general description
Central retinal artery occlusion (ICD 10 - H34.1) is a disease caused by a sudden cessation of blood circulation in the central retinal artery or its branches.
Among the main causes of this pathology are spastic narrowing or inflammation of the artery walls, as well as embolism and thrombosis. In elderly and senile people, risk factors are atherosclerotic changes in blood vessels and arterial hypertension. In young people, risk factors are pathological conditions associated with dysfunction and/or anatomical integrity of the valvular structures of the heart, as well as cardiac arrhythmias.
Symptoms of retinal hemorrhage
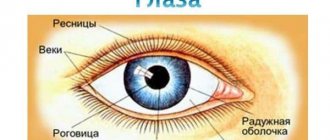
As the pathological process develops, the presence of blood in the eye may be almost unnoticeable, but since the retina contains visual receptors, the condition of hemorrhage is very dangerous.
General signs of illness:
- Flickering in the eyes of the so-called “flies”.
- Blurred and split image.
- Feeling of pressure in the eye.
- Decreased visual acuity.
- Formation of a grid before the eyes.
Initially, a gradually growing cloudy spot appears before the patient’s eyes. If the localization of the hemorrhage is large, vision may completely disappear. The ability to see normally decreases especially quickly when there is bleeding in the center of the macular zone.
Even a minor hemorrhage in the organ of vision requires professional consultation with a doctor, since there is a risk of retinal detachment, and this condition already leads to blindness.
Diagnosis of central retinal artery occlusion
The diagnosis is made according to the medical history and characteristic clinical picture.
Instrumental studies:
- Visometry.
- Perimetry.
- Ophthalmoscopy.
- Listening to the heart and carotid arteries.
- Fluorescein angiography (topical diagnosis of embolus).
- Doppler examination of the carotid arteries.
- Blood pressure measurement.
- Electrocardiographic study.
Laboratory research:
- UAC.
- OAM.
- Wasserman reaction.
- Blood sugar level.
- Hbs antigen.
Causes
Ophthalmologists call undertreated or uncorrected angiopathy of the visual organs the main cause of retinal angiosclerosis. At this stage, the pathological process is complicated by structural deformations of the retina, impaired conduction of impulses along the optic nerve, and multiple hemorrhages in the space between the retina and the underlying layer.
Since angiopathy of the retinal blood vessels develops against the background of systemic diseases, angiosclerosis is characterized by the same set of provoking factors:
- hypertension, in which pressure causes the walls of blood vessels to stretch, crack and become denser;
- atherosclerosis of the vessels of the head, in which the lumen of the arteries supplying the retina narrows due to cholesterol deposits;
- diabetes mellitus and other endocrine diseases, in which the capillary walls become thinner, microcirculation slows down, and the risk of thrombosis increases;
- rheumatic damage to the walls of arteries and capillaries;
- systemic vascular anomalies such as Buerger-Raynaud syndrome, periarteritis, periphlebitis and others;
- diseases of the hematopoietic system, in which platelet aggregation increases and small vessels become clogged with blood clots.
In addition to pathological causes, retinal angiosclerosis can occur against the background of physiological processes: toxicosis during pregnancy and age-related changes. The role of bad habits in the development of the condition is great: according to statistics, such a diagnosis often accompanies alcoholism and tobacco addiction.
Good to know! Doctors call radiation sickness the rarest cause of sclerotic changes in the retinal capillaries.
Treatment of central retinal artery occlusion
If the symptoms of occlusion of the central retinal artery lasted less than a day, it is necessary to immediately massage the eye using a special technique and puncture the anterior chamber.
- Antibacterial therapy, anticoagulants, vasodilators, antispasmodics and antisclerotic agents are mandatory.
- Cauterization with a laser beam.
- In parallel, therapy is carried out for the underlying disease that caused the occlusion.
Complication: atrophy of the optic nerve with a sharp decrease in the function of the visual analyzer.
Essential drugs
There are contraindications. Specialist consultation is required.
- Atropine sulfate (an antispasmodic to relieve spastic processes, to create drug-induced mydriasis). Dosage regimen: 0.1% atropine sulfate solution 0.5 ml is administered retrobulbarly.
- Caffeine (psychostimulant and analeptic). Dosage regimen: injection of 1.0 ml of 10% caffeine solution under the skin.
- Eufillin (has antispasmodic, vasodilator and bronchodilator effects). Dosage regimen: 10 ml of 2.4% aminophylline solution is administered intravenously. There are 15 injections per course.
- Nicotinic acid (vasodilator). Dosage regimen: 1 ml of 1% nicotinic acid solution is administered intramuscularly once a day. There are 15 injections per course.
- Fibrinolysin (fibrinolytic agent). Dosage regimen: 1000 units of fibrinolysin on novocaine with heparin 500 units are administered retrobulbarly.
Diagnosis and treatment of retinal hemorrhage
During diagnostic procedures, the doctor will examine the fundus of the eye using an ophthalmoscope. Patients with signs of retinal hemorrhage are required to undergo a general blood test; such a laboratory test will help identify the root cause of the development of the pathology.
If there is severe damage to the retina and extensive hemorrhage, then an operation is performed - vitrectomy. During surgery, formed blood clots and clouded areas of the vitreous body of the organ of vision are removed. The ability to see normally after surgery is restored within a few weeks. If the lesions of the optic nerve and retina were voluminous, then after the recovery period vision may remain poor.
Drug therapy includes vascular-strengthening and hemostatic pharmacological agents. Patients are required to be prescribed vitamins K and C, because vitamin preparations improve blood clotting and have a positive effect on the walls of blood vessels.
If a moderate hemorrhage in the retina is diagnosed, which is not associated with the progression of serious diseases in the body, then patients are advised to rest and the load on the organ of vision should be reduced. Doctors advise sitting with your eyes closed for a while; such preventive measures promote natural blood sedimentation. You should take care of the hygiene of the organ of vision; you should not allow specks or any foreign bodies to get into your eyes. If you follow all the ophthalmologist's recommendations, your ability to see normally will be restored within 2.5-4 weeks.
For preventive purposes, patients who have weak retinal vessels are advised to avoid sudden bends down or turns of the head. In addition, you should constantly strengthen your immune system and promptly treat common pathologies, then the risk of bleeding into the retina tissue will be significantly reduced.
For diagnosis and treatment of hemorrhage in the retina of the eye, contact medical institutions in Moscow (Kolomenskaya metro station and VDNKh metro station) and Vidnoye
Clinical signs
As a rule, patients note a sudden and persistent decrease in vision or sectoral loss of visual fields. Before the development of the characteristic pattern of ACAS, complete blindness occurs in approximately 15% of cases.
The decrease in visual acuity is significant: in 10% of cases, blindness occurs, in 50% of cases, fingers can be distinguished from the face, in 20%, visual acuity is 0.1-0.2. If any of the branches of the central nervous system is affected, visual acuity may be preserved, but defects occur in the visual field.
In young people, embolism of the central nervous system or its branches is more often observed. This occurs due to endocrine and septic diseases, acute infections, rheumatism, and injuries.
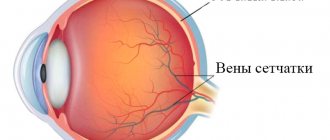
When examining the fundus, a typical finding is gray-white diffuse opacification of the retina, narrowing of individual or all branches of the central retina. In the area of the central fovea, an area of bright hyperemia is detected, standing out against the background of blanching of the retina, called the “cherry pit” symptom. This is explained by the thinning of the retina and the translucency of the bright red lining of the vessel in the indicated place. At the beginning of the disease, the optic disc remains pink in color and only then gradually turns pale due to its atrophy.
Sometimes a characteristic ophthalmoscopic picture may be absent: the area of retinal edema is localized only paramacularly or in the form of scattered areas. In such cases, the arteries are narrowed slightly, which indicates a small degree of occlusion. The presence of an additional cilioretinal artery often eliminates the “cherry pit” symptom and provides high visual acuity due to the preservation of central vision.
With embolism of the central nervous system, the prognosis is always pessimistic. In young people, after a spasm, vision can return almost completely; the prognosis in older people is much worse.
Blockage of any of the branches of the central nervous system partially reduces vision, and only the corresponding sector of the visual field is lost.
Treatment
The methods by which retinal angiosclerosis is eliminated depend on the degree of change in microcirculation, the nature of such processes and the reasons that caused them. In general, the scheme of conservative effects is designed in such a way as to enhance metabolic processes, improve nutrition of the retina, and normalize blood circulation in the structures of the eyeball. For this purpose, several groups of drugs are prescribed:
- Medicines for vasodilation
- “Pentoxifylline”, “Agapurin”, “Vazonit” and their analogues. Drugs in this group are suitable for the treatment of angiopathy of any origin. They prevent the formation of blood clots and protect the walls of blood vessels from unwanted changes.
- Anticoagulants
- “Trombonet”, “Aspirin Cardio” or “Ticlopidine”. Drugs in this group are prescribed for an increased risk of thrombosis or for blockage of the ocular vessels that has already occurred, as well as for angiosclerosis in hypertensive patients.
- Metabolism stimulants
— oral medications “Neurorubin”, “Milgamma”, “Mildronat”, injection forms of Riboxin, nicotinic acid, “Cocarboxylase”, ATP and vitamin-mineral complexes in tablets and injections. Additionally, the doctor may prescribe local medications - Taufon or Emoxy-Optic drops.
- Venotonics
- “Phlebodia”, “Vasoket”, “Normoven” and their analogues. Drugs in this group are prescribed if venous stasis is detected during the diagnostic process. They are used as adjuncts for diabetic forms of retinal angiosclerosis.
- Microcirculation stimulants
- “Cavinton” and “Actovegin”. Drugs of this group are indispensable in the presence of ischemic and congestive processes, signs of retinal dystrophy. Drugs that reduce the degree of permeability of the walls of arteries and veins - “Ditsinon”, “Parmidin”, natural remedies with ginkgo biloba extract - will help to strengthen and complement their effect.
Despite the abundance of various medicinal groups, they all provide short-term help, but do not eliminate the cause of the disease. Therefore, treatment of retinal angiosclerosis always contains actions aimed at relieving the original source of the problems:
- for diabetes mellitus, a low-carbohydrate diet, glucose-lowering drugs or insulin, substances with lipoic acid and antioxidants, as well as moderate physical activity are prescribed;
- in case of hypertensive origin of the pathology, antihypertensive drugs are prescribed, in addition - statins and sedatives;
- for autoimmune (rheumatoid) and traumatic pathologies, glucocorticoids, Lidase and Chymotrypsin are used in the form of injections, electrophoresis and tissue treatment with Biosed, Humisol, and vitreous are prescribed.
To accelerate the restoration of trophism and functionality of the retina, physiotherapy is prescribed: acupuncture, pulse and color exposure, magnetic therapy, pneumomassage and sessions using the Sidorenko Glasses simulator. To keep blood vessels in good shape, yoga classes, swimming, and massage courses for the collar area are recommended.
Surgical treatment of fundus vascular sclerosis
not used due to their small diameter and difficulty of access to them. Minimally invasive techniques are used only to eliminate complications of angiosclerosis - retinal rupture and detachment. Laser coagulation is considered the most effective and minimally traumatic method of restoring its integrity. In addition, vitrectomy can be performed: removal of the vitreous body and reconstruction of the retina with subsequent fixation.
Causes of angiopathy:
- hypotension or hypertension;
- atherosclerosis;
- hyperglycemia in diabetes mellitus;
- autoimmune processes;
- traumatic causes;
- hereditary diseases.
The listed conditions can negatively affect the condition of veins and arteries throughout the body. With retinal angiopathy, the following changes occur:
- violation of the tone of the vascular wall;
- the occurrence of vasospasm;
- thrombosis;
- formation of atherosclerotic plaques.
These changes lead to ischemic changes in the retina of the eye, i.e., a deterioration in its nutrition. As a result, oxygen starvation or tissue hypoxia occurs. If left untreated, a complication of angiopathy develops.
Diagnostics
Angiopathy can be confirmed by a classic visual examination of the fundus - ophthalmoscopy. During the study, the doctor records a change in the vascular pattern: the appearance of additional branches or excessive tortuosity of arterioles and venules, expansion or narrowing of their diameter indicate in favor of this pathology. To confirm the diagnosis and identify the causes of the anomaly, additional diagnostic procedures are performed:
- MRI of the eyeball and head, with which you can detect functional and trophic disorders of soft tissues;
- CT and radiography of retinal vessels with contrast, with the help of which it is possible to visualize even minor violations of vascular patency;
- Dopplerography and ultrasound of the retina, which give an idea of the speed and direction of blood flow in the eyeballs.
Based on the results obtained, treatment tactics for retinal angiosclerosis are developed.