Hemophthalmos is a condition in which blood enters the vitreous body of the eye. The vitreum or vitreous humor is 99% water. The remaining percentage includes collagen, hyaluronic acid, ions and proteins. More than 80% of the eyeball, namely 4 ml, is vitreum. Thanks to it, the eye retains its shape and light reaches the retina.
What is hemophthalmos
There are hyaloid membranes in front and behind the vitreous body. The vitreum is limited posteriorly and laterally by the retinal membrane, and anteriorly and laterally by the epithelium of the ciliary body. Anteriorly, the structure is in contact with the ligaments of Zinn and the lens capsule. Due to such close anatomical and functional interaction, the health of the retina largely depends on the condition of the vitreous body. Vitreum is firmly attached to the retina along the dentate line and around the optic nerve, where the fixation can weaken as the body ages, causing posterior vitreous detachment.
Types of hemophthalmos:
- Partial. Hemophthalmos occupies a third of the volume of the vitreous body. Occurs after mild eye injuries, against the background of diabetic retinopathy, atherosclerosis, arterial hypertension, retinal dystrophy and vascular pathologies.
- Subtotal (from 1/3 to ¾) and total (more than 3/4 of the volume). They develop as a result of severe injury to the eyeball (penetrating or non-penetrating).
Hemophthalmos causes structural changes in the vitreous body, which can be dangerous for vision. Along with the blood, red blood cells enter the vitreum. Gradually they begin to break down, releasing hemoglobin, which settles in the form of grains. In the vitreous body, the hemoglobin shell dissolves, the substance turns into hemosiderin, which has a negative effect on the retina.
Hemophthalmos
Description
Vitreous hemorrhage
(hemophthalmos), a manifestation of other diseases, can be caused by rupture of normal blood vessels, bleeding from damaged retinal vessels, bleeding from abnormal new vessels, or spread of vitreous hemorrhage through the retina from other sources. In the elderly, vitreous hemorrhage usually occurs spontaneously and only rarely can be the result of trauma.
ICD-10:
H43.1 Vitreous hemorrhage.
Abbreviations:
CT—vitreous body, CVR—central retinal vein, PVR—posterior vitreous detachment.
Epidemiology.
The incidence of intravitreal hemorrhage in the general population is 7 cases per 100 thousand population per year.
Prevention
? Prevention depends on the disease underlying the pathology. Some conditions, such as AVO (including hemorrhagic AVO, which is the most common cause of spontaneous VT hemorrhage), cannot be prevented. In other cases (for example, with retinal vein occlusion), it is necessary to prevent the development of a similar situation in the other eye
, as well as carry out general treatment to prevent the development of stroke or myocardial infarction.
? This includes treatment of hypertension and hypercholesterolemia
, as well as increased IOP (if it increases). Treatment of arterial hypertension also reduces the risk of myocardial infarction and stroke, the incidence of which is higher in patients who have had retinal vein thrombosis than in the general population. In addition, it has been shown that the administration of antiplatelet agents (acetylsalicylic acid and dipyridamole) reduces the risk of recurrent retinal vein thrombosis in the affected eye and the risk of retinal vein thrombosis in the patient's second eye.
? Careful control of blood sugar and reduction of blood pressure
in diabetics, they reduce the risk of developing microvascular lesions, including diabetic retinopathy and, accordingly, the frequency of intravitreal hemorrhages.
? Early treatment of severe preproliferative or early proliferative retinopathy with argon laser coagulation
can prevent the development of newly formed blood vessels. Moreover, this treatment appears to accelerate the natural progression of AVO by reducing the likelihood of traction of neovascular branches, a major cause of intravitreal hemorrhage. There is an opinion that from this point of view, early vitrectomy is effective in the treatment of diabetic retinopathy, since it makes it possible to remove the CT from the posterior hyaloid membrane - the basis along which the branches of newly formed vessels spread, and the source of traction of these vessels.
Screening.
Hemorrhage in the CT should be suspected and an examination of the organ of vision should be carried out in patients with complaints of the appearance of a floating red or black spot (or spots), “flying spots” before the eyes, cloud-like or cobweb-like shadows in the field of vision, as well as a sharp decrease in vision.
Classification
Intravitreal hemorrhages are divided according to volume, location and stages of disease development.
? By volume
: partial, subtotal and total hemophthalmos.
? By location of hemorrhage
? Retrolental. Between the anterior hyaloid membrane of the CT and the posterior capsule of the lens.
? Paraciliary. Surrounds the posterior peripheral part of the lens.
? Preretinal. Between the posterior limiting membrane of the CT and the retina.
? Epimacular. In the cavity located between the posterior limiting membrane and the retina in the macula area (vitreoschisis).
? Intravitreal. In the cavity ST.
? Combined. Occupies several sections of the ST.
? According to the stages of disease development
(Table 9).
Table 9.
Classification of vitreous hemorrhage by stages of disease development
Etiology
? In the elderly, the most common causes of intravitreal hemorrhage are posterior retinal detachment (with or without retinal tear) (38%); Next in frequency is proliferative diabetic retinopathy (32%) and proliferative retinopathy after retinal vein occlusion (11%). All other reasons combined account for 19%.
? In adults, the frequency of causes is distributed as follows:
: The most common is diabetic retinopathy (39-54%). Other important causes are retinal tear without retinal detachment (12-17%), posterior retinal detachment (7.5-12%), rhegmatogenous (due to retinal tear or detachment) retinal detachment (7-10%) and retinal neovascularization after occlusion of the central vein and its branches (3.5-10%). Also, intravitreal hemorrhage can result from any disease that causes peripheral neovascularization.
? In children, the leading cause of hemorrhages in the CT is trauma (including the “violently shaken baby” syndrome - preretinal hemorrhages - subhyaloid location).
? Causes of intravitreal hemorrhage
? Proliferative diabetic retinopathy (usually T1DM).
? Occlusion of the central vein or its branches.
? Other diseases accompanied by vascular occlusion and proliferative retinopathy (vasculitis, sickle cell anemia).
? Retinal tears, rhegmatogenous retinal detachment (the risk is especially high in patients with high myopia).
? Posterior detachment of the retina with ruptures of the retina and its vessels.
? Exudative form of age-related macular degeneration. ? Malignant choroidal melanoma.
? Microaneurysms of the retinal arteries.
? Retinal tears due to eye trauma [blunt trauma (bruise) or penetrating injury].
? Systemic lupus erythematosus.
? More rare causes
: • aortic arch syndromes; • Terson syndrome - occurs mainly in patients 30-50 years old (intraocular hemorrhages against the background of subarachnoid hemorrhage, occur in approximately 1/3 of patients with subarachnoid hemorrhage, approximately 6% have intravitreal hemorrhage); • open and closed trauma (including shaken baby syndrome, child abuse); • dominant (familial) exudative vitreoretinopathy; • carotid-cavernous fistulas; • Eales disease; • syndromes of increased blood viscosity; chronic leukemia; • incontinentia pigmenti (melanoblastosis, Bloch-Sulzberger syndrome: in 35% of patients the organ of vision is involved in the pathological process: strabismus, cataracts, blue sclera, retinal pseudoglioma); • Norrie's disease is a form of congenital bilateral retinal pseudoglioma; • retinal angiomatoses; • embolism of retinal vessels (for example, talc); • retinal telangiectasia; • retinal vasculitis, including arteriolitis; • retinopathy of prematurity; • sarcoidosis • ulcerative colitis, Crohn's disease; • uveitis, including parsplanitis.
It must be borne in mind that a similar clinical picture may occur with vitreitis
(inflammatory changes in the CT, for example, with uveitis). Symptoms similar to vitreitis can occur even with large cell lymphoma.
Posterior vitreous detachment
.
In 72-79% of cases of hemorrhagic ZOS, concomitant retinal ruptures occur due to increased density of fusion of the CT with the underlying retina. If left untreated, these patients may develop retinal detachment. Posterior vitreous detachment (PVD) in the elderly is caused by age-related changes in the vitreous, consisting of syneresis (liquefaction of the vitreous), as a result of which the posterior hyaloid membrane of the vitreous peels off from the internal limiting membrane. The incidence of AVO
increases significantly between the ages of 50 and 70 years. However, with myopia it occurs more often than with other types of refraction.
Proliferative retinopathy
. Another common cause of hemophthalmos in the elderly is the rupture of newly formed vessels on the optic disc or other localization. Newly formed vessels are a consequence of ischemia in the posterior segment of the eye, leading to the production of angiogenic factors. These vessels are fragile and proliferate along the surface of the partially detached posterior cortex of the CT at sites of vitreoretinal adhesions. Detachment of the CT gel and movements of the eyeball cause traction of the vessels, their tearing, which leads to hemorrhages. The most common causes of ischemia of the posterior segment of the eye are diabetes, followed by retinal vein occlusion and ocular ischemic syndrome [3].
? Proliferative diabetic retinopathy.
Diabetic hemophthalmos is distributed by location as follows: in 34% of cases it is located in the retrohyaloid space, in the CT - in 6% of cases, hemophthalmos of combined localization occurs in 32% of patients. Proliferative diabetic retinopathy is the cause of hemophthalmos in 89% of patients with type 1 diabetes and in 64% of patients in other cases.
? Postthrombotic proliferative retinopathy
. Postthrombotic retinopathy occurs in older age groups (average age about 64 years). Arterial hypertension is present in 88% of patients in this group. Occlusion of the CRVO branch is the most common cause of hemorrhage in the CT (59%), followed by occlusion of half of the CRVO branches (35%) and occlusion of the CRVO (6%). This distribution also reflects the risk of developing neovascularization in the posterior segment of the eye.
Risk factors for retinal vein thrombosis can be divided into local and systemic
.
? Systemic risk factors
include arterial hypertension, diabetes, hypercholesterolemia and hyperviscosity syndromes. Myeloproliferative diseases occur in 1% of patients with retinal vein occlusion.
? Local risk factors
include small optic disc, hypermetropia and branching abnormalities of the retinal vessels.
Other reasons
? Retinal artery macroaneurysms
can also cause hemorrhage in the CT in the elderly, especially in hypertensive patients. They are most common in women. Only 10% of patients with arterial macroaneurysms rupture with hemorrhage in the VT. In most cases, the process resolves spontaneously.
? Breakthrough hemorrhage in the CT
may occur in older patients with age-related macular degeneration and choroidal neovascularization. This condition results from the growth of abnormal blood vessels from the choroid through Bruch's membrane, the retinal pigment epithelium, then into the subretinal space. The disease is considered multifactorial. Neovascularization usually develops close to the fovea and may be accompanied by metamorphopsia (distortion of straight lines), micropsia (the impression that objects are smaller than they actually are), blurred vision followed by sudden complete loss of vision due to subretinal and sometimes intravitreal hemorrhage. The abnormal vessels that form choroidal neovascularization are very fragile. They can easily cause hemorrhage, usually of subretinal localization or located under the retinal pigment epithelium (hemorrhagic detachment of the retinal pigment epithelium). However, sometimes breakthrough hemorrhage in the CT is possible with the development of partial hemophthalmos.
? Finally, even rarer causes of CT hemorrhage in the elderly include choroidal melanoma, Terson syndrome
(intravitreal hemorrhage against the background of subarachnoid hemorrhage, when hemophthalmos is predominantly bilateral), false Terson syndrome (the patient has retinal neovascularization after parsplanitis) and Eales disease (vasculitis of unknown etiology, causing hemophthalmos). Other rare (iatrogenic) causes include perforation of the eyeball during retrobulbar and parabulbar injections (including during local anesthesia during eye surgery), dental procedures, and drug interactions.
Clinical picture
? Cloud-like or cobweb-like shadows in the field of vision, “fog” before the eyes.
? Clots of coagulated blood in the CT, leading to the appearance of moving shadows in the field of view.
? Massive hemorrhage reduces visual acuity down to the level of light perception.
? With a slight hemorrhage in the CT, the patient complains of the sudden appearance of floating opacities
, red or, much more often, black. With more severe hemorrhages, sudden loss of vision is noted. If the cause of hemophthalmos is ZOS, photopsia (the impression of flashing lights) may be present due to mechanical stimulation of retinal ganglion cells by the peeling surface of the posterior hyaloid membrane (traction).
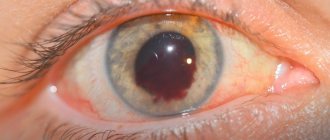
? When examined in transmitted light, the red reflex from the fundus of the eye is muted
, details of the fundus (ONH and retinal vessels) are foggy or indistinguishable. In the anterior parts of the CT, red blood cells can be detected, IOP can be increased, especially in the case of prolonged existence of hemophthalmos. In this case, biomicroscopy of the anterior sections of the CT reveals “ghost-cells” - leached red blood cells. Occasionally, a combination with hyphema is possible, especially if the patient has an intraocular lens and a history of posterior capsulotomy. The cause of intravitreal hemorrhage can be suspected in the presence of rubeosis of the iris, newly formed vessels in the angle of the anterior chamber, posterior synechiae and a relative afferent pupillary defect. In these cases, fundus examination of the second eye may help identify diabetic retinopathy, hypertensive retinopathy, vasculitis, choroiditis, or ocular ischemia.
Diagnosis
? The degree of decrease in visual acuity can vary from a slight decrease to the level of light perception.
? Ophthalmoscopy: moving shadows against the background of a red reflex, details of the fundus are indistinguishable.
Anamnesis
? Complaints of visual impairment (visual disturbances).
? History of ocular trauma, including intraocular surgery.
? General diseases.
Survey
Particular attention must be paid to the following steps
:
? visual acuity;
? biomicroscopy of the anterior segment of the eyeball;
? biomicroscopy of the CT, paying attention to the subject of CT detachment, the presence of pigmented cells in the anterior sections of the CT, condensates, localization of hemorrhage;
? gonioscopy;
? IOP measurement;
? examination of the periphery of the fundus with scleral pressure;
? ultrasound B-scan.
? There are not enough reliable symptoms
, which would make it possible to distinguish ZOS in combination with a retinal tear from ZOS without a retinal tear; therefore, a detailed examination of the periphery of the fundus is necessary: preference should be given to indirect binocular ophthalmoscopy with scleral pressure. Even in cases of fairly dense hemophthalmos, when the posterior pole of the eye is not visualized, the peripheral retina can often be examined using this technique. In some cases, applying a binocular patch for several hours (or even overnight) can allow hemophthalmos to settle and detect retinal breaks. Many patients with retinal tears have pigmented cells in the anterior portions of the CT. Additional information can be provided by biomicroscopy with a three-mirror lens or a small collecting lens for indirect ophthalmoscopy.
? Therefore, the examination should include a thorough medical history.
(life history, general somatic status and existing eye diseases), examination of visual acuity in both eyes, pupillary reaction, biomicroscopy, direct ophthalmoscopy, indirect ophthalmoscopy: careful examination of the periphery of the fundus with a wide pupil with mandatory stereopsis (binocular head-mounted Skepens ophthalmoscope).
To exclude peripheral ruptures, examination with scleral pressure or a three-mirror Goldmann lens
.
? Additional studies include ultrasound of the eye
in cases where the condition of the fundus is difficult to assess due to hemorrhage or opacity of the optical media (for example, corneal opacities, cataracts, etc.). An experienced diagnostic ultrasound specialist can assess the degree of retinal attachment, the presence of a foreign body and CT detachment.
? Diagnosis of the cause of intravitreal hemorrhage
is extremely important, as it determines the tactics and strategy of treatment. As stated above, the most common cause of spontaneous hemophthalmos is hemorrhagic ZOS with or without a retinal tear or retinal detachment. In rare cases, when good visibility of the fundus is still maintained, it is relatively easy to determine retinal breaks, retinal detachment or other pathology of the fundus. Immediate surgical removal of the blood (if indicated) not only improves vision, but also allows for a complete examination of the underlying retina. However, this tactic is permissible only if retinal tears or detachment were detected during an ultrasound examination.
? In the absence of a good view of the fundus, and also in cases where surgical removal of blood is not recommended, it is necessary to rely on B-scan
.
? Dynamic and static B-scan
is carried out to determine the condition of the posterior cortex of the CT, to detect retinal detachment, tumors and newly formed vessels (for example, intraocular melanoma or extensive neovascular membrane). Retinal breaks and branch neovascularization can sometimes be detected on a B-scan, but their absence on a B-scan does not exclude their presence. Additionally, B-scan can be used to differentiate intravitreal hemorrhage from preretinal hemorrhage in diabetics.
? In the absence of an AIA
on a B-scan, the likelihood of retinal rupture or detachment sharply decreases.
In the presence of AVO, as a rule, there is no retinal detachment. However, in this case, a flat local anterior retinal detachment may be missed. The frequency of such false negative conclusions depends on the experience of the diagnostician. False-positive results
may be due to blood covering the posterior surface of the CT, which may be mistaken for retinal detachment. Additional A-scanning and determination of the retina’s proximity to the optic disc (in the case of complete detachment of the optic disc there is no connection with the optic disc) can minimize errors of this kind. There may be other reasons for false positive errors. In particular, the presence of concomitant suprachoroidal hemorrhage and hemorrhagic ZOS may be mistaken for hemorrhagic retinal detachment. The convexital surface of suprachoroidal hemorrhage and its lack of mobility on dynamic B-scan may help differentiate it from retinal detachment. In addition, a combination of suprachoroidal hemorrhage with hemorrhagic-exudative retinal detachment and hemorrhagic ZOS is possible (for example, after systemic administration of streptokinase and tissue plasminogen activator in case of suspected myocardial infarction).
? In the absence of AVR on the B-scan, it is necessary to exclude diabetes and post-thrombotic retinopathy
as a cause of retinal neovascularization. The presence of AOS also does not exclude these diseases, since AOS can appear long before hemorrhage. Careful history taking regarding the time interval between the appearance of floaters and the onset of hemorrhage can help determine the age of AOS.
? If retinal vein thrombosis is suspected
A general blood test is performed, ESR or plasma viscosity is determined to identify syndromes of high blood viscosity. If thrombosis of the retinal veins is suspected as the cause of intravitreal hemorrhage, a study of urea, blood electrolyte composition, creatinine, fasting blood sugar and lipid spectrum is carried out, as well as plasma protein electrophoresis, ECG and determination of thyroid function.
? General examination includes
checking blood pressure, since elevated blood pressure is the most common risk factor for retinal vein thrombosis; also exclude retinal macroaneurysms and unstable diabetic retinopathy.
Treatment
? an urgent consultation with an ophthalmologist is necessary on the same day or the next day after its detection.
. Patients with diabetes who have been diagnosed with proliferative diabetic retinopathy should contact their attending ophthalmologist.
? Minor hemorrhages resolve on their own, without specific treatment.
? The patient is recommended to sleep in a semi-sitting position
so that the blood settles under the influence of gravity and the fundus becomes accessible for inspection.
? In case of proliferative retinopathy and retinal breaks due to posterior detachment of the retina, laser coagulation of the retina is performed
(immediately or after restoration of CT transparency).
? If there is a significant violation of the transparency of the CT, detachment can be diagnosed using ultrasound
.
? Vitrectomy
indicated if the transparency of the CT is not restored, as well as immediately when retinal detachment occurs. Treatment of intravitreal hemorrhage includes treatment of the cause that caused it, the hemorrhage itself and possible complications.
? In case of a confirmed retinal tear, retinal detachment or other fundus pathology, laser or surgical treatment
(vitrectomy).
? In the case of fresh hemorrhagic AVO and the absence of other pathological changes according to B-scan data, the doctor is faced with a dilemma. As mentioned, B-scans can easily miss
small retinal tears and flat anterior retinal detachment. In this case, the patient is at risk of losing central vision due to involvement of the central vein in the detachment in the distant future.
? Maintaining
in such cases it should be conservative or proactive (preemptive tactics).
? Conservative management includes close observation with serial ultrasound examinations
to identify any progressive retinal detachment before the center is involved; observation should be regular until spontaneous clearing of hemophthalmos, which would allow a complete examination of the retina.
? Proactive management
includes early vitrectomy, removal of intravitreal hemorrhage in order to conduct a detailed examination of the retina. In the presence of retinal tears, laser treatment is performed, and in case of retinal detachment, the necessary surgical intervention is performed. Although the proactive approach has its advantages due to the possibility of detailed intraoperative examination of the retina and improved vision in the postoperative period, it also has disadvantages due to the risk of complications associated with vitrectomy and the almost inevitable development of cataracts.
? Most hemophthalmos resolves on its own; however, complications are possible, including secondary hemolytic glaucoma
, the so-called “shadow” cell glaucoma, or “ghost cells”, and blurred vision due to the slow removal of cellular debris from the CT. Vitrectomy can be performed for both conditions. Occasionally (after vitrectomy in a patient with diabetic retinopathy), despite adequate laser treatment and the absence of neovascularization in the posterior pole of the fundus, relapse of hemophthalmos may occur. In these cases, it is believed that tufts of neovascularization develop at the sites of the perforations associated with the vitrectomy. In such cases, CT rinsing may be necessary. The use of tissue plasminogen activator and volumetric homeostatic fluid-liquid exchange is described.
? Finally, repeated injections of low doses of alteplase
in rabbits they provide rapid resorption of intravitreal hemorrhage within 2-3 weeks without signs of toxic effects on the retina. However, other studies of intravitreal tissue plasminogen activator have shown a modest effect with an increased incidence of tractional retinal detachment.
? Application of prourokinase
- proenzyme plasminogen activator of the urokinase type) has shown effectiveness in the treatment of partial hemophthalmos in the period of occurrence from 3 days to 4 weeks from the moment of development of hemophthalmos. In case of subtotal and total hemophthalmia, treatment with fibrinolytics is ineffective and vitrhemectomy is indicated.
Patient education
especially important for proliferative diabetic retinopathy and recurrent hemophthalmos. In case of a floating red or black spot (or spots), “flying spots” before the eyes, cloud-like or cobweb-like shadows in the field of vision, as well as a sharp decrease in vision, the patient is recommended to take 10% calcium chloride solution orally; cold should be provided to the eye area for 2-3 hours, rest (bed rest). Urgent contact with an observing ophthalmologist.
Further management.
Treatment of diseases that are the cause of intravitreal hemorrhage. Prevention of recurrence of hemophthalmos and hemorrhage in the fellow eye.
Forecast
The prognosis depends on the cause of the hemorrhage, although most small hemorrhages in the CT tend to resolve gradually. The volume and location of hemorrhage are also of great importance for the course and outcome.
? Hemorrhages
, occupying less than 1/8 CT (according to B-scan), in most cases resolve completely or almost completely.
? Blood soaking
from 1/8 to 1/4 of the CT volume is dangerous due to mooring, increasing the risk of retinal detachment.
? If the hematoma occupies from 1/4 to 3/4 of the CT, then the prognosis for visual functions is usually questionable. Without timely surgical intervention (in combination with fibrinolytic therapy), MT fibrosis and tractional retinal detachment appear in the later stages.
? Total hemophthalmos
(blood occupies more than 3/4 of the volume of the eye), as a rule, leaves no hope of saving the eye.
Application
Principles of treatment of non-traumatic hemophthalmos
The main goals of treatment are to accelerate the processes of hemolysis and fibrinolysis
, removal of fibrin degradation products, detoxification of hemoglobin, normalization of the pH of the environment, reducing the amount of protein and cholesterol in the eye cavity.
? With fresh hemophthalmos
A binocular bandage is applied, bed rest is prescribed, and cold is applied to the eye area for 2-3 hours.
? In the first 1-3 days, hemostatic agents
: ethamsylate intramuscularly (12.5% solution, 2 ml), or orally, menadione sodium bisulfite, 0.015 g, or 10% calcium chloride solution.
? To accelerate hemolysis and remove “slags” from the eye cavity, osmopreparations are administered parenterally
: glycerol or mannitol, hypertonic solutions of glucose and sodium chloride. For the purpose of detoxification and treatment of hematogenous siderosis, intravenous infusions are used: “povidone + sodium chloride + potassium chloride + calcium chloride + magnesium chloride + sodium bicarbonate”; or drugs that bind iron - dimercaprol (5% 5.0 ml, No. 10, i.v.), or edetic acid (disodium salt, 3.8%, 1 ml s.c.).
? enzyme preparations are used 2-3 days after the occurrence of hemorrhage
. The drugs of choice are plasminogen activators: prourokinase, administered parabulbarly at 5000 IU. To prepare the injection solution, the contents of the ampoule are dissolved ex tempore in 1 ml of physiological solution.
? Systemic enzyme therapy
includes "wobenzym" or "phlogenzyme". "Wobenzym" is used 8-10 tablets 3 times a day for 2 weeks, then 2 weeks 7 tablets 3 times a day for several months. The pills are taken 30-60 minutes before meals, washed down with plenty of water. "Flogenzyme" is used 2 tablets 3 times a day for several months. The pills are taken 30-60 minutes before meals, washed down with plenty of water.
? Methylethylpyridinol is used as a retinoprotector
. This drug has a wide range of biological properties: it inhibits free radical oxidation, actively interacts with the products of lipid and protein peroxidation, stabilizes cell membranes, inhibits platelet aggregation, and inhibits the transition of fibrin monomer to fibrin polymer. The drugs are administered subconjunctivally or retrobulbarly. Pentahydroxyethylnaphthoquinone also has an antioxidant effect (0.02% solution administered parabulbarly).
? If on the 10th day no effect is observed from the treatment, it is necessary to decide on the advisability of surgical intervention
.
If the reaction is positive (the CT becomes more transparent, a pink reflex appears from the fundus, visual acuity improves), it is necessary to proceed to the next stage of conservative treatment. Since, starting from the 10th day, hemophthalmos enters the proliferative-dystrophic stage, treatment should be aimed at preventing gross mooring. For this purpose, enzymes with pronounced proteolytic activity
:
? collalysin
administered parabulbarly at 30 IU. To prepare an injection solution, the contents of the ampoule are dissolved ex tempore in 10 ml of physiological solution or
? hyaluronidase
(administer 32 units by electrophoresis).
? Use systemic vitamin therapy
: intramuscular ascorbic acid 2.0 ml, pyridoxine 1.0 ml, riboflavin 1.0 ml or thiamine 1.0 ml.
—-
Article from the book: Clinical guidelines - ophthalmology | Moshetova L.K., Nesterova A.P., Egorova E.A.
How is hemophthalmos formed?
Under the influence of damaging factors, the integrity of the vessels of the eye is disrupted, as a result of which blood accumulates in the vitreous body. Red blood cells begin to break down, deposited in grains. Such processes harm all adjacent structures, but more so the retina.
Stages of hemophthalmos:
- Bleeding (first day after injury). Blood enters the vitreous cavity and reduces its transparency.
- Fresh hematoma (two days). Blood clots form.
- Toxic-hemolytic (3-10 days). The process of clot destruction begins. Decay products enter other elements of the eyeball through diffusion. Complete opacification of the vitreous body occurs.
- Proliferative-dystrophic (10-180 days). Dystrophy of the retina, lens and other structures develops. The hematoma fills with connective tissue and becomes denser.
- Intraocular fibrosis (after six months from injury). The vitreous thickens, being replaced by connective tissue. The risk of retinal detachment increases. As a result, the eyeball atrophies and blindness occurs.
Signs of hemophthalmos
The occurrence of hemophthalmos is accompanied by opacities that float in the field of vision, blurring, intolerance to light, and the appearance of cobwebs or shadows in front of the eye. With small hemorrhages, many dark “spots” appear in the field of vision; with moderate hemorrhages, clearly visible dark stripes appear, which can reduce visual acuity, sometimes to the point of light perception. Most often, with hemophthalmia there is no pain, with the exception of cases of trauma and neovascular glaucoma. In the presence of concomitant pathology, the symptoms of intraocular hemorrhage may vary according to its nature, course and stage of development.
Causes of intraocular hemorrhage
Most often, the cause of hemophthalmos is a defect in the formation of blood vessels, in which they quickly rupture. This condition is typical for severe retinal damage in patients with diabetes mellitus. This problem occurs when blood flow in the retina is disrupted during postthrombotic retinopathy. The growth of defective vessels is also observed with dystrophy of the center of the retina and tumors of the choroid of the eyeball.
Causes of hemophthalmia:
- glaucoma;
- macular degeneration;
- damage to the eyeball;
- retinal or vitreous detachment;
- diabetic retinopathy;
- vascular thrombosis;
- hypertensive crisis (sudden increase in blood pressure);
- eye surgeries;
- neoplasm in the eyeball;
- autoimmune pathologies that cause vascular inflammation;
- abnormal development of eye vessels.
The cause of hemophthalmos can be injuries of a different nature: penetrating with destruction of membranes and blood vessels, as well as contusions and blunt trauma. Hemorrhages are often diagnosed when the retina is ruptured or detached when the retinal vessels are damaged. The most pronounced symptoms will be detachment of the posterior hyaloid membrane in those places where the vitreum is tightly attached to the vessels.
Hemophthalmos may indicate a disease of the circulatory system. Hemorrhages in the eye are often observed with hypertension, sickle cell anemia, vasculitis, vascular inflammation and oncological blood diseases.
Sometimes blood enters the vitreum from the subretinal space. This happens with the development of uveal melanoma or age-related macular degeneration. Hemophthalmos is possible with Treson syndrome, when subarachnoid hemorrhage occurs. In this case, the retinal vessels rupture due to a sharp jump in intracranial pressure.
In children, hemophthalmos develops as a result of shaken baby syndrome. Parents can cause hemorrhage even with a slight shake of the baby in an attempt to calm him down.
It is extremely rare that hemophthalmos is caused by uveitis, Eales' disease, sarcoidosis, chronic leukemia, Crohn's disease, and retinopathy in prematurity. Bleeding disorders and long-term anticoagulant therapy do not usually lead to hemophthalmos.
Causes
There are a large number of different factors that contribute to the occurrence of hemorrhages.
The main causes of hemophthalmos are as follows:
- eye injury as a result of injury resulting in rupture of the eye membranes and blood vessels;
- complication after eye surgery;
- rupture of newly formed vessels that occurs in patients with decompensated diabetes mellitus, in people with circulatory disorders in the retinal vessels;
- retinal detachment, accompanied by rupture of blood vessels;
- vasculitis;
- persistent increase in blood pressure;
- sickle cell anemia.
The disease often causes spontaneous vision loss, as blood clots prevent the light ray from passing to the retina. Whether vision is lost completely or partially depends on the volume of blood accumulated in the vitreous. After a few days, the hemoglobin in the blood cells is destroyed, the red blood cells become discolored, and therefore vision is completely restored. But without appropriate treatment, the process will be repeated again and again until the breakdown products of red blood cells and constant hemorrhages lead to atrophy of the eyeball.
Symptoms of hemophthalmos
With severe hemorrhage, visual acuity is critically reduced, even to the point of blindness. The degree of decrease in visual acuity depends on the amount of blood in the vitreum. In severe cases, only light perception is preserved. If the hemorrhage is caused by retinal detachment, patients see flashes of light of different types (lights, lightning, sparks). This is the phenomenon of photopsia.
An eye examination reveals the presence of a granular mass of blood behind the lens. The structure of the vitreous body is not determined. Resorption of blood clots leads to destruction of the vitreous body, it becomes liquefied. Fibrils (protein structures in tissues) thicken and swell, becoming covered with blood grains, red blood cells and other decay products.
With hemophthalmia, patients complain of cobweb-like and rounded shadows appearing in the field of vision. The effect of blurred vision appears. Shadows are usually dark red or black in color. When the eyes move, the blood clots move, causing the shadows to shift.
Symptoms
The clinical picture of hemophthalmos depends on the stage of development of the disease and the volume of blood accumulated in the vitreous area.
Patients with hemophthalmia experience the following unpleasant symptoms:
- sensation of cobwebs in the eyes;
- floating black spots before the eyes;
- blurred vision;
- fear of bright light.
Symptoms vary depending on the stage of ophthalmological pathology. At the bleeding stage, patients note the appearance of fog before the eyes, which is gradually replaced by cobweb-like or cloud-like shadows (red or black).
Numerous black spots in front of the gases indicate minor hemorrhages, dark stripes in front of the eyes indicate a moderate hemorrhage. If the disease has reached a pronounced degree, vision is greatly reduced, often a person sees only light, without distinguishing objects. Hemophthalmos does not cause pain, the only exception being cases when it is caused by glaucoma or injury to the organs of vision.
Diagnosis of hemophthalmos
The patient can help the doctor make a diagnosis by providing details about how and when the symptoms began. It is very important to mention all injuries that occurred, as well as associated pathologies.
An ophthalmologist should conduct an initial examination. Methods for diagnosing hemophthalmos include biomicroscopy using a slit lamp, when the doctor examines the structures of the eyeball and the fundus. With hemophthalmos, you can notice hemorrhages under the conjunctiva and in the anterior chamber of the eye, between the cornea and iris.
Ophthalmoscopy allows a more detailed examination of the fundus of the eye, which is fundamentally important for determining the cause of hemorrhage and choosing treatment. In case of partial hemophthalmos, floating blood clots are detected in the vitreum, which do not interfere with examination of the fundus. Complete hemophthalmos covers the bottom of the eye, there is no red reflex (reflection of light from the retina through the transparent media of the eye).
The condition of the retina and vitreous body can be analyzed using ultrasound scanning. Ultrasound helps determine the nature of hemophthalmos, and during chromatic electroretinography the functionality of the retina is checked.
Diagnostics
To identify partial, total, subtotal hemophthalmos of the eye, you need to undergo a thorough examination by an ophthalmologist. Initially, the doctor will ask about the presence of diseases that contribute to the appearance of hemophthalmos and eye injuries. Using various studies, the presence of blood clots in the vitreous body and the area that surrounds it is established.
Instrumental diagnostics include:
- indirect binocular ophthalmoscopy with scleral punching, which is used to examine the peripheral parts of the retina for retinal breaks;
- ophthalmoscopy with a Goldmann lens;
- visometry to determine visual acuity;
- biomicroscopy to identify foci of hemorrhage and condensation in the anterior parts of the vitreous;
- B-scan, which helps to study the condition of the posterior vitreous;
- Ultrasound of the eye. Helps to see ruptures of the ocular vessels during the traumatic genesis of hemophthalmos, to assess the degree of vitreous detachment, and the retinal fit. It is prescribed if it is impossible to examine the retina due to clouding of the cornea, cataracts, or severe hemorrhage.
All patients are prescribed standard tests, including determination of blood glucose, general blood and urine analysis, and coagulogram.
Conservative treatment of hemophthalmos
Small foci of hemophthalmos tend to resolve, but this is a very slow process. In some cases, complete resorption does not occur. Total and subtotal hemophthalmos is an indication for hospitalization of the patient. Treatment of partial hemophthalmia can be carried out on an outpatient basis. The course of treatment will depend on the cause of the vitreous hemorrhage, so it is important to make the correct diagnosis.
Therapy for hemophthalmos is always the same, but partial hemorrhage, as a rule, does not require great intensity and surgical intervention. You should prepare in advance for the fact that the treatment will be long, and it must be completed.
Principles of treatment
- If the hemorrhage has occurred recently, the patient is advised to rest in bed and wear a cold bandage.
- To avoid new hemorrhages, calcium supplements are prescribed (calcium gluconate 10% intramuscularly and calcium chloride drops 3% locally).
- Additionally, you can take vitamins B2, C and PP, as well as Dicinone and Vikasol.
- After 1-2 days from the start of treatment, enzyme preparations are prescribed to resolve clots. These are eye drops with potassium iodide, lidase or ronidase solution (0.1%).
- To prevent the formation of strands, hormonal therapy (eye drops or injections under the conjunctiva) is prescribed. For these purposes, use a solution of Dexamethasone (0.1%) or Prednisolone (0.3%). Parabulbar injections of collalysin, an enzyme preparation that dissolves collagen, are effective. You need to make 10 injections every other day. Additionally, injections of enzymes (Lecozim, Fibrinolysin) are prescribed.
- Anticoagulant therapy is recommended to prevent blood clotting. Solutions of heparin and streptodecase are injected under the conjunctiva.
- To enhance the resorption effect, sodium iodide solution (10%) is administered intravenously.
- It is possible to use autohematotherapy. 2, 4, 6, and then 8 ml of blood from a vein are injected intramuscularly.
- Sometimes medications with aloe extract are prescribed.
- We must not forget about physical therapy. For hemophthalmia, lidase electrophoresis is indicated (15 procedures, 15 minutes each). A month later, potassium iodide electrophoresis is performed with the same frequency.
- Additionally, phonophoresis of heparin and potassium iodide is prescribed.
- Laser treatment of hemophthalmos is possible.
- The effectiveness of hirudatherapy cannot be denied.
In cases where drug treatment is ineffective within 7-10 days, surgical treatment of hemophthalmos is required. Without treatment, strands begin to form in the eye, which provoke retinal detachment and atrophy the eyeball. Lack of therapy or its ineffectiveness is a sure path to complete blindness.
With complete and timely treatment of partial hemophthalmos, the prognosis is favorable in most cases. Conservative therapy promotes resorption of hemorrhage areas and restoration of vision. Subtotal and total hemophthalmos require urgent and powerful treatment, otherwise the risk of complications reaches one hundred percent.
Treatment
Treatment of a pathological condition is based on the cause of its occurrence. The last two stages of the disease are treated exclusively in the hospital, the patient is placed in an inpatient department. The patient must remain in bed with the obligatory application of a sterile bandage.
In case of partial form, therapy is conservative; in case of subtotal and total form, surgical intervention may be required. For example, vitrectomy.
If you are bleeding, do not engage in physical activity or take blood thinning medications. Medicines are prescribed to stop bleeding. This is Dicion, calcium chloride, Etamsylate. After the patient is discharged from the hospital, treatment continues. The patient is prescribed medications to prevent recurrence of hemophthalmos.
These are medications with vitamins and calcium. For example, Vikasol, Dicion.
During therapy, an ultrasound of the eyes is performed. If the examination shows clots, enzyme agents are prescribed. They are administered by injection under the lower eyelid.
Additionally, medications are prescribed that strengthen the vascular walls - Riboflavin, Ascorbic acid, Pyridoxine. For partial and total hemophthalmia, retinoprotectors are prescribed. These products protect the retina from damage.
Surgical treatment of hemophthalmos
Since complications of hemophthalmia are extremely dangerous, only 10 days are allocated for conservative therapy. If treatment does not help during this period, surgical removal of blood from the vitreous body is prescribed.
One of the main methods of treating hemophthalmos is vitrectomy. The operation involves removing the vitreous and replacing it with a gel-like substance. This procedure helps prevent retinal detachment.
Removing the vitreous and filling the cavity with a special solution eliminates the problem of retinal tension. The solution presses the retina against the walls of the eye, maintaining its normal position. In this way, it is possible to prevent repeated hemorrhage and stop the growth of pathological vessels. Vitrectomy does not require hospitalization of the patient, despite the fact that it is a complex microsurgical operation. The procedure takes 1-2 hours.
Types of hemophthalmos
Various amounts of blood can flow into the vitreous body. It may be a few drops or the blood permeates its entire mass. Depending on the volume of blood shed, the following types of hemophthalmos are distinguished:
- Partial – less than a third of the vitreous;
- Subtotal – from one to two thirds;
- Total – more than two-thirds of the volume of the vitreous.
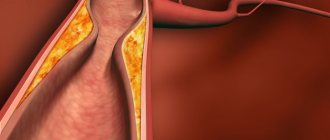
Fig.1 Presence of blood in the eye (1/3 filled - partial hemophthalmos)
Depending on which part of the eye the hemorrhage is localized, there are anterior, posterior, median and mixed hemophthalmos. In relation to the walls of the eye, central, parietal and hemorrhage are distinguished.
Hematoma goes through four stages of evolution, which are presented in Table No. 1
Table No. 1. Stages of evolution of intraocular hematoma
| Stage No. | Name | Duration |
| I | Fresh hematoma | From a few minutes to 48 hours |
| II | Toxic-hemolytic | From 3 to 10 days |
| III | Proliferative | From 10 days to 6 months |
| IV | Fibrosis | More than six months |
According to ultrasound data, low, medium and high density hemorrhages are distinguished.
Complications of hemophthalmos
A frequent complication of hemorrhage in the eye is severe destruction of the vitreous body. It happens that hemophthalmos becomes recurrent, provoking the formation of connective scar tissue in the vitreum. With prolonged intraocular hemorrhage, children often develop amblyopia and myopic shift.
Hemophthalmos can be complicated by hyphema. This is a hemorrhage in the anterior segment of the eyeball, which is localized between the iris and cornea. Even if prolonged hemophthalmos has not led to significant damage to the retina, and normal vision is preserved, the risk of developing secondary glaucoma increases.
Hemorrhage into the vitreous body can be prevented by timely treatment of pathologies that can cause hemophthalmos. It is very important to follow safety precautions and protect your eyes from damage.
Sources used:
- Changes in the fundus of the eye in internal diseases / M.G. Margolis, B.V. Pluzhnichenko. - Moscow
- Bloodstream of the ciliary body of the eye: monograph. / Alexey Pryakhin. - M.: LAP Lambert Academic Publishing, 2013.
- Clinical ophthalmology. Systematized approach / Jack Kansky. - M.: Logosphere, Elsevier Urban & Partner, 2009.
- International Council of Ophthalmology
Prognosis and prevention
Currently, scientists have not developed specific measures to prevent hemophthalmos. Patients are recommended to monitor blood pressure levels, and after forty years, measure intraocular pressure once a year. An effective method for preventing hemophthalmos in patients with diabetes is systematic monitoring of blood glucose levels. They should undergo adequate therapy for the underlying disease and visit an ophthalmologist twice a year for a preventive examination. If necessary, our specialists can perform laser coagulation of blood vessels and reduce the risk of developing the disease.
With hemophthalmia, the prognosis depends on the volume of blood poured into the vitreous body. Only early detection of hemorrhage and timely treatment make it possible to restore full eye function. A favorable prognosis is when the vitreous body is filled with blood to 1/8. If blood soaks from 1/8 to 1/4 of its part, the risk of retinal detachment is high. With hemophthalmia of 1/4 - 3/4 of the vitreous, the prognosis for vision restoration is questionable. If total hemophthalmos has developed, it is not possible to restore vision without surgery. 95% of patients develop atrophy of the eyeball. This further leads to complete blindness and disability.
Symptoms of the disease
Signs of hemophthalmia of the eye are determined by the volume of blood that enters the eye, as well as the stage of the pathology and its characteristics. Bleeding can last from a couple of seconds to a day, during which patients notice moving dots in front of the eyes, floating fog and other visual effects. The main feature that distinguishes hemophthalmos is sudden complete clouding, as well as black and red shades before the eyes. The level of clarity reduction is determined directly by blood filling. With extensive bleeding, patients cannot distinguish even bright lighting at all.
The most characteristic symptoms
Based on the severity of the disease, the patient feels the following symptoms:
- moving multi-colored dots and threads before the eyes;
- decreased vision, loss of sharpness, while vision improves in the morning only after waking up. This fact is explained by the fact that during a long stay in a horizontal position, blood collects in the lower compartment of the organ of vision;
- significant deterioration of vision, when the patient does not see objects, but distinguishes only between dark and light times of day.
In the case of small hemorrhages, the clarity of vision in patients decreases insignificantly, and ganglion cells against the background of retinal detachment provoke the development of photopsia. Noticeable pain occurs in the case of hemophthalmos of the eyes after significant trauma or iatrogenicity.
Therapeutic measures
Treatment of hemorrhages in the intraocular media is prescribed in accordance with the cause of hemophthalmos. Thus, quickly determining the cause of the incident is the primary goal for specialists.
Currently, there are no medications with proven effectiveness for the treatment of hemophthalmos. Therefore, in the presence of breaks caused by proliferative diseases of the retina, laser or cryocoagulation is performed. An alternative to retinal coagulation can be injections into the vitreous body of certain drugs that suppress vascular growth factors (Avastin, Lucentis, Eylea). In the case of retinal detachment, surgical treatment of the pathology is carried out as quickly as possible.
One of the surgical treatment options for hemorrhage inside the eye is vitrectomy. This is an operation in which partial or complete removal of the vitreous humor is performed. Vitrectomy is indicated:
- For hemophthalmia caused by retinal detachment;
- If the transparency of the vitreous body is not restored for more than 2-3 months;
- When bilateral hemophthalmos is diagnosed and/or there is a suspicion of a traction component, in young patients with diabetes or in healthy children to prevent amblyopia;
- For hemophthalmia accompanied by rubeosis, hemolytic glaucoma or shadow cell glaucoma.
Patients with hemophthalmia are advised to be hospitalized and bed rest on a bed with the head end elevated. As a rule, the attending physician will stop taking anticoagulant drugs (aspirin), if they were taken previously. A complete restriction of physical activity is recommended. The prognosis for treatment of hemophthalmos is directly related to the cause of hemorrhage.
Conservative treatment options
Conservative methods involve the use of the following measures:
- on the first day you need to apply cold to the eyes, which will reduce the manifestations and narrow the eye vessels;
- drops in the eyes and injection of drugs with calcium chloride, B vitamins to reduce the amount of bleeding;
- blood clot-absorbing medications for 1-2 days (potassium iodide, lidase, lecozyme, streptodecase), which reduces the visible signs of hemophthalmos;
- hirudotherapy.
Partial hemophthalmos implies a favorable prognosis; with total pathology in the eyes, the outcome depends on the timeliness of contacting a specialist and the speed of application of measures. That is, the sooner the patient applies and begins to treat hemophthalmos of the eye, the more favorable the doctors’ prognosis.