One of the severe and frequent complications of diabetes is diabetic retinopathy. It is characterized by damage to the vessels of the retina, in which vision is severely deteriorated until it is irreversibly lost. There are three stages of this disease: non-proliferative, pre-proliferative and proliferative. Let's find out how they manifest themselves and are treated.
In this article
- Causes of diabetic retinopathy
- Stages of retinopathy in diabetes mellitus
- Non-proliferative stage of diabetic retinopathy
- Preproliferative diabetic retinopathy
- Proliferative retinopathy in diabetes mellitus
- Retinopathy in diabetes mellitus: diagnosis
- Diabetic retinopathy: treatment
- Nutrition for diabetic retinopathy
Diabetes mellitus, which is diagnosed in approximately 5% of the world's population, can lead to the development of dangerous complications. One of them is diabetic retinopathy, which is caused by damage to the vessels of the retina. An increase in blood sugar levels leads to the destruction of vascular walls, including in the eyes. This inevitably affects vision.
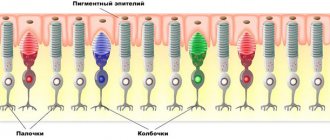
The retina is involved in primary information processing. Light rays are collected on it, which are then refracted, passing through the cornea and lens. Next, the information enters the brain, and we see the picture at which our gaze is directed. Even minor damage to the inner lining, or retina, which is the thinnest structure of the eyeball, causes a decrease in visual function.
Moreover, such disorders are diagnosed in almost all patients with diabetes. But ophthalmological signs appear several years after this diagnosis. After just two years, symptoms of diabetic retinopathy are observed in 15% of diabetics, after 10-15 years - in almost half of patients, and after another 20-30 years - in 90-100% of patients. It does not matter at all what type of diabetes a person has - insulin-dependent or non-insulin-dependent. The danger of the pathology is that it can lead to complete blindness, which cannot be cured.
It happens that the patient does not notice ophthalmological signs or ignores them for several years. This is due to the slow progression of the pathology. However, there may also be rapid development. This is due to the patient’s lifestyle and the presence of other diseases.
Causes of diabetic retinopathy
Diabetic retinopathy in diabetes mellitus occurs due to increased blood glucose levels, that is, glycemia. It causes oxidative stress, the production of free radicals, which increases vascular permeability. This is the main reason. There are a number of predisposing factors that contribute to the development of diabetic retinopathy. Among them:
- hypertension;
- genetic predisposition;
- smoking;
- alcohol consumption;
- pregnancy and lactation period;
- kidney pathologies.
The risk of diabetic retinopathy increases with age. This disease is diagnosed more often in older people. All these factors, combined with an increase in blood sugar levels, negatively affect the condition of blood vessels. Oxygen delivery to tissues deteriorates.
The retina is one of the most sensitive structures of the eyeball and the entire body, especially to the blood supply. Lack of nutrients leads to changes in the fundus of the eye and deterioration of vision. The nature of the damage depends on the stage of diabetic retinopathy.
Classification
Source: noalone.ru Retinopathy is a non-inflammatory lesion of the retina caused by vascular disorders.
The main cause of this disease is impaired blood circulation in the vessels of the eye. Retinopathy can be a complication of various pathologies, for example, hypertension, diabetes. Important
The progression of this disease sometimes leads to partial or complete loss of visual function of the eye. For many people, complete loss of vision is one of the worst life scenarios. Partial loss of visual function can also cause many fears.
Of course, when the situation has already arrived, there is nothing to be afraid of, all that remains is to live with it. But if this disease is in its early stages, or you know that you are predisposed to it, it is important to understand the mechanisms that cause it.
The retina is the inner layer of the eye, which has a wide vascular network. The small vessels in the retina can become damaged due to a number of factors, such as high blood pressure (hypertension). Retinopathy can also be caused by microcirculatory disorders, which are caused by a diabetic shift in metabolism.
The disease also occurs against the background of extensive abnormal growth of blood vessels - as a consequence of early birth (retinopathy of prematurity). Let us consider the types of this disease and the mechanisms of its occurrence in more detail. Types of retinopathy: hypertensive retinopathy; diabetic retinopathy; retinopathy of prematurity.
Hypertensive retinopathy
It appears against the background of damage to the microarteries of the eye, which are provoked by high ocular pressure. Compression of the arteries and veins of the eye, pathological changes in the walls of blood vessels and the points where the vessels intersect, hemorrhages, microaneurysms - all these are signs of hypertensive retinopathy.
Sick people may not immediately notice any changes; in the initial stages, patients complain only of pain in the head and a slight deterioration in the visibility of objects. The last degree of hypertensive retinopathy is accompanied by swelling of the optic nerve.
Diabetic retinopathy
This pathology is one of the most severe complications of diabetes. The mechanism of its occurrence is complex: it is associated both with hereditary characteristics of the vascular structure and with changes in metabolism. In diabetes, unwanted substances enter the retina of the eye.
Metabolic disorders lead to increased blood flow. Next, the inner surface of the vessels is affected, which, in turn, leads to blockage of the capillaries. Microaneurysms then form, causing capillaries to grow pathologically in places where they shouldn’t exist.
Then hemorrhages begin in the eye. Some of the capillaries are destroyed, and degeneration of the eye vessels occurs (the vascular structure becomes simpler). There are several degrees of diabetic retinopathy. The first degree is expressed by hemorrhages and swelling of the retina.
The second is characterized by venous and capillary anomalies, large accumulations of blood inside the retina. The third degree is manifested by the proliferation of blood vessels, hemorrhages into the vitreous body of the eye.
Newly formed vessels are usually very fragile; they cannot withstand the pressure of blood flow and rupture, which leads to retinal detachment. In the initial stages, people have no symptoms noticeable in the eye.
A sharp deterioration in visual function and loss of vision indicate that the process has already gone too far.
Retinopathy of prematurity
This disease usually occurs in very premature babies. Common causes of the disease: inflammatory gynecological diseases in the mother of the child, bleeding during childbirth; fetal pathology, etc.
Until the age of six months, retinopathy occurs actively - in the form of changes in the arteries and veins. Hemorrhages into the vitreous body and retinal detachment accompany the first period of the disease.
Then, from six months to a year, a period of reverse development occurs. After one year, during the scar period, children develop myopia with ruptures and detachments of the retina; the eyeballs become smaller and the eye pressure increases.
Treatment for retinopathy depends on the factors that trigger it. Depending on the type of retinopathy, various steps are taken to prevent its progression.
Factors that provoke changes and degeneration of the vascular network of the eye (diabetes, hypertension or prematurity) are themselves quite significant and can lead to serious consequences. You have to deal with the consequences of these factors for the rest of your life.
Important
The causes of diseases leading to retinopathy are extensive. Causes of hypertension and its consequences Sedentary lifestyle, smoking, diabetes, excessive consumption of table salt and alcohol are all common risk factors that can trigger hypertension.
Hypertension also occurs with background unstable mental activity. No one is immune from the occurrence of this disease, because it occurs due to a violation of the mechanism of excitation - inhibition of the nervous system.
Difficult relationships with people, disrupted work and rest schedules can become a trigger for the development of hypertension. Constant stress due to an unfavorable situation in the family or at work, the inability to relax and, as a result, the desire to reduce the emotional stress with alcohol or cigarettes - this situation is familiar to many.
Of course, a negative emotional climate forces you to use means that help you calm down. Cigarettes and alcohol help quickly change your internal state. But what about the condition of the blood vessels? Gradually, the cardiovascular system works worse and worse, which entails new difficulties, including eye problems.
There is a definite relationship between the degree of retinopathy and patient mortality. A small percentage of people with advanced retinopathy survive more than four years after diagnosis.
How to treat hypertensive retinopathy? All actions of doctors when making such a diagnosis are aimed at preventing damage to the blood vessels of the eye by reducing pressure.
Patients take appropriate medications, because without them, the load not only on the eyes, but also on the vessels of other vital organs increases significantly.
The human heart can function at high voltage for a limited time, so treatment of hypertension and hypertensive retinopathy is directly related to the prevention of death.
Diabetes occurs against the background of a disorder of the pancreas. The genetic predisposition of people to this disease is the cause of diabetes. Diabetes can also be caused by pregnancy (gestational diabetes), infections, and improper medication use.
The number of people with this pathology is growing, and some do not even know that they have it. The complications associated with diabetes are extensive, because they affect the entire human body: kidneys, eyes, nervous system and other organs and organ systems.
Damage to small and large blood vessels, deterioration of oxygen metabolism in tissues, damage to the arteries, disorders of the nervous system, kidney disease caused by metabolic disorders, increased susceptibility to injuries to the soft tissues of the foot - all these are complications of diabetes.
As for retinal lesions, they most often correlate with kidney lesions. This is a late complication and often leads to blindness in older people with diabetes.
How to treat diabetic retinopathy? Diabetic retinopathy is treated through the joint efforts of several doctors, most often an endocrinologist and an ophthalmologist. A proper diet is of great importance, the general meaning of which is to exclude the intake of easily digestible carbohydrates (sweets, etc.).
It is also recommended to take in food substances that help normalize fat metabolism. A considerable share is given to the use of vitamins that strengthen the walls of blood vessels. In the second and third degrees of this disease, treatment using pulsed light (photocoagulation) is indicated.
During such sessions, the vessels heat up and the blood in them coagulates. Causes of prematurity and its consequences The factors leading to premature birth are extensive. These are various diseases of the mother, including gynecological, infectious and endocrine.
Poor nutrition, bad habits, too early or late age of a woman - all this can provoke premature birth. Retinopathy of prematurity occurs against the background of various processes.
An unfavorable external environment, excessive amounts of light or oxygen lead to the proliferation of eye vessels. The growth of blood vessels and connective tissue causes retinal detachment.
How to treat retinopathy of prematurity? With this disease, infants are advised to undergo frequent ophthalmological examinations. Doctors, as a rule, prescribe several types of treatment: instillation of drops, laser correction of the retina or its correction using liquid nitrogen, removal of the vitreous.
In the early stages, in most cases the disease resolves spontaneously. Other causes of retinopathy Lesions of small vessels of the eye often occur against the background of intense work activity, colds, wearing glasses and contacts.
It’s good if burst blood vessels only cause aesthetic inconvenience - it goes away. In cases where retinal vascular ruptures are the background consequences of serious diseases and disorders, their treatment requires a serious and comprehensive approach.
Non-proliferative stage of diabetic retinopathy
The non-proliferative stage is the mildest. An increase in blood glucose levels causes a violation of the integrity of the vascular walls. Biological fluid enters the intercellular space. The risk of developing this pathological condition increases with arterial hypertension, excess cholesterol, improper functioning of the kidneys, etc. During the examination, the doctor may detect the following ophthalmological signs that accompany the non-proliferative stage of retinopathy:
- slight dilatation of the arteries and their protrusion;
- hemorrhages in the central region of the retina;
- yellowish lesions, or hard exudates, near the vascular walls;
- soft exudates, or white lesions, which represent localized areas of infarction.
Nonproliferative diabetic retinopathy is accompanied by a slight decrease in vision. Sometimes this symptom is absent or unnoticeable to the patient. This complicates timely diagnosis. If this stage has been identified, the ophthalmologist recommends:
- come for examination once every six months;
- monitor blood pressure indicators;
- monitor blood sugar levels and follow a diet;
- See a doctor even if your vision decreases slightly.
Often, diabetic retinopathy indicates poor or no control of blood glucose levels and a violation of the rules that any diabetic should follow. In other words, he eats improperly, smokes, drinks alcohol, etc. Along with ophthalmopathology, other microvascular disorders may develop.
Preventing blindness in diabetes
Most patients with a disease duration of more than 10 years have some signs of eye damage due to diabetes mellitus. Careful monitoring of blood glucose levels, following an appropriate diet and maintaining a healthy lifestyle can reduce, but do not eliminate, the risk of blindness from eye complications of diabetes.
Risk factors for developing diabetic retinopathy:
- duration of diabetes
- uncompensated diabetes mellitus (poor glycemic control),
- pregnancy,
- genetic predisposition.
The surest way to prevent blindness is strict adherence to the frequency of fundus examinations by an ophthalmologist.
Necessary frequency of examinations of patients with diabetes mellitus by an ophthalmologist.
| TIME OF DIABETES ONset | DATE FOR FIRST INSPECTION |
| Age up to 30 years | After 5 years |
| Age over 30 | When diagnosing |
| Pregnancy | First trimester* |
| INSPECTION RESULTS | FREQUENCY OF REPEATED INSPECTIONS |
| Lack of DR | Annually |
| Nonproliferative diabetic retinopathy | 4-6 months |
| Proliferative, preproliferative DR or diabetic macular edema | Laser treatment is prescribed, the frequency between stages of which ranges from 2-3 weeks to 4-6 months. |
Laser treatment is prescribed, the frequency between stages of which ranges from 2-3 weeks to 4-6 months.
* - during pregnancy, repeated examinations are carried out every trimester, even if there are no changes in the fundus of the eye.
If there is an unexpected decrease in visual acuity or the appearance of any other vision complaints in diabetic patients, an examination should be carried out immediately, regardless of the timing of the next visit to the ophthalmologist.
Only a specialist can determine the degree of diabetic damage to the organ of vision.
You will undergo all the necessary examinations using modern high-precision equipment.
Preproliferative diabetic retinopathy
This is the second, more critical stage of this disease. At the time of its progression, deformation of small vessels is observed. They become more tortuous, bifurcate, and arterial loops appear. Under an ophthalmoscope, the doctor can see a lot of exudates in the fundus, both soft and hard. Ophthalmological symptoms are already more pronounced. The preproliferative stage of retinopathy is accompanied by the following changes in vision and eye condition:
- the image is unclear, the outlines of figures are blurred;
- yellowish tint of the tunica albuginea;
- decreased central visual acuity;
- the appearance of glare, clouding;
- the appearance of small blood webs on the sclera.
If treatment is not started at this stage, the disease will continue to progress. There is a high probability of its transition to the third stage. Let's find out how proliferative diabetic retinopathy manifests itself.
Proliferative retinopathy in diabetes mellitus
With diabetic retinopathy, the blood supply to the inner lining is disrupted. This leads to the formation of abnormal vascular channels in it. This pathological process is called neovascularization; it is a protective reaction of the body. Thus, it relieves the retina from oxygen starvation.
Newly formed vessels are very fragile. They are often damaged, which leads to numerous hemorrhages in the vitreous area. Scars appear that “pull” the retina from its place, causing its detachment.
There may be other consequences. The growth of new vessels in the iris causes rubeous glaucoma, which manifests itself in increased intraocular pressure. In this case, the pupil acquires a slight greenish tint. Aqueous humor stagnates in the eyeball. Because of this, the vitreous hardens. This process leads to nerve atrophy.
The proliferative stage of diabetic retinopathy is characterized by severe symptoms. It is no longer possible to ignore or not notice its signs. These symptoms include:
- short-term complete loss of vision (sometimes long-term);
- blurred image, which becomes more obvious when blood sugar rises;
- “floaters” in the eyes;
- visible objects seem smaller than they really are;
- color perception is impaired;
- the eyes get tired very quickly, pain appears;
- With increased visual load, flashes and “lightning” flash.
Diabetic retinopathy of both eyes is an even more severe pathological process. It is characterized by a large number of newly formed vessels. There is a risk of complete loss of vision. In such cases, 80% of patients become blind.
Diabetic retinopathy can be complicated by diabetic cataracts. However, it is more common in children and young people than in the elderly. It is also more often diagnosed in women. The disease is always bilateral. At the same time, diabetic cataracts progress in both eyes quite quickly. It develops within 2-3 months, and in a diabetic crisis - within a few hours.
During biomicroscopy, whitish opacities are detected in the surface layers of the lens, which resemble flakes. Opacities in the posterior capsule are also visible. But this form of cataract differs from age-related in the nature of its course. It can be cured without removing the transparent body.
Stages of the disease
Retinopathy is a collective concept that unites various diseases of the retina of a non-inflammatory nature (primary retinopathy) and its damage in certain diseases of other organs and systems (secondary retinopathy).
Primary R. includes idiopathic central serous R., acute posterior multifocal pigment epitheliopathy, external exudative R., the etiology of which is not clear.
Secondary R. include hypertensive and diabetic R. retinopathy in diseases of the blood system, Purtscher’s traumatic retinopathy, Berlin opacities (contusional edema of the retina), etc.
- Primary retinopathy.
- Secondary retinopathy.
- The third (proliferative) stage of diabetic R. is characterized by neovascularization and the formation of so-called glial tissue. Most often, gliosis is detected in the area of the optic nerve head or main vascular trunks.
Idiopathic central serous retinopathy (idiopathic macular detachment, preretinal edema, central angiospastic R., central serous choriopathy, central serous retinitis) usually occurs in somatically healthy people 20-40 years old (more often men), who have a history of emotional stress and paroxysmal migraine type headaches.
The process in most cases is one-sided. Symptoms consist of metamorphopsia in the form of micropsia of a positive scotoma (Scotoma) and decreased visual acuity (Visual acuity). Visual acuity is typically improved when corrected with weak positive lenses, which is important for early diagnosis of the disease.
The leading sign is serous detachment of the pigment epithelium in the macular zone, ophthalmoscopically determined as a limited round or oval protrusion of a darker shade than the surrounding retina.
The foveal reflex (a strip of light around the central fovea of the retina) is usually absent. In some cases, grayish or yellowish precipitates may be visible on the posterior surface of the retina. Treatment is laser coagulation.
Drugs that strengthen the vascular wall (for example, calcium dobesilate), improve microcirculation (solcoseryl), diuretics to reduce retinal edema, and hyperbaric oxygenation (hyperbaric oxygenation) are also prescribed.
The prognosis with timely treatment is favorable. In 80% of patients after 1-4 months. From the onset of the disease, serous retinal detachment may disappear, and visual acuity is restored to its original level.
Acute posterior multifocal pigment epitheliopathy is characterized by the appearance of multiple flat subretinal foci of grayish or white color. The defeat can be one- or two-sided.
Impairment of central vision develops rapidly with the appearance of central or paracentral scotomas in the field of vision. The reverse development of lesions, which is observed in the period from several days to several weeks from the onset of the disease, is accompanied by the formation of multiple areas of depigmentation and accumulation of cement.
In half of the cases, vitreous opacification is observed. Perivascular couplings appear in the peripheral vessels of the retina, a slight expansion and tortuosity of its veins, and swelling of the optic nerve head. A number of patients develop episcleritis (see Scleritis), Iridocyclitis.
Treatment includes the use of vitamins and vasodilators (pentoxifylline, Cavinton, etc.), drugs that increase tissue oxygenation (solcoseryl), corticosteroids in the form of retrobulbar injections, and hyperbaric oxygenation. The prognosis for timely treatment is favorable.
External exudative retinopathy (Coats syndrome, Coats disease, external exudative retinitis) is observed in young people, predominantly males. The lesion is usually unilateral.
It is characterized by the formation of white or yellowish exudate under the retinal vessels, deposition of cholesterol crystals, and hemorrhages. The changes occupy the peripheral parts of the fundus of the eye; the macular zone is rarely affected.
In many cases, multiple vascular anomalies are detected in the form of micro- and macroaneurysms, arteriovenous shunts, which is clearly visible with fluorescein angiography. The course of the disease is slow and chronic. Treatment includes laser photocoagulation and hyperbaric oxygen therapy.
The prognosis is serious. Retinal detachment is often observed, requiring surgical intervention; in some cases, Glaucoma and iridocyclitis develop.
Hypertensive retinopathy occurs in hypertension, kidney disease, and toxicosis of pregnancy.
The main thing in the ophthalmoscopic picture is a change in the retinal vessels in the form of an increase or decrease in their caliber, partial or complete obliteration, etc.
Arteriolosclerosis often accompanies hypertension and is characterized by straightening and narrowing of the retinal arterioles. The arterioles around the central fossa are thin, the corresponding venules are tortuous and dilated.
Due to a decrease in the transparency of the vascular wall and pallor of the arterioles, which is observed with hypertension in adolescence, the vascular reflex acquires a yellow tint (the so-called copper wire symptom).
With significant compaction of the vascular walls and narrowing of the lumen of small vessels, they take on the appearance of a silvery thread (the so-called silver wire symptom).
A characteristic ophthalmoscopic sign of hypertensive R. is the Salus-Hun symptom, or decussation (narrowing and displacement of the vein into the deeper layers of the retina as a result of pressure on it from a compacted and tense artery at the site of their decussion) of varying degrees of severity - I, II, III.
Vascular changes in the retina also manifest themselves in the form of microaneurysms, transudation and exudation. The origin of solid exudate, which is white or grayish foci, most often located in the central zone of the retina and not contrasted with fluorescein angiography, is associated with exit through the vascular wall as a result of an increase in its permeability of blood lipids.
Soft exudate in the form of white, round, cotton-like foci is caused by occlusion of the arteriole, which suggests that it is a retinal infarction.
In the malignant variant of hypertension, in arterial hypertension caused by kidney pathology, thrombotic occlusion of small vessels causes the development of soft exudate, forming a star figure in the macular zone.
Important
The latter, however, is not a pathognomonic symptom and is also found in infectious diseases (measles, influenza, erysipelas, etc.), helminthiases, and intoxications. In some cases, subretinal exudation is so massive that it leads to retinal detachment.
The progression of hypertensive R. is accompanied by hemorrhages in the retina, which, depending on the depth of location, can be striped or rounded, as well as swelling of the optic nerve head. Treatment is aimed primarily at the underlying disease.
Vasodilators, vitamins, anticoagulants are also used, laser coagulation and hyperbaric oxygenation are used. The prognosis is serious: retinopathy can lead to a significant decrease in vision, including blindness.
In addition, the development of R., in turn, is a poor prognostic sign for the underlying disease, and during pregnancy - for both the fetus and the mother. When a pregnant woman develops R., it may be necessary to terminate the pregnancy.
Diabetic retinopathy develops in approximately half of patients with diabetes mellitus, more often with long-term diabetes. There are three stages in the development of diabetic R.. The ophthalmological picture in the first two stages is the same as with hypertensive retinopathy.
In the first stage, dilation of the veins of the first to third order and the appearance of microaneurysms are noted. The expansion of the area of the non-vascular zone may indicate the beginning of the process of obliteration of the perifoveal capillaries.
In the second stage, pockets of hard and soft exudate appear. Edema of the macular area is characteristic, sometimes significant (the thickness of the retina in the area of edema can increase 4-5 times).
The prolonged existence of edema leads to the formation of micro- or macrocystic dystrophy, accompanied by a persistent decrease in visual acuity.
In some cases, single or multiple hemorrhages in the retina, segmentally dilated veins, emptying of blood vessels, retinal edema around the vessels in the form of couplings, as well as areas of focal ischemia are noted.
Sometimes glial tissue in the macular zone forms a kind of canopy along the posterior surface of the vitreous, causing a significant decrease in visual acuity with relative preservation of the retina.
The process ends with scarring and displacement of the vitreous, which can lead to tension and retinal detachment. Treatment is primarily aimed at the underlying disease. Laser coagulation is also used, vascular protective drugs are prescribed (calcium dobesylate, etamsylate), vitamins, agents that improve microcirculation, etc.
The prognosis is serious. Diabetic R. in 16-18% (and in the third stage in 50%) of cases ends in blindness. In addition, it is an unfavorable prognostic sign for the underlying disease. Retinopathy in diseases of the blood system develops with polycythemia, anemia, leukemia, and Waldenström's disease.
In polycythemia, the retinal veins may have an unusual dark red color, giving the fundus a cyanotic hue. Sometimes venous thrombosis and papilledema occur due to circulatory failure in the internal carotid, vertebral or basilar arteries.
With anemia, the fundus reflex due to a decrease in the hemoglobin content in red blood cells becomes paler, the arteries and veins of the retina dilate and sometimes their caliber and color become the same.
With severe anemia, pale hemorrhages appear located in the layer of nerve fibers (their extent depends on the degree of anemia), as well as deep hemorrhages of various shapes and sizes, with white areas in the center - Roth spots, caused by damage to the deep capillaries of the retina.
Anemia is accompanied by the development of extraretinal hemorrhages, which are located in the choroid of the eye in the form of a brownish disc, slightly lifting the retina, or are localized between the retina and the vitreous body and can lead to partial or complete hemophthalmos.
Retinal exudate may be hard or soft. A rare complication is exudative retinal detachment. In myeloid leukemia, the retinal veins become tortuous, and generalized retinal edema and papilledema may appear.
Various types of hemorrhages occur, incl. and subretinal. Exudate can be of various types, but most often in the form of small white dots scattered in the central zone of the fundus.
In Waldenström's disease and myeloma, changes in the retina are associated with dysproteinemia, paraproteinemia, increased blood viscosity and are characterized by dilation of the retinal veins, an increase in their tortuosity, and, to a lesser extent, dilation of the arteries.
The Salus-Hun symptom, microaneurysms, occlusion of small veins, and retinal hemorrhages appear. In some cases, cotton wool-like lesions appear in the layer of nerve fibers of the retina, and swelling occurs in the area of the optic nerve head.
In the azotemic stage of the disease, R. develops, characteristic of chronic kidney diseases. Treatment is aimed at the underlying disease. Vitamins, drugs that increase tissue oxygenation, laser coagulation, and anticoagulants for polycythemia are also indicated.
The prognosis for restoration of visual function is serious. Purtscher's traumatic retinopathy develops with sudden compression of the chest, at the moment of which, as a result of arteriolospasm, hypoxia of the retina occurs and the release of transudate from the blood into it.
1-2 days after the injury, hemorrhages and milky-white, sometimes silver-white spots appear in the retina around the optic nerve head. R. may be complicated by optic nerve atrophy.
Treatment is carried out with vitamins, vasodilators, drugs that reduce tissue hypoxia, and hyperbaric oxygenation is used. The prognosis is serious: organic changes in the retina can lead to decreased vision.
Berlin's retinal opacities are peculiar changes in the retina that develop with contusion of the eyeball.
Important
According to the German ophthalmologist R. Berlin, who described this R., retinal opacities are based on subchoroidal hemorrhage and swelling of the deep layers of the retina; according to other researchers, opacities are associated mainly with the appearance of transudate between the choroid and the retina.
The ophthalmoscopic picture is characterized by the presence of whitish opacification along the periphery of the retina on the side of the contusion; sometimes the same opacification appears on the opposite side of the retina, less pronounced in the macular zone.
Treatment includes the use of vitamins, drugs that reduce tissue hypoxia, and hyperbaric oxygenation. The prognosis is favorable.
Retinopathy in diabetes mellitus: diagnosis
It is worth noting that with this disease, the patient must visit an ophthalmologist every six months in order to detect complications in time and begin their treatment. To confirm retinopathy, you need to undergo several procedures:
- perimetry, which evaluates visual fields;
- electrophysiological study to determine the viability of nerve cells of the inner membrane and optic nerve;
- tonometry - a procedure for measuring intraocular pressure, which can increase already at the stage of preproliferative retinopathy;
- ophthalmoscopy - examination of the fundus of the eye, which displays all pathological changes, new vessels, exudates and microhemorrhages are visible.
Ultrasound, OCT, diaphanoscopy and other diagnostic methods may be prescribed. This depends on the degree of the disease and the presence of concomitant pathologies. For diabetes mellitus, the main therapeutic treatment is carried out by an endocrinologist.
Definition and classification
Retinopathy refers to pathological changes in the structure and functioning of the retinal vessels of the inner lining of the eye (retina) of a non-inflammatory nature. The pathology is a consequence of impaired blood supply to the vascular network due to a number of unfavorable factors of various origins. Eye retinopathy is dangerous due to severe irreversible processes leading to optic nerve atrophy and complete blindness.
Based on the underlying causes, the disease is divided into 3 categories:
- primary, not associated with inflammation;
- secondary (background), which is a consequence of the existing systemic pathology of other organs;
- retinopathy of prematurity.
Diabetic retinopathy: treatment
This pathology is secondary, so treatment is aimed primarily at combating diabetes. It is necessary to prevent hyperglycemia, which is achieved through medications and diet. With progressive diabetic retinopathy, laser coagulation of the retina is performed, with the help of which it is possible to suppress neovascularization, that is, the growth of new vessels. This helps prevent retinal detachment.
There are several techniques used today in ophthalmology for laser coagulation. The essence of any of them comes down to the following:
- destruction of the area of hypoxia of the inner membrane and cornea, which causes the formation of new vessels;
- normalization of the supply of a full volume of oxygen to the retina from the choroid;
- elimination of newly formed vascular networks.
For non-proliferative diabetic retinopathy, which is accompanied by macular edema, barrier laser coagulation is prescribed. During this procedure, paramacular coagulants are applied to the retina in several rows, which form a lattice. This multilayer mesh prevents the appearance of new pathological vessels. In the presence of microaneurysms, small hemorrhages, and various types of exudates, focal laser coagulation is performed. The preproliferative stage is treated with panretinal laser coagulation. During this procedure, coagulants are applied to the entire retina, except the macula.
Laser coagulation is a safe and low-traumatic operation, but at the same time very effective, especially in the non-proliferative and preproliferative stages of the disease. The procedure is performed under local anesthesia on an outpatient basis. There is no need to prepare for it. Coagulation is carried out using a special device and a targeted laser beam, which cauterizes pathological vessels. Along the way, pathways for alternative oxygen supply to the retina are formed. This operation lasts no more than half an hour. During it, the patient does not feel pain or other discomfort. No hospitalization required. But the effectiveness of the procedure is limited to two stages of diabetic retinopathy. In case of severe eye damage, a surgical operation is performed - vitrectomy.
This procedure is based on removing the vitreous (or part of it) and replacing it with a polymer, saline solution or other substance. The operation is performed in a hospital. Before it, you should not eat or drink water for about 12 hours. Vitrectomy lasts approximately 2 hours under general anesthesia or local anesthesia, depending on the patient’s condition. The surgeon makes an incision in the cornea, penetrates the inner parts of the eyeball and removes the vitreous humor. Instead, another substance is injected, which subsequently dissolves, and the eye is again filled with intraocular fluid. After the operation, the patient is prohibited for 2 weeks from:
- reading a lot and sitting at the computer tires your eyes;
- play sports, lift weights;
- go to the pool, bathhouse, sauna.
The operation can cause complications: retinal detachments, progression of cataracts, corneal opacification, endophthalmitis. But they are detected extremely rarely. In principle, vitrectomy is a safe treatment option for treating severe diabetic retinopathy.
Diagnosis of diabetic lesions of the organ of vision
Diagnosis of diabetic retinopathy should be carried out using modern high-precision equipment and include the following studies:
- determination of visual acuity, which allows you to determine the condition of the central region of the retina,
- visual field examination (computer perimetry) to determine the condition of the retina in the periphery,
- examination of the anterior segment of the eyeball (biomicroscopy), which allows you to determine the condition of the iris and lens,
- examination of the anterior chamber angle (gonioscopy),
- visual field examination (computer perimetry),
- measurement of intraocular pressure (tonometry).
If the level of intraocular pressure allows, then further studies are carried out with a medically dilated pupil.
- biomicroscopy of the lens and vitreous body,
- electrophysiological research methods to determine the functional state of the optic nerve and retina,
- Ultrasound examination (scanning) of the organ of vision to determine the condition of the vitreous body. This study is especially important in the presence of opacities in optical media, in which fundus ophthalmoscopy is difficult.
- examination of the fundus (ophthalmobiomicroscopy), which allows us to identify the condition of the retina and its relationship with the vitreous body, determine qualitative changes in the retina and their localization. Ophthalmic biomicroscopy should be carried out with mandatory registration and photographing of the data obtained, which makes it possible to obtain documentary information about the condition of the fundus, the degree of retinopathy and reliable results of the effectiveness of the prescribed treatment.
The study reveals changes in the retina that indicate the presence of retinopathy with a risk of progressive damage and blindness, indicating the likelihood of an unfavorable outcome over the next year.
The results of these studies will allow our specialist to recommend the treatment you need to prevent vision loss.
Nutrition for diabetic retinopathy
The disease will recur and progress if the patient does not follow the diet. It is the basis of therapy for diabetes of any type. First of all, the patient will have to give up sweets, salt and alcohol. You should also avoid other foods that can cause an increase in blood pressure or blood sugar.
It is recommended to quit smoking. You need to consume vitamins A, B, C, E, PP. The body should also receive selenium, chromium, copper, folic acid, etc. You need to control your weight. With obesity, the risk of developing complications greatly increases. In addition, it is recommended to be examined more often. In no case should you ignore ophthalmological symptoms or try to cure retinopathy with folk remedies.