How does diabetes affect vision?
Diabetes mellitus is a metabolic disorder characterized by elevated blood sugar levels. The main cause of this disease is insufficient production of insulin in the body, a hormone that maintains glucose concentration and regulates carbohydrate metabolism. This pathology is quite severe, it leads to the development of various complications. Diabetes mellitus also affects vision. An increase in blood sugar levels leads to deterioration of blood vessels. The tissues of the eyeballs do not receive enough oxygen. In other words, eyes with diabetes constantly suffer from lack of nutrition, especially if there is no proper treatment. This causes decreased vision. Most often, diabetics develop diabetic retinopathy - 70-80% of patients. Another 20-30% accounts for the following ophthalmopathologies:
- diabetic cataract;
- diabetic glaucoma;
- dry eye syndrome.
According to official statistics, from 5 to 20% of diabetics go blind in the first 5 years after their diabetes is diagnosed. However, according to doctors, in reality the problem is larger. Many patients do not treat diabetes, the pathology develops, and the deterioration of vision is associated with age-related changes in the body and other factors.
Let's take a closer look at the listed ophthalmopathologies. When should a patient be alert? Let's find out whether it is possible to prevent vision deterioration in diabetes.
Factors in the development of diabetic retinopathy.
The duration of diabetes is the most significant risk factor. Diabetic retinopathy rarely develops in the first 5 years of the disease or before puberty, but in 5% of patients with type 2 diabetes, diabetic retinopathy is detected at the same time diabetes is diagnosed.
High sugar levels are no less a significant risk factor than the duration of the disease. It is known that good blood sugar management can prevent or slow the development of diabetic retinopathy.
Diabetic
(nephropathy) causes worsening of diabetic retnopathy.
Other risk factors include excess weight, hyperlipidemia and anemia.
How diabetes affects vision - diabetic retinopathy
A prerequisite for the development of retinopathy is hyperglycemia - an increased concentration of sugar in the blood.
In this condition, thinning of the capillaries and the formation of microthrombi occur. Various abnormalities appear in the fundus. The retinal tissue suffers from a lack of oxygen. There are three forms/stages of diabetic retinopathy:
- Non-proliferative. Aneurysms form in the retina, hemorrhages occur, edema and foci of exudation occur. This form of pathology is also characterized by macular edema. The danger of the early stage is that vision does not deteriorate, but pathological processes may be irreversible.
- Preproliferative. Microvascular abnormalities are observed. Frequent retinal hemorrhages occur.
- Proliferative. Proliferation is a pathological growth of tissue. At this stage of the disease, most of the vessels are replaced by overgrown ones. Multiple retinal hemorrhages are observed. Vision begins to deteriorate. Usually its sharpness drops rapidly. If the disease is not stopped at this stage, the patient will go blind. Retinal detachment is possible due to the fact that there is a lot of overgrown connective tissue in the fragile vessels.
As already noted, at the initial stage, retinopathy is not accompanied by visual impairment. Sometimes a person does not notice alarming symptoms for a long time even in the second stage, because they rarely bother. Subsequently, signs of the disease appear such as:
- blurred vision;
- flickering “flies”, floating dark spots;
- a veil covering the eyes;
- reduced visibility at close range.
The effect of diabetes on vision
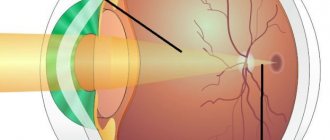
The main symptom of diabetes is increased blood glucose levels (hyperglycemia). In this regard, the inner layer of small vessels of the retina is affected, and the functioning and interaction of the cells of the retina of the eye is disrupted. The structure of the proteins of blood cells is disrupted, which leads to increased platelet aggregation and decreased elasticity of red blood cells.
Also, diabetes mellitus is often accompanied by increased blood pressure, which negatively affects the regulation of vascular tone.
As a result of numerous negative processes caused by hyperglycemia and metabolic disorders, a violation of microcirculation of the fundus develops. There is an expansion and blockage of blood vessels, an increase in vascular permeability. This leads to disruption of oxygen circulation and nutrition of the retina. These processes are included in the concept of the non-proliferative stage of diabetic retinopathy.
Next, a more severe proliferative stage develops. It is characterized by the appearance and growth of new, pathologically organized blood vessels. In this way, the body tries to compensate for insufficient oxygen metabolism. However, new vessels do not have a full structure and grow on top of the retina, where they cannot realize their beneficial properties and only interfere with vision.
Diabetic cataract
Cataracts cause clouding of the lens. It becomes impenetrable to light rays. Vision with this pathology deteriorates very much. Cataracts are one of the causes of blindness in many older people. Diabetes mellitus can also provoke this disease. With constant hyperglycemia, which leads to metabolic disorders, glucose compounds accumulate in the lens of the eye. They cause it to darken and thicken.
How does cataract develop in diabetes mellitus? It usually develops faster with this disease than due to other reasons. The pathology progresses as follows:
- At the first stage, vision does not change. The patient experiences virtually no symptoms. Often, it is possible to detect cloudiness at this stage only during a preventive or routine examination.
- In the second stage, immature cataracts are observed. The first vision problems appear. Its severity may decrease.
- In the third stage, the lens becomes almost completely cloudy. It turns milky grey. Of all visual functions, at this stage color perception is preserved, but impaired.
- At the fourth stage, the fibers of the transparent body disintegrate. Complete blindness occurs.
The intensity of symptoms depends on the type of diabetes. Typically, diabetics with types 1 and 2 of the disease notice the following signs:
- a veil before the eyes;
- impaired color vision - colors become dull;
- diplopia - double image;
- sparkles in the eyes.
In the later stages, there is a strong decrease in visual acuity. Any visual load leads to rapid fatigue. It is impossible to read or work on a computer. Gradually, the patient ceases to distinguish between objects and images.
Cataract
The possibility of lens clouding increases with the duration of diabetes. A cataract goes through several stages of “maturation”, during which the lens thickens and increases in size: initial, immature, mature and overripe (mammary).
The causes of cataracts in diabetes mellitus are increased sugar levels in the blood and chambers of the eye, impaired blood supply and nutrition to the lens, damage to nerve fibers due to endocrine disorders
True diabetic cataract is more typical for the younger age group with juvenile uncompensated diabetes. It develops rapidly, over a few days, and affects both eyes at once. If you identify this process in time, then by normalizing carbohydrate metabolism, you can reverse the process. If this is not done, then further maturation of the cataract occurs and the lens becomes uniformly clouded. Myopia develops. Dystrophic processes and microcirculation disorders occur in the iris.
Diabetic glaucoma
Glaucoma is a group of ophthalmological diseases in which there is an increase in intraocular pressure. It is often diagnosed in old age. Diabetes mellitus can also be the cause of its development. An increase in blood sugar levels leads to a deterioration in the condition of blood vessels and their proliferation. New capillaries block the outflow of intraocular fluid, causing an increase in ophthalmotonus - pressure in the eyeball. Glaucoma can occur in different forms. Depending on the stage of the disease and other factors, it is accompanied by:
- increased photosensitivity;
- profuse lacrimation;
- flashing “flashes” and “lightning” before the eyes;
- pain in the eyeballs;
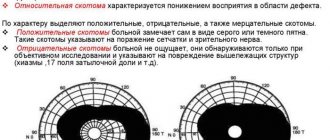
- narrowing of visual fields;
- the appearance of rainbow circles before the eyes.
Increased intraocular pressure can lead to damage to the optic nerve with subsequent atrophy of its tissue. In such cases, visual functions are lost forever. Glaucoma, like other complications of diabetes (retinopathy and cataracts) can lead to irreversible blindness.
Diabetic retinopathy and types
An ophthalmic disease affects the small blood vessels of the eye. Arterioles, veins, and capillaries undergo degeneration. This is a common complication of diabetes and can lead to complete blindness in the patient. The disease is diagnosed in 90% of patients with hyperglycemia.
The main cause of visual impairment is impaired microcirculation. Unwanted substances enter the retina, causing the formation of shunts, microaneurysms and hemorrhages. Patients complain of pain and decreased visual acuity,
According to the WHO classification, diabetic retinopathy is divided into the following types:
- Retinopathy I, non-proliferative. Microaneurysms and hemorrhages are found in the membrane of the eye. They can be identified by small round dots or spots. Retinal edema is noted.
- Retinopathy II, preproliferative. The optometrist detects venous abnormalities, including loops, tortuosities, caliber fluctuations, and duplications. Dense discharge and signs of hemorrhage appear.
- Retinopathy III, proliferative. The optic nerve and retina are affected. After hemorrhages, fibrous tissue forms, leading to retinal detachment. Glaucoma is common.
How to prevent eye diseases in diabetes?
So, diabetes mellitus affects vision quite strongly. At the same time, an increase in blood sugar concentration is the main cause of retinopathy, cataracts and other ophthalmic pathologies. There are also a number of predisposing factors. These include:
- genetic predisposition;
- heavy visual load, habit of reading in the dark;
- constant use of electronic devices - computers, phones, tablets;
- wearing low-quality sunglasses without UV filters or complete lack of eye protection from UV rays;
- bad habits - smoking, alcohol abuse.
In most cases, severe consequences of diabetes occur in patients who neglect treatment, do not engage in prevention, and rarely visit a doctor. When diagnosing diabetes mellitus, the predisposing factors listed above should be completely excluded. What else do ophthalmologists advise?
Firstly, diabetics need to visit an ophthalmologist at least once a year. If diabetic retinopathy or other ophthalmopathologies have already been identified, then it is recommended to check the condition of the eyes 3-4 times a year. Secondly, you need to take eye vitamins. They are also available in the form of drops.
Vision correction for diabetes
If vision in diabetes begins to steadily decline, then measures will need to be taken to correct it:
- Visit an ophthalmologist twice a year for follow-up examinations. This will allow timely detection of critical changes in the eyeball and prevent complete blindness.
- Follow all the instructions of the treating endocrinologist exactly - take medications, perform insulin injections. This will help maintain blood sugar levels within normal limits at all times, which will reduce the likelihood of rapid progression of cataracts, glaucoma and retinopathy.
- If necessary, wear corrective glasses at all times. Regarding the advisability of using contact lenses, you should consult with specialists; often diabetes mellitus becomes a contraindication to this type of visual acuity correction.
- Follow the rules of rest and wakefulness/work during the day. If the patient is forced to spend a lot of time at the computer or reading papers (specifics of work activity), then he must break away from the usual “picture” every hour, look out at the window, and blink frequently.
According to statistics, those patients with diabetes who closely monitor the condition of their visual organs and follow all the recommendations of doctors reduce the risk of complete blindness significantly.
Vitamins for eyes for diabetes
Metabolism in this disease is disrupted. Because of this, the body does not receive enough microelements and vitamins. In this regard, doctors prescribe vitamin complexes to diabetics that help strengthen blood vessels and improve eye condition. It is recommended to take daily:
- B vitamins that normalize sugar levels and improve blood circulation.
- Ascorbic acid. It strengthens the immune system and increases the elasticity of blood vessels.
- Tocopherol, vitamin E. It removes toxins and glucose breakdown products from the body.
- Retinol (vitamin A). This element improves night vision and increases its sharpness.
- Vitamin P, which improves microcirculation by dilating blood vessels.
The specific drug will be prescribed by the attending physician. He will determine the dosage.
Eye surgery for diabetes
When is eye surgery necessary for diabetes? In the initial stages, cataracts, glaucoma and retinopathy are treated with conservative methods - using eye drops and other medications. In extreme cases, operations are prescribed. Thus, for retinopathy, laser coagulation may be required. It is aimed at preventing and regressing vascular proliferation. In case of serious damage to the eye, it may be necessary to undergo vitrectomy - partial removal of the vitreous humor.
Complete clouding of the lens, which occurs with severe cataracts, is treated by removing it. The transparent body is replaced with an intraocular lens. This operation is carried out today using laser technology. Often, replacing the lens is the only way to preserve the patient's vision.
With constant increases in intraocular pressure, an operation is performed to speed up the process of outflow of intraocular fluid. It is prescribed only in cases where drug therapy does not bring results.
We list the symptoms that should alert a diabetic and make him go to an ophthalmologist:
- decreased visual acuity;
- a veil before the eyes;
- flickering “flies”, the appearance of black spots;
- constant dryness of the cornea, redness of the sclera;
- pain, itching, tingling in the eyes;
- rapid fatigue of the visual organs.
How to restore visual function to a diabetic?
The basis of vision treatment for diabetes mellitus is, first of all, timely treatment of the underlying disease and normalization of the glucose ratio.
By improving the general condition of the diabetic, it will be possible to achieve normalization of visual functions. However, the complexity of the clinical picture will have a direct impact on the selection of a specific treatment algorithm for diabetics.
In order to improve vision in type 2 diabetes at the initial stage, it is recommended to use medications and folk remedies. For example, the most popular of the latter is mumiyo. In more severe cases, restoration of visual functions can be achieved solely through surgery.
Joint pain in diabetes
For example, glaucoma is initially treated with antihypertensive drips. However, the main treatment method is surgery, which is recommended as early as possible. In this case, vision will be restored to a greater extent, complications and critical consequences will be excluded.
Vision can only be restored with cataracts through surgery. How positive the result is will be influenced by the degree of damage to the retina. For retinopathy, so-called step-by-step laser coagulation of the retina is performed. However, in cases of progressive diabetes mellitus, vitrectomy is recommended.