require a specialized approach to therapy.
Hyphema
The term hyphema means intraocular hemorrhage localized in the anterior chamber of the eye (it is located between the cornea and the iris). Signs can be detected with the naked eye - a purplish-red liquid forms a horizontal level on the anterior chamber.
The cause of such hemorrhage in the eyeball may be an inflammatory process affecting the ciliary body or iris. If blood leaking from the eye saturates the cornea, this can lead to a sharp deterioration in vision.
Hemophthalmos
Hemorrhage into the vitreous body of the eye is called hemophthalmos of the eye. This pathology often occurs for the following reasons:
- acute circulatory disorders;
- ruptures and detachments of the retina;
- damage to the central retinal artery (with atherosclerosis, thrombosis, embolism);
- diabetic retinopathy.
Important information: What to do and how to stop bleeding with an ovarian cyst (polycystic disease)
As in the case of retinal hemorrhage, symptoms of hemophthalmos bother patients. The list of typical complaints:
- decreased visual acuity;
- appearance of blood from the eye;
- red veil;
- the appearance of cobwebs, dark spots and floating threads in the field of vision.
During the diagnosis, the absence of the fundus reflex is revealed. In this case, a distinction is made between complete and partial hemophthalmos.
Retinal
Retinal hemorrhages in the eye are those that are concentrated in the retina. They develop against the background:
- hypertension;
- diabetes mellitus;
- atherosclerosis.
The main symptoms of this pathology:
- deterioration or complete loss of vision;
- colored or black spots before the eyes;
- the appearance of a veil.
According to external signs, retinal hemorrhages are divided into several types:
- Intraretinal. In such cases, bleeding occurs into the thickness of the retina. Externally, the clinical picture appears in the form of small circles or purple streaks.
- Preretinal. Blood accumulates between the hyaloid membrane in the vitreous body of the eye and the retina. They look like a large puddle, larger than the optic disc in size.
- Subretinal. In such cases, blood flowing out of the eye accumulates between the layer of nerve fibers and the retinal epithelium. They appear as ill-defined dark spots.
Hyposphagma
Hypophagma is a subconjunctival hemorrhage in which blood comes from the eyes and accumulates between the conjunctiva and sclera. This type of pathology is considered the most common. In 98% of patients with contusion, hemorrhage in the sclera is detected.
The list of reasons for the appearance of this pathology should include:
- injuries and concussions;
- excessive physical activity;
- high blood pressure;
- severe cough, vomiting, straining.
Visible manifestations are the appearance of red, irregularly shaped areas on the white of the eye. The size of the hemorrhage in the eye depends on the degree of damage.
With severity 1-2, the patient does not experience pain or discomfort. The quality of vision is not reduced. With the third degree of severity, a foreign body sensation often appears. During blinking, this feeling intensifies. This symptom does not affect visual acuity. This clinical picture rarely lasts longer than three weeks. If the pathology occurs due to impaired hemostasis, then frequent relapses are possible.
Hyphema
Hyphema is a pathological process in which blood begins to accumulate in relatively large quantities in the anterior chamber of the eyeball. This zone is located between the iris and the cornea. As the blood accumulates, it begins to gradually cover the whites and other external structures of the eye, resulting in a gradual deterioration of vision (if the process is neglected, cataracts develop and vision loss occurs).
Most often, the development of hyphema is caused by injury (a blow, a fall, after various ophthalmic surgical interventions (for example, during eye surgery as a consequence)).
Also, the main reasons for the appearance of hyphema include:
- Violation of blood clotting processes.
- Infection of the eyeball with herpes.
- The appearance of damaged blood vessels in the iris.
- Cancer process.
In addition to the occurrence of a small hematoma on the eye, hyphema is also accompanied by the following symptoms: a relatively large amount of blood accumulates in the anterior chamber; Photosensitivity increases significantly; pain appears in the area of the eyeball and forehead; vision gradually becomes blurred, the picture is blurred and blocked.
An ophthalmologist diagnoses this type of disease. To make a diagnosis, an external examination and examination of a person’s complaints are usually sufficient. Already at the initial appointment, the specialist will examine the internal structure, measure the pressure in the eyes, and determine visual acuity. In difficult situations, various additional examinations are prescribed.
Taking into account the probable causes of the disease and based on the results of the examinations performed, the ophthalmologist can give the following therapeutic recommendations:
- Reduced physical activity (in some cases, complete bed rest is recommended).
- Wearing a bandage over an eye that is swollen with blood.
- High position of the head during sleep so that excess blood does not flow to the eyes.
In such situations, traditional treatment with eye drops or surgery is indicated (surgery is always prescribed if there is a possibility that a person may lose vision).
What do constricted pupils mean?
Constricted pupils are a very common phenomenon. The pupils of a healthy person constantly change their size, becoming either wider or narrower, due to a natural reaction to changes in the brightness of light. As brightness increases, the pupils reflexively constrict. This phenomenon in ophthalmology is called miosis. But as soon as you dim the brightness of the light a little, the pupils begin to dilate. This phenomenon is called mydriasis.
If the pupils remain constricted for a long time and do not respond to changes in light intensity, then this may indicate the presence of serious pathologies and requires immediate contact with a specialist.
What is a pupil and how does it work?
The pupil is a small hole of variable diameter in the iris of the eye. This hole is the diaphragm of the eyeball and can change its size depending on the internal state of the human body or changes in light intensity. In an unirritated state, its diameter varies from 2 to 8 mm.
The change in the size of the palpebral fissure occurs due to the alternate work of 2 eye muscles: the sphincter, which is responsible for narrowing, and the dilator, which is responsible for widening. The entire process is controlled by the nervous system and the cerebral cortex.
The process of the pupil's response to light occurs in 4 stages:
- The photoreceptors of the retina receive light stimulation.
- The optic nerve sends the signal to the cerebral cortex.
- The cerebral cortex produces an impulse responsible for miosis.
- The impulse is transmitted through nerve endings to the sphincter, which provides contraction.
All these invisible internal processes take a fraction of a second, so outwardly you can observe the effect of the instantaneous reaction of the eye opening to light.
Miosis is a very powerful and indicative reflex. It closes on the cerebral cortex and operates as long as the cortex remains alive. In other words, even if a person is in a state of coma or clinical death, miosis persists.
And in some cases, only by this reflex can one judge whether a person is alive or not. That is why checking the pupil for miosis is the most important emergency medical procedure if the patient is unconscious.
Causes of pupil constriction in healthy people
There is a whole list of reasons when constricted pupils should not be classified as a pathology. Reduced palpebral fissures in older people and newborns are considered quite normal. In older people, this is a natural reaction of the body to an age-related reduction in physical and mental activity.
In babies under one year of age, the pupils differ significantly from the pupils of an adult, both in structure and functioning. Firstly, they are narrowed physiologically and have a diameter of about 2 mm. Secondly, they react poorly to light and expand very poorly. But as the child grows up, everything returns to normal.
In middle-aged people, the eye openings may narrow as a result of mental and physical overload. However, after rest, their size is restored.
The size of the pupils may decrease as a result of taking certain medications, such as heart medications or sleeping pills.
What diseases can constricted pupils indicate?
Eyes are not only a mirror of the soul, but also a reflection of a person’s state of health. The number of diseases accompanied by miosis is enormous.
These can be either minor deviations in the functioning of the human body, for example, discomfort in the nasopharynx or severe pain as a result of a bruise, or serious dysfunction of the brain and nervous system.
Miosis is a constant companion of nicotine, alcohol and, especially drug addictions. Narrow pupils are one sign of drug intoxication that every parent should know these days. Even if a teenager's behavior is relatively normal, small pupils will definitely give him away.
There is also the concept of toxic miosis, which develops as a result of poisoning caused by a number of products, medications, and chemicals. In peacetime, the effect of miosis occurs when poisoned:
- mushrooms;
- caffeine;
- ethyl alcohol;
- morphine;
- bromine;
- phosphorus compounds, for example, dichlorvos;
- dyes.
During combat operations, narrowed palpebral fissures are observed in those who have been exposed to chemical warfare gases.
Miosis may indicate the presence of eye diseases. The simplest of them is the entry of a foreign body into the cornea. More serious diseases are iritis and iridocyclitis. In this case, the muscles of the iris experience a spasm, as a result of which the pupil stops responding to the light source.
If we talk about eye diseases, the pupil also narrows when:
- internal ocular hemorrhage;
- drooping eyelid;
- corneal ulcer;
- inflammation of the eye vessels.
What other diseases can constricted pupils indicate?
As mentioned above, the effect of miosis is provided by the nervous system and cerebral cortex. For this reason, reduced palpebral fissures often indicate serious disorders of a person’s nervous system or the functioning of his brain.
Most brain injuries cause miosis, especially if the posterior parts of the organ are injured or there is damage to the brain nerves. If, as a result of a head injury, only 1 pupil has decreased, then this indicates which side was injured.
In addition, a decrease in the palpebral fissures may indicate the presence of:
- stroke;
- meningitis;
- epilepsy;
- encephalitis;
- high pressure;
- decreased thyroid function;
- multiple sclerosis;
- brain tumors.
To summarize, we can safely say that if a person has narrowed palpebral fissures for some time, this does not always mean that serious pathologies are present.
If the reason for the narrowing lies in ordinary overexertion, then simply resting is enough. However, serious diseases can also constrict the pupils, which at first do not reveal themselves as anything other than miosis. In this case, only a doctor will be able to determine the true reasons why the pupils are constricted.
A working method to restore vision! You will throw your glasses in the trash in just 3 days...
Restoring vision. Real life story.
Treatment
When the first symptoms appear, you should immediately visit an ophthalmologist for a thorough diagnosis, which includes:
- Initial examination;
- Determination of visual acuity;
- Fundus examination;
- Angiography;
- Tomography (including using a computer);
- Gonioscopy and biomicroscopy.
After determining the nature and severity of the problem, the ophthalmologist prescribes treatment.
By medication
Mild vitreous hemorrhage resolves with drug treatment. The patient is prescribed drugs that have a positive effect on the state of the blood (Vikasol), as well as intravenous administration of sodium chloride and local administration of calcium chloride. In addition, dexamethasone solution is prescribed as a corticosteroid drug.
Vikasol is used to improve blood condition
Surgically
One of the most commonly prescribed treatments for bleeding is laser coagulation. This procedure can eliminate the problem of hemorrhage from abnormal vessels, as well as prevent relapses and possible complications of the disease.
The most radical surgical treatment for the disease is vitrectomy, which is the removal of the affected area of the vitreous. This method is shown:
- For retinopathy;
- If the condition worsens two to three months after the onset of the disease;
- In case of traumatic injury;
- With retinal detachment;
- If there are no positive results from treatment with other methods.
Folk remedies
Traditional methods of treating diseases of this type are not usually used as alternatives to professional ones. They are effective as a complement to the main methods.
- Chicory root. For thirty grams of product you need to take a glass of boiling water and leave it for ten minutes. Take half a glass three times a day.
- Aloe juice. Take a teaspoon orally after meals.
- Blueberry juice. Mix one part of the product with two parts of water and use for instillation.
VISUAL DISORDERS AND BLINDNESS (H53-H54)
H53 Visual impairment
H53.0 Amblyopia due to anopsia Amblyopia caused by:• anisometropia• visual deprivation• strabismusH53.1 Subjective visual disorders Asthenopia. Day blindness. Hemeralopia. Metamorphopsia. Photophobia. Atrial scotoma. Sudden loss of vision Visual iris rings Excludes: visual hallucinations (R44.1)H53.2 Diplopia. Image duplicationH53.3 Other disturbances of binocular vision. Retinal image inconsistency Image fusion due to stereoscopic defect. Simultaneous visual perception without image fusion Depression of binocular vision H53.4 Visual field defects. Extended blind spot. Generalized narrowing of the visual field Hemionopsia (opposite) (same name). Quadrant anopsia Scotoma:• arcuate• Bjerrum• central• ring-shapedH53.5 Color vision anomalies. Achromatopsia. Acquired color vision deficiency. Color blindness Deuteranomaly. Deuteranopia. Protanomaly. Protanopia. Tritanomaly. Tritanopia Excludes: day blindness (H53.1)H53.6 Night blindness
Excluded: due to vitamin A deficiency (E50.5)
H53.8 Other visual disturbances
H53.9 Visual impairment, unspecified
H54 Blindness and decreased vision
Note• For categories of visual impairment, see the following table. Excludes: transient blindness (G45.3)H54.0 Blindness in both eyes. Visual impairment category 3, 4, 5 in both eyesH54.1 Blindness in one eye, reduced vision in the other eye Visual impairment category 3, 4, 5 in one eye and category 1 or 2 in the other eyeH54.2 Reduced vision in both eyes. Category 1 or 2 visual impairment in both eyesH54.3 Unspecified loss of vision in both eyes. Category 9 visual impairment in both eyesH54.4 Blindness in one eye. Visual impairment categories 3, 4, 5 in one eye H54.5 Reduced vision in one eye. Category 1 or 2 visual impairment in one eye H54.6 Unspecified loss of vision in one eye. Visual impairment category 9 in one eye H54.7 Unspecified vision loss. Visual impairment category 9 NOS Note • The following table shows the classification of the degree of visual impairment recommended by the WHO Scientific Group on the Prevention of Blindness, Geneva, 6-10 November 1972 (WHO Technical Report Series, N518, 1974). The term “low vision” in H54 covers categories 1 and 2 of the table, the term “blindness” covers categories 3, 4 and 5, and the term “unspecified vision loss” covers category 9. If the limits of the visual field are also taken into account, patients with a visual field of no more than 10 degrees, but more than 5 degrees around the central visual axis, should be classified as category 3, and patients with a visual field of no more than 5 degrees around the central axis should be classified as category 4, even if central visual acuity is not broken.
Category Visual acuity with the best possible correction of visual impairment maximum value minimum value less than equal to or more than 1 6/18 6/60 3/10 (0.3) 1/10 (0.1) 20/70 20/200
2 6/60 3/60 1/10 (0,1) 1/20 (0,5) 20/200 20/400
3 3/60 1/60 (counting fingers at a distance of 1 m) 1/20 (0.05) 1/50 (0.02) 20/400 5/300 (20/1200)
4 1/60 (counting fingers at a distance of 1 m) Light perception 1/50 (0.02) 5/300 5 No light perception 9 Unspecified or unspecified
DISEASES OF THE EYELIDS, LACRIMAL DUCT AND ORBITS (H00-H06)
H01 Other inflammations of the eyelids
H01.0 Blepharitis Excludes: blepharoconjunctivitis (H10.5)H01.1 Non-infectious dermatoses of the eyelid Dermatitis:• allergic }• contact }• eczematous } of the eyelid Disciform erythematous lupus } Xeroderma }H01.8 Other inflammations of the eyelid, specifiedH01.9 Inflammation of the eyelid, unspecified
H02 Other eyelid diseases
Excluded: congenital malformations of the eyelid (Q10.0-Q10.3)H02.0 Entropion and trichiasis of the eyelidH02.1 Ectropion of the eyelidH02.2 LagophthalmosH02.3 BlepharochalasisH02.4 Ptosis of the eyelidH02.5 Other diseases affecting the function of the eyelid Ankyloblepharon. Blepharophimosis. Wrinkling of the eyelid Excludes: blepharospasm (G24.5) tic (psychogenic) (F95. -)• organic (G25.6) H02.6 Xanthelasma of the eyelid H02.7 Other degenerative diseases of the eyelid and periocular region Chloasma } Madarosis } eyelid Vitiligo } H02.8 Other specified diseases of the century. Hypertrichosis of the century. Unremoved foreign body in the eyelidH02.9 Disease of the eyelid, unspecified
H03* Lesions of the eyelid in diseases classified elsewhere
H03.0* Parasitic diseases of the eyelid in diseases classified elsewhere Dermatitis of the eyelid caused by Demodex species (B88.0+) Lesions of the eyelid in: Leishmaniasis (B55. -+) Loiasis (B74.3+) Onchocerciasis ( B73+)• lice (B85.3)H03.1* Lesions of the eyelid in other infectious diseases classified in other headings Lesions of the eyelid in:• herpes virus infection (B00.5+)• leprosy (A30. -+)• molluscum contagiosum (B08 .1+)• tuberculosis (A18.4+)• yaws (A66. -+)• herpes zoster (B02.3+)H03.8* Lesions of the eyelid in other diseases classified in other headings. Lesions of the eyelid in impetigo (L01 .0+)
H04 Diseases of the lacrimal apparatus
Excluded: congenital malformations of the lacrimal apparatus (Q10.4-Q10.6)H04.0 Dacryoadenitis. Chronic hypertrophy of the lacrimal glandH04.1 Other diseases of the lacrimal gland. Dacryops. Dry eye syndrome Lacrimal gland:• cyst• atrophyH04.2 EpiphoraH04.3 Acute and unspecified inflammation of the lacrimal ducts. Dacryocystitis (phlegmatous) } Dacryopericystitis } acute, subacute or Lacrimal canaliculitis } unspecified Excludes: dacryocystitis of the newborn (P39.1)H04.4 Chronic inflammation of the lacrimal ducts Dacryocystitis } Lacrimal gland: }• canaliculitis } chronic• mucocele }H04.5 Stenosis and insufficiency of the lacrimal ducts. Dacryolite. Eversion of the lacrimal punctum Stenosis of the lacrimal:• canaliculus• duct• sacH04.6 Other changes in the lacrimal ducts. Lacrimal fistulaH04.8 Other diseases of the lacrimal apparatusH04.9 Disease of the lacrimal apparatus, unspecified
H05 Diseases of the orbit
Excluded: congenital malformations of the orbit (Q10.7)H05.0 Acute inflammation of the orbit Abscess } Cellulitis } Osteomyelitis } orbit Periostitis } Tenonitis H05.1 Chronic inflammatory diseases of the orbit. Granuloma of the orbit H05.2 Exophthalmic conditions Displacement of the eyeball (external) NOS Hemorrhage } Edema } of the orbit H05.3 Deformation of the orbit Atrophy } Exostosis } of the orbit H05.4 Enophthalmos H05.5 Unremoved long-standing foreign body due to penetrating injury to the orbit Retrobulbar foreign body H05.8 Other diseases eye sockets. Orbital cystH05.9 Disease of the orbit, unspecified
H06* Lesions of the lacrimal apparatus and orbit in diseases classified elsewhere
Possible complications
Cloudiness, spots and other effects quickly become stable and may last forever. A mild form of the disorder does not pose a great danger and does not lead to serious complications.
The clearer and thicker the optical effects are visible, the stronger the destruction. It can develop up to complete detachment of the vitreous body. A sign of more serious problems may be the occurrence of “lightning” and “flashes”.
Whatever the form and severity of the disorder, when these symptoms appear, an immediate examination by an ophthalmologist is required. Delay can lead to even more serious consequences, including complete loss of vision without the possibility of recovery.
Treatment
The treatment strategy largely depends on the volume of hemophthalmos. If less than a third of the vitreous is affected, it is not recommended to take any serious measures, since the hemorrhage may resolve on its own within a few weeks. During this period, bed rest and regular examinations of the dynamics of the disease are prescribed. In addition, anticoagulants are prescribed to prevent the formation of clots on the surface of the organ and drugs to stabilize blood pressure, since hypertension often leads to relapse and causes complications
It is important to take vitamins B and C, which help strengthen the walls of blood vessels.
Surgical methods
For subtotal and total bleeding, conservative therapy is practically useless, since medications cannot stop the spread of blood cells and prevent the formation of clots with a large volume of bleeding. Therefore, in such a situation, they almost always resort to surgical treatment methods.
- Laser coagulation. It is used if the disease has not yet led to retinal detachment. The method consists in crushing blood cells into extremely small particles, which subsequently cease to be a threat to the health of the vitreous body. This operation is very complex in terms of execution, so it requires a certain skill of the surgeon and assistants. As a rule, with its help you can not only reduce the risk of developing complications, but also prevent relapses in the next five years;
- Antivasoproliferative therapy. This is a hybrid operation at the intersection of surgery and conservative treatment. The procedure involves injecting drugs (bevacizumab or ranibizumab) into the vitreous, which reduces the risk of complications and prevents subsequent bleeding. Often the technique is used as a preparatory procedure before vitrectomy or after some ophthalmic operations;
- Vitrectomy. It is considered a traditional way of treating complex forms of hemophthalmos. It is an endoscopic procedure, with the help of which the contents of the vitreous body are surgically removed, which is subsequently filled with an artificial liquid, gas mixture or silicone oil of similar chemical and physical properties. The technique and methodology of the procedure differs greatly depending on the skills of the surgeon and the clinical picture of the disease. As a rule, the prognosis for recovery is almost always positive if all instructions are followed during the postoperative period.
If even minor ophthalmological manifestations are detected, it is necessary to urgently seek advice from a specialist.