Sympathetic ophthalmia is a non-purulent inflammation that develops in a healthy organ of vision due to injury to the second eye or ophthalmic surgery performed on it.
The process develops and manifests itself very slowly; in some cases, the appearance of severe symptoms is preceded by a period of several weeks to several months. The main danger of the pathology is that it can lead to the loss of the inflamed eye, while the main treatment is aimed at healing the diseased paired organ.
Causes of the disease
The causes and mechanism of development of the disease are not exactly clear and are speculative. Some researchers believe that the etiology of the disease is viral. Most likely, the pathogen is uveotropic and penetrates from the initially affected eye to the healthy eye through the blood.
Other researchers, in particular I.V. Davydovsky, consider the appearance of signs of sympathetic ophthalmia to be the result of immune disorders, namely, a manifestation of autoimmune allergies.
Many experts note that dysfunction of the nervous trophism plays a significant role in the development of pathology.
Disease prevention
Due to the fact that the reason for the development of such a pathology is not entirely clear, it is quite difficult to name effective ways to prevent it. However, it is believed that damage to one eye somehow programs the body to produce an autoimmune inflammatory response to certain parts of the eye. It appears that trauma to the eye brings tissue into contact with the bloodstream, which stimulates the immune system.
This produces antibodies, which are the body's defense proteins. The body produces antibodies against antigens that are recognized as foreign proteins. Normally, the eye tissue is separated from the bloodstream, but after an eye injury, the blood mixes with the eye tissue. Antibodies are incorrectly directed against ocular tissue antigens.
It is also believed that certain microorganisms may contribute to sympathetic ophthalmology. Therefore, the most effective and productive way to prevent the development of the disease is considered to be regular visits to an ophthalmologist at least 1-2 times a year. At the same time, it is recommended to consult a doctor at the first symptoms of the disease, as well as if you begin to experience discomfort or are bothered by an unexpected decrease in vision.
Symptoms of sympathetic ophthalmia
The disease is accompanied by manifestations similar to those of iridocyclitis of the fibrinous type (with the release of fibrinous exudate).
In addition to symptoms of irritation of the organ of vision (pain, spasm of the eyelids and the inability to unclench them, lacrimation, photosensitivity), injection of the eyeball, swelling of the iris, reduction of the pupil in size, the appearance of posterior adhesions, decreased transparency of the vitreous body, and accumulation of moisture in the anterior chamber of the eye appear.
Next comes planar fusion of the iris with the anterior part of the lens, complete or partial fusion of the pupil, and the formation of anterior synechiae, which close the angle between the iris and cornea.
Gradually, the pressure inside the eye increases and glaucoma develops. Sometimes there is a persistent decrease in intraocular pressure, which threatens eye subatrophy.
If iridocyclitis is of the serous type, then the manifestations of sympathetic ophthalmia are less significant. Small gray precipitates form on the back of the cornea, and adhesions are observed less frequently. Pericorneal injection is also insignificant or absent.
In some cases, secondary glaucoma is diagnosed.
This form of the disease is generally more favorable than the one described above, but the serous type of sympathetic ophthalmia is rare in isolation.
Iridocyclitis usually progresses very slowly. Constant exacerbations of the disease alternate with long-term remissions. Sometimes the disease lasts up to several years, occasionally it debuts and progresses acutely and rapidly.
In addition to inflammation, widespread (less often locally limited) choroiditis can also appear in the vessels of the anterior part of the eye.
An early complication of sympathetic ophthalmia can be retinal detachment as a result of penetration of exudate and the formation of infiltrate in the vascular network, as well as against the background of neuroretinitis.
Possible complications
The severe consequences of lack of timely treatment may include:
- Vitreous opacification;
- Papillitis;
- Violation of the production and outflow of moisture inside the eye, in other words, glaucoma.
Glaucoma is a complication of sympathetic ophthalmia
If ophthalmia develops as uveitis, wrinkling and atrophy of the vitreous body, retinal detachment, decreased muscle tone and vision, deterioration in its quality and blindness are possible.
The disease progresses slowly and may be accompanied by periods of exacerbation and improvement. Stopping its progression and returning visual functions is possible only with properly selected therapy.
Timely initiation of treatment is necessary, since the disease can be completely cured only in the early stages of its development. In rare cases, in later stages, it is possible to remove the eyeball.
Sympathetic inflammation of the eyes
Etiology of sympathetic inflammation of the eye
. Perforated eye injury, complicated by sluggish chronic iridocyclitis, less often surgical intervention or perforated corneal ulcer. The second, healthy eye becomes ill.
The pathogenesis of sympathetic inflammation of the eye is not entirely clear. It is assumed that there is a uveotropic virus that enters the eye from the conjunctival sac at the time of a penetrating wound and then enters the second eye. In this case, importance is attached to sensitization of the second eye and disruption of nervous trophism. In recent years, the role of toxoplasmosis in the origin of sympathetic ophthalmia has been pointed out.
Symptoms of sympathetic inflammation of the eye. It develops no earlier than 12-14 days, most often 4-8 weeks after injury to the first eye. The disease can occur in the form of uveitis or neuroretinitis. More often, plastic uveitis is observed with signs of irritation of the eyeball, hyperemia of the iris, constriction of the pupil, exudate in the area of the pupil and anterior chamber, posterior synechiae, precipitates, and vitreous opacities. Intraocular pressure is usually reduced, but secondary glaucoma may develop in the future. With sympathetic neuroretinitis, inflammation is more pronounced in the posterior segment of the eyeball.
The course of sympathetic inflammation of the eye. Characterized by slow progression with periods of subsidence and exacerbation of the process. Changes in the refractive media and the retina contribute to a decline in visual function.
Recognition of sympathetic inflammation of the eye
It is not difficult if the process develops in the second eye after a penetrating wound to the first eye. The diagnosis is confirmed by histological examination of the damaged eye.
Prevention of sympathetic inflammation of the eye. Timely enucleation of the injured eye (no later than the 14th day after injury). Indications: severe eye injury, blindness, symptoms of sluggish iridocyclitis, hypotension, lack of positive dynamics of the process. Preventive measures also include timely and thorough treatment of penetrating wounds and their treatment.
Treatment of sympathetic inflammation of the eye . Local mydriatic agents in the form of drops, ointments, powder for hypotension, miotic agents for hypertension. Cortisone in a 0.5% solution once a day in the form of drops, subconjunctival injections of 0.2 ml 1-2 times a week. In the regression stage, instillation of a 3% solution of potassium iodide 3 times a day, dionin 2-3 times a day in a 1-6-10% solution. Leeches on the temple. General treatment is antibiotics intramuscularly and orally (penicillin 150,000-200,000 units 2-4 times a day, for a course of 6,000,000-7,000,000 units; streptomycin 250,000-500,000 units 1-2 times a day, for course 5,000,000-8,000,000 units, tetracycline 100,000-200,000 units with nystatin 0.1 g 4 times a day for 5-10 days orally, chloramphenicol up to 4 g per day for adults, monomycin, erythromycin) . Prednisolone according to the scheme: 5 days, take 1 tablet 4 times a day, 5 days, 1 tablet 3 times a day, 5 days, 1 tablet 2 times, then 5 days, 1 tablet 1 time a day. While taking prednisolone, a salt-free diet with an increase in the amount of protein is recommended, and potassium acetate in solution is taken orally. For 3-4 days before stopping prednisolone, as well as 3-4 days after stopping the drug, ACTH is sometimes prescribed intramuscularly at 10-60 units 2 times a day, for a course of 300-1200 units. Sulfonamide drugs, butadione in the acute period, osmotherapy, and rubbing in gray mercury ointment are indicated.
The prognosis of sympathetic inflammation of the eye depends on the timeliness of treatment. Currently, the use of antibiotics, sulfa drugs, and corticosteroids has significantly improved the prognosis. The prognosis for neuroretinitis and serous uveitis should be considered more favorable.
Symptoms
Sympathetic ophthalmia is manifested by the following patient complaints:
- lacrimation;
- photophobia;
- redness of the eye;
- a drop in visual acuity, first at close range, then at distance;
- violation of color identification.
Deformation of the vessels of the iris indicates a disease.
Signs of this disease upon examination are fogging of the endothelium, dilatation of the vessels of the iris, a decrease in the speed of constriction of the pupil to light, and damage to the optic nerve head. In this case, clouding of the vitreous body and a decrease in the level of dark adaptation can be detected. There are specific symptoms of this disease - drops of “mutton fat” - large deposits on the surface of the cornea and Dahlen-Fuchs nodules - thickenings on the retina.
Specific signs help the doctor during examination to suspect sympathetic ophthalmia.
Treatment and prognosis
Therapy boils down to the use of drugs to dilate the pupil of the eye (for example, atropine sulfate), as well as glucocorticosteroids. If treatment is started at the initial stage of the disease, then inflammation is effectively reduced, and in some cases the pathology recedes.
Glucocorticosteroids are prescribed in the form of retrobulbar injections or installations), as well as intramuscularly. In severe cases, cytostatics are required to suppress the process.
In case of bacterial infection of the eye, a course of antibacterial agents is recommended.
Additionally, the treatment program includes absorbable drugs and other means and methods. The prognosis is serious: blindness among patients reaches 40-80%.
Treatment
The risk of developing sympathetic ophthalmia during injuries or operations on a paired organ is consistently high, but inflammation of this kind is not always a consequence of injury. In any case, the detection of any of these symptoms requires immediate consultation with a specialist and examination, since only timely consultation with a doctor and treatment can preserve the visual ability of the eye.
Radical treatment methods include removal of the eyeball in case of blindness in the injured eye, which helps prevent the spread of the inflammatory process to the healthy organ of vision. An operation of this kind is carried out no later than 14 days from the moment of injury. But more often, ophthalmologists resort to drug therapy, trying to preserve the blind eye.
Preventive examinations must be performed every 6 months
To restore and maintain visual acuity, the following is prescribed:
- corticosteroid hormones;
- antibacterial, anti-inflammatory, antiallergic medications (can also be recommended if removal surgery has been performed);
- cytostatics.
The features and need for combined or non-traditional treatment are discussed with the doctor.
Read here how retrobulbar optic neuritis develops and what it can lead to.
Antibiotics, cytostatics and hormonal drugs are used in treatment
A vitamin that allows you to restore vision after various ophthalmological problems is vitamin eye drops with riboflavin.
conclusions
Sympathetic ophthalmia is one of the diseases of the organs of vision that are most dangerous for humans. In case of serious complications, complete loss of vision is possible, and in rare cases, removal of the eyeball may be indicated. However, timely treatment (especially in the early stages of development) can eliminate the problem and restore all the basic functions of the visual system. Therefore, it is necessary to start it as early as possible and, when the first symptoms are detected, seek qualified help.
Prevention and prognosis
Considering the penetrating nature of eye injuries, in which sympathetic ophthalmia develops, such a diagnosis is rare in ophthalmological practice. However, according to statistics, up to 80% of cases of diagnosing a disease, it ends unfavorably for the patient, i.e. complete blindness.
At the same time, the probable causes of the spread of inflammation also include other factors not related to injuries, so it is almost impossible to prevent the pathology. Experts in this field advise adhering to basic preventive measures aimed at preventing the disease:
- compliance with personal safety rules to avoid eye injuries;
- systematic examination by an ophthalmologist;
- compliance with all recommendations for the treatment of diseases of the organs of vision, incl. infectious and other nature;
- seek medical help if any problems with the visual system are identified;
- compliance with eye hygiene rules;
- refusal of self-medication.
Diagnosis of pathology takes into account the patient’s complaints, and includes a visual examination and medical examination of the cornea, lens and tissues around the site of inflammation.
When white light is not nice or establish the true causes of photophobia of the eyes.
Diagnostics
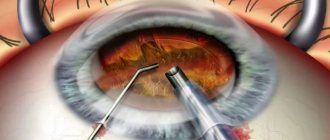
Investigation and diagnosis of problems usually includes the following measures:
- Visual inspection of the affected areas;
- Ophthalmoscopy (helps identify other possible disorders of the visual apparatus);
- Biomicroscopy (promotes examination of the cornea and lens of the eye);
- Histomorphological examination (allows you to examine tissue and detect other possible inflammatory processes in the organs of vision).
Carrying out ophthalmoscopy
Often important additional information is provided by interviewing the patient. Only after carrying out all of the above procedures can the doctor correctly make a diagnosis, determine the stage of progression and prescribe the correct treatment.
Accurate information is very important for a correct diagnosis. Therefore, during the interview, it is necessary to describe the situation as truthfully as possible and answer the ophthalmologist’s questions.
Types and classifications
Sympathetic ophthalmia has the following forms of development:
- Serous. Characterized by the occurrence of serous iridocyclitis. Most often, therapy in this case gives a good prognosis and the progression of the disease stops. Occurs with average frequency.
- Neuritic. It is diagnosed quite rarely and is an independent pathology. The onset of progression is often imperceptible and asymptomatic; after some time, mild neuritis appears. Dullness and swelling of the tissues and redness occur. It is usually cured with complete restoration of visual functions only in half of the cases.
- Mixed. It occurs more frequently than those listed and combines the characteristics of both forms. In most cases of therapy, the prognosis is favorable and most often ends in complete recovery of the patient.
Serous form of sympathetic ophthalmia
Forms of manifestation
The serous type of the disease is treatable with medication.
The following types of this disease are distinguished:
- Serous form - manifests itself as serous iridocyclitis. This manifestation of ophthalmia has the mildest course and is subject to conservative treatment.
- Neuritic - accompanied by a sharp manifestation of neuritis. With this form, damage to the optic nerve head, retinal hyperemia, and dilatation of the arteries and veins of the eye occur.
- Mixed - occurs most often and leads to an unfavorable outcome - blindness. At the same time, papilledema and significant exudation of serous contents develop.
Symptoms
Sympathetic ophthalmia may not appear for a long time or appear suddenly with acute symptoms. Signs:
- small specks called floaters;
- blurred vision;
- decreased vision;
- increased lacrimation;
- formation of precipitates in the area of a healthy organ of vision;
- photosensitivity (photophobia);
- redness of the mucous membrane;
- some patients experience pain.
There are periods when symptoms improve and then worsen. Sympathetic ophthalmia can be a chronic disease.
In rare cases, the disease is accompanied by hearing loss, headaches and dizziness, and vitiligo.