Conjunctivitis is the most common eye inflammation, accounting for almost a third of all ophthalmological pathologies. It is noteworthy that chronic conjunctivitis is more often diagnosed in middle-aged and elderly patients, while acute forms tend to occur in children. Often the chronic form of conjunctivitis is combined with blepharitis, keratitis, dry eye syndrome and meibomitis.
Features of chronic conjunctivitis
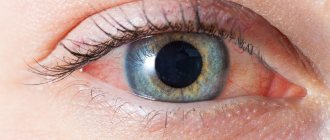
Chronic conjunctivitis is a protracted and stable catarrh of the conjunctiva, which can be of an infectious or non-infectious nature. Among the subjective symptoms of conjunctivitis (the patient's sensations) are itching, burning, photophobia and increased fatigue, as well as the effect of sand in the eyes. Objective symptoms: hyperemia and slight mucopurulent exudate.
Types of conjunctivitis:
- bacterial (streptococci, gonococci);
- allergic;
- chlamydial;
- dystrophic (exposure to paints, gases, chemicals);
- angular (diplobacillus Morax-Axenfeld);
- fungal (spirotrichilosis);
- viral (herpes simplex, adenovirus).
With follicular conjunctivitis, follicles form on the mucous membrane, and with hemorrhagic conjunctivitis, hemorrhages occur. Diagnosis of chronic conjunctivitis is carried out using biomicroscopy, refractometry, bacteriological culture and allergy testing. Treatment of the disease is based on eliminating the cause of inflammation. Local use of etiopathogenetic drugs and symptomatic therapy are prescribed.
Causes
At the moment, there are many reasons for inflammation of the eye mucosa, and determining the factors that led to inflammation is a rather difficult task. But the success of treating this disease depends precisely on the correct determination of the causes of inflammation.
The incubation period of conjunctivitis, depending on the type, ranges from several hours (epidemic form) to 4-8 days (viral form).
So, the most common cause of conjunctivitis is the following:
- Staying in a room where various aerosols and other substances of chemical origin are used
- Prolonged stay in an area of high pollution
- Impaired metabolism in the body
- Diseases such as meibomitis, blepharitis
- Avitaminosis
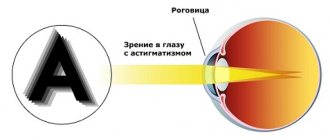
- Impaired refraction - myopia, farsightedness, astigmatism
- Inflammation in the sinuses
- Too bright sun, wind, too dry air
If conjunctivitis has developed due to occupational reasons, then it is very important to follow preventive measures to eliminate the harmful effects of irritating factors.
Causes of chronic conjunctivitis
All chronic conjunctivitis is divided into infectious and non-infectious. There is also a division into endogenous and exogenous. The cause of inflammation can be a constant mechanical effect on the eyeball (improper growth of eyelashes, grains of sand and particles of granular substances getting into the eyes).
Non-infectious exogenous forms are often caused by prolonged physical or chemical irritation of the eyeball. This may be exposure to dust, steam, acids and alkalis, cosmetics, as well as prolonged visual stress, which led to eye strain. Often, the chronic form of conjunctivitis is diagnosed in workers in the coal, cement, paper and flour milling industries, hot shops and chemical production.
Recurrent chronic conjunctivitis of a non-infectious nature often develops due to refractive error that is not treated. These are uncorrectable astigmatism, presbyopia, myopia and farsightedness. Dry eye syndrome or electroophthalmia (snow blindness) may also be the cause.
Endogenous factors of chronic conjunctivitis:
- helminthic infestation;
- demodex;
- seborrhea;
- anemia;
- avitaminosis;
- chronic diseases of the gastrointestinal tract (cholecystitis, gastritis, enterocolitis);
- diabetes;
- hyperglycemia.
Allergic conjunctivitis has a chronic course and seasonal dependence. It is often combined with rhinitis, asthma, and atopic dermatitis.
Infectious conjunctivitis can be caused by inflammation of the eyes (blepharitis, dacryocystitis), diseases of the ENT organs (sinusitis, tonsillitis). During diagnosis, cytogram and culture reveal staphylococci, proteus, enterobacteria, moraxella, chlamydia, pseudomonads and other pathogenic microorganisms. Sometimes chronic conjunctivitis occurs due to improper treatment of the acute form.
Symptoms of the disease
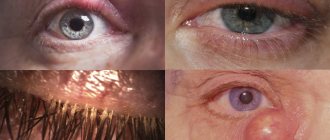
The symptoms of chronic conjunctivitis are similar to the acute disease, but are less pronounced. During remission, clinical manifestations may be absent. Exacerbations are provoked by repeated exposure to allergens, hypothermia, and stress.
Persistent symptoms include:
- foreign body sensation;
- feeling of itching and burning;
- lacrimation;
- redness of the mucous membrane;
- slight swelling.
Such symptoms are observed when the nature of the disease is non-infectious. If the cause is an allergy, sneezing and excessive discharge of fluid from the nose occurs.
Viral conjunctivitis is accompanied by the formation of a small amount of clear discharge. Bacterial infections cause a purulent, thick discharge.
Due to constant inflammation, dry eye syndrome develops. The conjunctiva thickens, sometimes to the point that the person cannot close their eyes completely. Constantly flowing tears irritate the skin and erosions appear on it.
Discomfort and burning affect the general condition of the patient. He becomes irritable, performance decreases, and concentration is lost.
Symptoms
Chronic conjunctivitis is characterized by a gradual increase in symptoms that persist for a long period. Typically, the symptoms of conjunctivitis intensify at night, as well as with prolonged use of artificial lighting.
Patients complain of the following occurrences:
- burning;
- “clogged” eyes;
- heaviness of the eyelids;
- photophobia;
- lacrimation;
- rapid fatigue of the visual system;
The amount and nature of the discharge depends on the etiology of conjunctivitis, but often it is scanty or moderate, has a mucous or mucopurulent form. When diagnosing, the doctor reveals slight hyperemia of the conjunctiva and roughness of the mucosa.
Allergic conjunctivitis causes the appearance of follicles and papillae on the mucous membrane, which provoke itching, and less commonly, visual disturbances and damage to the cornea. Sometimes this form of conjunctivitis is combined with eyelid dermatitis, uveitis, keratitis, retinitis or neuritis.
Symptoms
In the chronic form of the disease, symptoms appear slowly and in a mild form. Signs of pathology tend to intensify at night and worsen in the evening. This is also affected by prolonged exposure to artificial lighting. In this case, the person complains of the following manifestations:
- burning;
- feeling of sand in the eyes;
- increased sensitivity to light;
- uncontrollable lacrimation;
- decreased visual function.
Purulent discharge mixed with mucus is not abundant, but mainly depends on the type and degree of development of conjunctivitis.
Upon examination, the doctor observes slight roughness of the mucous membrane and redness. In the allergic form, follicles may appear that cause itching, burning, and pain in the eyes. Complications include corneal damage and decreased vision function.
This type of disease is in most cases combined with retinitis, keratitis, and uveitis.
Diagnosis of conjunctivitis
The main feature of chronic conjunctivitis is the discrepancy between the severity of symptoms and changes in the eye. This greatly complicates the diagnosis and search for the cause of inflammation. A diagnosis can only be made at a meeting with an ophthalmologist with a detailed description of complaints and examination of the eyeball. Ophthalmological and laboratory tests will help you see the picture of the disease from different angles.
Methods for diagnosing changes in chronic conjunctivitis:
- visometry (determining visual acuity);
- biomicroscopy (detection of conjunctival defects: hyperemia, velvety, papillary growths, loosening, etc.);
- refractometry and skiascopy (allows you to exclude refractive errors);
- Norn test and Schirmer test (for dry eye syndrome);
- fluorescein installation test;
- bacteriological culture of a smear from the conjunctiva (to determine the pathogen).
If chronic conjunctivitis is a secondary condition, additional consultation with an otolaryngologist, endocrinologist, allergist, dermatologist or gastroenterologist will be required. According to indications, radiography of the nasal sinuses, bacteriological culture from the nasopharynx, ELISA, PCR and RIF diagnostics for chlamydia are prescribed. Sometimes they also determine the level of glucose in the blood, perform allergy tests and examine eyelashes to detect demodicosis.
If you have conjunctivitis, you should consult a doctor promptly, since its symptoms may resemble the clinical picture of other diseases. Patients often confuse inflammation with dry eye syndrome and computer syndrome. All three conditions are similar in symptoms, but the treatment will be radically different. It must be remembered that improper treatment can cause more harm than no treatment at all.
What is eye conjunctivitis?
Conjunctivitis is an inflammation of the mucous membrane of the eye (conjunctiva) caused by allergies, bacteria, viruses, fungi and other pathogenic factors. Manifestations of this disease can lead to redness and swelling of the eyelids, the appearance of mucus or pus, lacrimation, burning and itching, etc. Conjunctivitis is the most common eye disease - it accounts for about 30% of all eye pathologies.
What is the conjunctiva? This is the mucous membrane of the eye, covering the back surface of the eyelids and the front surface of the eyeball up to the cornea. It performs quite important functions that ensure the normal functioning of the organ of vision.
- It is usually transparent, smooth and even shiny.
- Its color depends on the underlying tissues.
- She takes care of everyday tear production. The tears it produces are enough to moisturize and protect the eye. And only when we cry, the main large lacrimal gland comes into operation.
Conjunctivitis, in addition to redness of the eyes that spoils the appearance and constant involuntary lacrimation, causes a number of extremely unpleasant symptoms with which it is impossible to continue living as usual.
How to cure chronic conjunctivitis
Therapy for chronic conjunctivitis will be successful only if the cause of the inflammation has been identified and eliminated. For ametropia, wearing glasses or contact lenses, or laser vision correction is indicated.
If conjunctivitis is caused by constant irritation of the eyeballs, it is necessary to eliminate the provoking factors: remove foreign bodies from the conjunctival vault, epilate the eyelashes. When a concomitant chronic pathology is identified during the diagnostic process, treatment should be carried out under the supervision of an appropriate specialist.
For local use, cold lotions with astringent solutions (resorcinol) and herbal tinctures (chamomile, tea) are prescribed. It is allowed to use zinc sulfate, adrenaline and dicaine. It is possible to carry out instillations into the conjunctival cavity using antibacterial, vitamin and disinfectant drops, as well as artificial tears and corticosteroids. At night, you can apply ointment to your eyelids.
Any medications for chronic conjunctivitis should be prescribed by a doctor. The choice will depend on the type of inflammation and its causative agents. Conjunctivitis is often treated with Oftalmoferon. This remedy fights against viruses and microbes, eliminates the symptoms of inflammation and allergies. In the treatment of chronic conjunctivitis, these drops have the advantage of a wide spectrum of action and a short list of contraindications.
Since all chronic diseases require long-term treatment, and conjunctivitis is no exception, the risk of fungal infection increases. To prevent this, ophthalmologists include Colbiocin ointment or drops in therapy, which contain antifungal components.
Principles of treatment of different forms of conjunctivitis
- When chronic conjunctivitis is accompanied by purulent discharge, you need to use antimicrobial drugs, a solution of syntomycin or sodium sulfapyridazine, as well as sodium sulfacyl. In this case, drops are instilled three times a day, and disinfectant ointments are applied at night.
- Adenoviral conjunctivitis is treated with solutions of Interferon or Laferon. Intensive administration of drugs is necessary in the first days of treatment, gradually reducing the dose until symptoms disappear. Additionally, antiviral ointments (tebrofen, bonaftone) are prescribed.
- As an additional therapy, it is allowed to take homeopathic medicines, which will strengthen not only the visual system, but the entire body as a whole.
- To prevent dryness, tear substitutes (Oftagel, Vidisik) are prescribed.
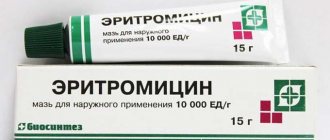
- For bacterial inflammation, Diclofenac, antibiotics and ointments (tetracycline, erythromycin, gentamicin) are prescribed. The discharge should be removed during washing with a solution of boric acid and furatsilin. Additionally, Picloxidine drops are prescribed.
- Chlamydial conjunctivitis requires systemic treatment. Levofloxacin, erythromycin ointment in the eyes, Lomefloxacin drops, sometimes Diclofenac, but more often Dexamethasone are prescribed. Treatment may continue for weeks or months.
- In case of purulent lesions, the eyes are washed as directed. First, the discharge is removed with antiseptics, then ointments (tetracycline, erythromycin) are prescribed. If there is swelling, Diclofenac should be used.
- For allergic conjunctivitis, topical drugs (Spersallerg, Allergoftal) and the administration of Lecrolin or Alamid are prescribed. After symptoms have resolved, preventive therapy is continued. For recovery, Solcoseryl is prescribed in gel form.
You need to prepare in advance for the fact that the treatment of chronic conjunctivitis will be long. Therefore, a change in drugs is required during the process to avoid addiction.
Viral conjunctivitis
The cause of infection is smallpox, measles, herpes viruses, adenovirus, and atypical trachoma virus. Conjunctivitis caused by adenoviruses and herpes viruses is very contagious; patients with such forms need to be isolated from others.
Symptoms of conjunctivitis:
- Severe inflammatory reaction of the conjunctiva (swelling, redness due to vasodilation).
- Inflammation of the conjunctiva occurs almost simultaneously in both eyes
- Despite the pronounced inflammatory reaction, there is no abundant purulent discharge.
- As a rule, eye inflammation is accompanied by fever and inflammation of nearby lymph nodes.
How to treat conjunctivitis of viral etiology?
There is currently no clear answer on how to treat viral conjunctivitis in adults. It should be remembered that treatment should be aimed at destroying the causative agents of the disease, which can be varied.
The basis of treatment is antiviral drugs intended for general and local use. Local medications include drops and ointments containing tebrofen or oxolin. And also an interferon solution.
In acute cases, use Tobrex and Okacin eye drops up to six times a day. For severe swelling and irritation, use anti-inflammatory and antiallergic drops: Alomide, Lecrolin twice a day. In case of acute conjunctivitis, it is forbidden to blindfold or tape your eyes, as this greatly increases the risk of developing inflammation of the cornea.
Parasitic conjunctivitis
There is a type of helminth that affects the eyes. Onchocerciasis is transmitted through insect bites and is characterized by an itchy rash and filarial scabies. Almost every patient with onchocerciasis is diagnosed with a chronic form of conjunctivitis.
During diagnosis, pinpoint opacities of the cornea are detected, which either disappear or increase and form larger lesions. At the early stage of the disease, only subjective symptoms occur without structural changes in the eyeball. Biomicroscopy can detect microfilariae in the cornea.
For onchocerciasis, the prescription of Ditrazine and Antikrol is required (sequential or simultaneous therapy). Ditrazine acts on microfilariae, and Antikrol affects adult parasites. With the mass death of parasites, an allergic reaction is observed, complicating treatment. Severe side effects occur in 30% of cases, so it is important to take antihistamines and corticosteroids at the same time.
Causes of conjunctivitis
The causes of conjunctivitis can be different, which determines its type (purulent, bacterial, viral). Most often, the disease can be caused by an infection (virus or bacteria). Infectious conjunctivitis develops if a child comes into contact with an infected person through touching, coughing or sneezing. You can also become infected through unwashed hands or infected objects, water, and towels while swimming.
If your child has been diagnosed with an eye infection, including conjunctivitis, do not allow him to share personal hygiene items with other people. The infected person carries the infection until the discharge from the affected eye disappears. Children diagnosed with infectious conjunctivitis should not attend kindergarten or school. Child care should include regular hand washing with disinfectants to prevent transmission of infection to other family members and others.
Bacterial conjunctivitis is often caused by the same type of bacteria that causes throat infections. Viral conjunctivitis can appear against the background of colds. Viral and bacterial conjunctivitis in children is easily transmitted through hand contact.
Purulent conjunctivitis is provoked by pyogenic bacteria, allergic conjunctivitis is caused by allergens, which include, for example, pollen. Follicular conjunctivitis - various infections, viruses and fungi. An ophthalmologist must diagnose and treat eye diseases in children.
Prognosis and prevention
Chronic conjunctivitis is difficult to cure. Inflammation is characterized by frequent relapses, so complete recovery is possible only by eliminating the causes and systematic therapy. The long course of inflammation of the conjunctiva, taking months and even years, can limit the patient’s professional suitability and ability to work.
Prevention of conjunctivitis involves eliminating hazards (domestic and professional), as well as using protective equipment when working at work. Inflammation can be avoided through timely correction of refractive errors and treatment of other pathologies of the visual system.
Conjunctivitis does not immediately become chronic, and therefore it is necessary to monitor the condition of the visual system and undergo regular preventive examinations. If alarming signs occur, you should consult an ophthalmologist and undergo full treatment before complications begin.
Sources used:
- Ophthalmology. Atlas-reference book / D. Kanski. - M.: Medical literature, 2009.
- Medicinal reference book for an ophthalmologist / M.L. Krasnov, N.B. Shulpina. - M.: State Publishing House of Medical Literature, 1998.
- Parasitic eye diseases / Yu.F. Maychuk. - Moscow: Mir, 1988.
- National Eye Institute
Prevention
The basic rule for preventing the chronic form of the disease is timely consultation with a doctor. After a thorough diagnosis, you can identify the irritant and eliminate it in time. In addition, the following recommendations should be followed:
- Adhere to a healthy lifestyle. Nutrition should be balanced and rich in vitamins. Full sleep, especially after prolonged exercise.
- To refuse from bad habits. It is important to consider that smoking negatively affects the mucous membranes of the eyes and causes irritation.
- In all conditions, observe the rules of personal hygiene.
- When using contact lenses, monitor their condition and place them in a disinfectant solution.
- Undergo a preventive examination with an ophthalmologist 1-2 times a year.
- Use sun protection glasses and limit exposure to artificial light on your eyes.
- Follow safety precautions at work.
By contacting an ophthalmologist in a timely manner, the development of a chronic form of the disease can be avoided. If there is a predisposition to the development of ophthalmological pathologies, you should be examined by a doctor more often.
Treatment methods for conjunctivitis
With proper treatment, conjunctivitis is not dangerous and goes away within a few weeks. The course of treatment depends on the cause of the disease.
Ophthalmologists at Family Doctor have extensive experience in diagnosing and treating conjunctivitis. The family orientation of our clinics allows us to provide quality medical care to even the youngest patients. This aspect is important in the treatment of conjunctivitis, since children often suffer from it (after all, children tend to rub their eyes, and their hands can be dirty).
Treatment of allergic conjunctivitis
If conjunctivitis is allergic, it is important to identify the allergen that caused the disease. In the future, it will be necessary, if possible, to exclude contact with this allergen.
The course of treatment for allergic conjunctivitis includes the use of antihistamines. It is also possible to prescribe eye drops containing corticosteroid hormones.
Treatment of bacterial conjunctivitis
In the case of bacterial conjunctivitis, antibiotic eye drops or eye ointments are used to speed up the healing process.
Treatment of viral conjunctivitis
For viral conjunctivitis, drugs with interferon are usually prescribed.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating