Conjunctivitis is a very common ophthalmological disease. It is characterized by inflammation of the conjunctiva, the mucous membrane that covers the inner surface of the eyelids and sclera. Eye drops are an effective pharmacological form that allows you to actively act on inflamed tissues with conjunctivitis.
In this article
- What to put in your eyes for conjunctivitis?
- What medications can be used for viral conjunctivitis?
- What should I use in my eyes for bacterial conjunctivitis?
- Treatment of allergic conjunctivitis with drops
- How to put eye drops correctly?
- Is it possible to choose eye drops yourself?
What to put in your eyes for conjunctivitis?
Many people believe that conjunctivitis is not a serious condition. Many people suffer from it in childhood and do not remember exactly how they were treated, so they believe that this disease does not pose a particular danger to the eyes. In fact, this opinion is wrong. Like any other disease, conjunctivitis requires timely initiation of treatment, since in its absence the disease can lead to:
- blepharitis;
- dry eye syndrome;
- formation of scars on the cornea;
- changes in the structure of the eyelids;
- keratitis.
If conjunctivitis is diagnosed early, it is quite easy to treat. The main thing is to contact an ophthalmologist at the moment when the first symptoms of the disease are detected. The eyes are an unprotected organ. They regularly suffer from bright sunlight, dust particles, and computer radiation. If pathogenic viruses or bacteria enter the mucous membranes of the eyes, an inflammatory process begins. This is conjunctivitis. The characteristic symptoms of this disease are:
- redness of the sclera;
- increased tearfulness;
- burning and itching;
- formation of mucous or purulent discharge;
- dry eyelids;
- hyperemia.
The ophthalmologist must decide which medications to use for conjunctivitis. Eye drops vary greatly in composition. This is due to the fact that the disease can have different forms, each of which has its own specifics. There are three types of conjunctivitis, namely:
- bacterial;
- viral;
- allergic.
For each form of the disease in modern pharmacology there are different drops. The difference between them is that their main components act on a specific pathogen. For viral conjunctivitis, drops are used that can have an antiviral effect. The bacterial form of the disease will require antibiotics. Accordingly, only an ophthalmologist can make a decision on prescribing a drug.
Effect on other body systems
Other body systems may also be affected by eye drops. Headaches are the most common negative effect of eye drops, although stomach problems, including diarrhea and nausea, may also occur. These effects are not common and are most common with drops that deliver medications.
The drops may also affect the cardiopulmonary system. Fast heartbeats and difficulty breathing can occur from some types of droplets, while others result in slower breathing and slower heartbeat rhythms. An otherwise healthy patient will usually not have serious complications from these effects, but a patient with pre-existing heart disease could potentially make the condition worse.
You may be interested in Vita Yodurol Drops: price, instructions, reviews
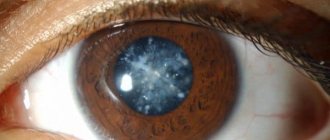
Some types of drops can cause quite serious damage to the eyes. Anesthetic drops can damage the cornea, and decongestant drops can cause glaucoma. Patients who experience a sudden change in vision should consult a doctor because some of these conditions can permanently impair vision.
What medications can be used for viral conjunctivitis?
If the patient has been diagnosed with a viral form of conjunctivitis, the ophthalmologist will recommend drops that contain components that suppress the replication of the virus. Also, these drugs can have a regenerating and calming effect on the conjunctiva. The doctor will decide which of them to instill into the eyes. Self-selection of drops is unacceptable. For adenoviral conjunctivitis, certain drugs are prescribed, for enteroviral conjunctivitis, others are prescribed. The following eye drops have proven to be highly effective:
- "Ophthalmoferon". Popular drops with antiviral, antihistamine, immunomodulatory effects. The drug has many advantages. It can be used to treat conjunctivitis in adults and children. The main active components of Oftalmoferon are interferon, aimed at suppressing the virus, and diphenhydramine, which effectively relieves itching and burning. The duration of treatment is usually no more than a week. The ophthalmologist decides how much to drip “Ophthalmoferon” individually in each specific case. During the first days, it is recommended to instill the drug into the eyes no more than 6 times. In subsequent ones - no more than three. The drops have no contraindications for use. The exception is individual intolerance to the components of the drug.
- "Aktipol". These eye drops contain para-aminobenzoic acid, which is an inducer of endogenous interferon. It increases the amount of proteins released by the body's cells in response to damage from viruses. Effectively eliminates "Actipol" and swelling of the eyelids - one of the most common symptoms of conjunctivitis. The drug has virtually no contraindications and can be used to treat children, but only with the consent of a doctor. Actipol is instilled into the eyes, 1-2 drops 6-8 times a day. The duration of treatment is determined by the ophthalmologist after examining the patient. The drug is recommended to be used after clinical recovery - 3 times a day for 5 days.
- "Florenal". Another effective eye drops that ophthalmologists prescribe to patients with a viral form of conjunctivitis. The drug has a pronounced antiviral effect and is able to suppress the proliferation of viral cells in the tissues of the visual organs. Florenal can be used for conjunctivitis caused by the herpes virus. The advantage of the drug is that it has an exclusively local effect and is not absorbed into the bloodstream. Instill Florenal 1-3 times a day, a couple of drops. The duration of treatment is prescribed by the ophthalmologist. In some patients, the drug may cause side effects, such as itching and burning in the eye area. Usually they are short-lived and do not require discontinuation of the drops.
Why are vasoconstrictor eye drops dangerous?
Few people realize the dangers of the drugs that are most often prescribed for dry eye syndrome. They help relieve redness resulting from overexertion and prolonged work at the computer. But after 5-7 days, vasoconstrictor drugs become addictive.
A decrease in the sensitivity of vascular receptors to the active ingredients leads to the fact that the redness of the eye membrane becomes chronic. In addition, there is a risk of impaired nutrition and blood supply to the tissues of the visual organs, and narrowing of the lumen of blood vessels.
Ophthalmologists say that the use of vasoconstrictor drugs for xerophthalmia can worsen the condition of the visual organs. Due to disruption of the stability of the tear film, the eyes become too sensitive and vulnerable. The use of drops that constrict blood vessels in this situation can further injure the eyes. Self-medication often ends in blepharitis, conjunctivitis, and corneal ulcers.
Drops with a vasoconstrictor effect can be used in short courses and only after consultation with a doctor. They have contraindications, so uncontrolled use of such drugs can cause harm to health.
What should I use in my eyes for bacterial conjunctivitis?
Eye drops that are used to treat bacterial conjunctivitis contain an antibiotic. It affects the causative agent of the disease, helps to destroy bacteria that cause the inflammatory process. Most often, doctors prescribe drops with a broad-spectrum antibiotic, for example:
- "Levomycetin". This drug is very popular due to its affordable price and high effectiveness. It has a good therapeutic effect and rids the sick person’s body of gram-positive and gram-negative bacteria. The drug can be dripped in case of damage to the visual organs by streptococci, staphylococci, chlamydia, Escherichia coli and Pseudomonas aeruginosa. Ophthalmic ophthalmologists prescribe 1 drop of Levomycetin into the eyes 3-4 times a day. The duration of the course of treatment is determined by the doctor. Usually the drug is used for no more than three days. The use of this medicine is not recommended for pregnant women and nursing mothers. Levomycetin should not be instilled into the eyes of newborns. For the treatment of “childhood” conjunctivitis, this drug can be used only when the child reaches two years of age.
- "Albucid". Another affordable drug that is regularly prescribed by doctors for the treatment of conjunctivitis in adults and children. The main active ingredient of the drug is sodium sulfacyl. This substance copes well with bacteria of any kind. "Albucid" is available in two concentrations - 20% and 30%. The first option is prescribed by ophthalmologists to pregnant women and children. The second is successfully used to treat adults. The drug penetrates into eyes affected by conjunctivitis very quickly and has an effective local effect. A small amount of it enters the blood. Albucid can be instilled into the eyes 4-6 times a day, 1-2 drops. The duration of treatment depends on the severity of the disease.
- "Tobrex". A modern medicine whose main active ingredient is the antibiotic tobramycin. It successfully relieves the inflammatory process caused by staphylococci, Pseudomonas aeruginosa and Escherichia coli, as well as other pathogenic microorganisms. The advantage of Tobrex is its recent appearance on the pharmacological market. Due to this, many bacteria did not have time to develop immunity against the active substance of the drug, which is why it is highly effective. Drops are not recommended for use by pregnant women, patients with impaired renal function, as well as myasthenia gravis and Parkinson's disease. The ophthalmologist determines how many days and how often Tobrex can be instilled into the eyes on an individual basis.
There are other effective drops for treating bacterial conjunctivitis. After conducting an examination, the ophthalmologist can prescribe those that, in his opinion, will best suit the patient and will not cause side effects.
Treatment of allergic conjunctivitis with drops
For allergic conjunctivitis, eye drops are used not for treatment, but to eliminate unpleasant symptoms: itching, burning, swelling. They also relieve redness of the sclera and conjunctiva. For patients with allergic conjunctivitis, ophthalmologists often prescribe the following antihistamines:
- "Allergodil." These eye drops have a combined action. They effectively relieve swelling and block histamine receptors. This drug fights a complex of symptoms characteristic of the allergic form of conjunctivitis: itching, redness, swelling of the eyelids. Allergodil is not recommended for use by women during pregnancy and lactation, as well as by children under 6 years of age. The drug is instilled 3 times a day, 1-2 drops into the conjunctival sac of each eye. After instillation, some patients experience blurred vision, but this usually does not last long - no more than an hour. In this regard, doctors recommend stopping driving during treatment.
- "Cromohexal". A drug whose main active ingredient is cromoglycic acid. It stabilizes the membranes of mast cells, thereby relieving allergy symptoms. The regularity of using Cromohexal can be from 1 to 4 times a day. The total course of treatment should not exceed one month. The drug has contraindications. It is not recommended for use by pregnant and lactating women, children under 5 years of age, or patients with kidney or liver failure. Cromohexal has proven highly effective as a prophylactic agent. It is often prescribed by ophthalmologists to people who suffer from chronic conjunctivitis. If you instill this drug into the eyes during remission, you can achieve stabilization of the condition during the allergy period. When treating conjunctivitis, the effect usually occurs a few days after starting to use the drops.
- "Dexamethasone." A potent drug that is used for severe cases of allergic conjunctivitis, when other treatment methods do not provide the desired effect. These eye drops are hormonal. They have a wide list of contraindications and side effects, and therefore their use must be agreed upon with the attending physician. Dexamethasone can be used only for allergic forms of the disease. For purulent eye lesions, its use is contraindicated. When treating acute conditions, ophthalmologists prescribe 1-2 drops every two hours. After the inflammatory process decreases - every 6 hours.
Systane Ultra. They are not antihistamines, but are effective in relieving redness and irritation from the eyes.
Systemic effect of eye drops
Oculocardial reflex Read more: Regional anesthesia
4. Systemic effect of eye drops
The effect of eye drops is not limited to the eye. Through the mucous membrane of the conjunctival sac and nasolacrimal duct, eye drops enter the bloodstream, exerting a systemic effect on the body. This is important. For example, the content of phenylephrine in one drop of a 10% solution is 5 mg (the volume of one drop is 1/20 ml). For comparison: the dose of phenylephrine for the treatment of arterial hypotension in adults is 0.05-0.1 mg IV. The drugs contained in eye drops enter the bloodstream faster than with subcutaneous injection, but slower than with intravenous injection (the toxic dose of phenylephrine when administered subcutaneously is 10 mg). The risk of toxic effects of eye drops is especially high in children and the elderly, so they are prescribed a less concentrated 2.5% solution of phenylephrine (Table 4). Note that among patients in need of ophthalmological intervention, a very large proportion are children and the elderly.
TABLE 4. Systemic effect of eye drops
| A drug | Mechanism of action/effect on the eye | Systemic side effects |
| Adrenalin | Sympathomimetic/mydriasis, ↓IOP | Arterial hypertension, tachycardia, headache |
| Atropine | Anticholinergic/mydriasis | Central anticholinergic syndrome* |
| Acetazolamide | Carbonic anhydrase inhibitor/↓IOP | Stimulation of diuresis, hypokalemic metabolic acidosis |
| Acetylcholine | Cholinomimetic/miosis | Bronchospasm, bradycardia, arterial hypotension |
| Scopolamine | Anticholinergic/mydriasis, vasoconstriction | Central anticholinergic syndrome* |
| Timolol | β-blocker/↓IOP | Bradycardia, bronchial asthma, heart failure |
| Phenylephrine | α-adrenergic agonist/mydriasis, vasoconstriction | Arterial hypertension, bradycardia |
| Cyclopentolate | Anticholinergic/mydriasis | Disorientation, psychosis, seizures |
| Echothiophate | AChE inhibitor/miosis, ↓IOP | Increased duration of action of succinylcholine, bronchospasm |
Echothiophate is an irreversible AChE inhibitor used to treat glaucoma. The entry of echothiophate into the systemic circulation causes a decrease in plasma cholinesterase activity. Succinylcholine is broken down by plasma cholinesterase, so echothiophate increases the duration of its action. However, the duration of action of succinylcholine does not increase very significantly - up to 20-30 minutes, so the risk of postoperative apnea is low. Inhibition of cholinesterase activity persists for 3-7 weeks after discontinuation of echothiophate eye drops. The muscarinic-like side effects of echothiophate (bradycardia during induction of anesthesia) are easily prevented by IV atropine or glycopyrrolate.
Eye drops with adrenaline can cause arterial hypertension, tachycardia and arrhythmia; the arrhythmogenic effect is potentiated by halothane. Injecting a solution of adrenaline directly into the anterior chamber of the eye does not cause disturbances in the cardiovascular system.
Timolol is a non-selective beta-blocker that inhibits the formation of aqueous humor and thereby reduces IOP. Timolol eye drops are one of the most common medications for the treatment of glaucoma. Treatment with timolol is associated with a small risk of intraoperative complications such as atropine-resistant bradycardia, arterial hypotension and bronchospasm.
5. General anesthesia
The decision on the choice of anesthesia technique is made by the patient, the anesthesiologist and the surgeon collectively during a joint discussion. Some patients do not even want to hear about regional anesthesia. Their fears may be due to fear of attending surgery, as well as pain they have experienced during previous operations performed under regional anesthesia. Although there is no clear evidence that either general or regional anesthesia is safer, there is widespread agreement that regional anesthesia does provide greater protection against surgical stress. General anesthesia is indicated when contact with the patient is difficult, since even a slight movement of the head during microsurgery can cause serious complications. Sometimes regional anesthesia is contraindicated due to the peculiarities of the surgical technique. In any case, before the operation, a definite decision should be made regarding the choice of anesthesia technique. The combination of regional anesthesia with deep sedation is contraindicated because it combines the risks of both techniques (eg, local anesthetic toxicity and airway compromise).
Premedication
Before ophthalmological operations, patients often experience anxiety, especially if the intervention is repeated and the risk of blindness is high. In children, concomitant congenital anomalies are common (for example, fetal rubella syndrome, Goldenhar syndrome, Down syndrome). Adult patients are most often elderly, with many concomitant diseases (for example, arterial hypertension, diabetes mellitus, coronary artery disease). All these factors should be taken into account when prescribing premedication.
Induction of anesthesia
The choice of anesthesia induction technique largely depends not on the eye disease and the nature of the operation, but on concomitant somatic diseases. The exception is patients with penetrating wounds and rupture of the membranes of the eyeball. For penetrating wounds and ruptures of the membranes of the eyeball, it is necessary to induce anesthesia gently, avoiding a pronounced increase in IOP. To prevent reaction to the endotracheal tube, a deep level of anesthesia and muscle relaxation should be provided before intubation. The severity of IOP elevation during laryngoscopy and tracheal intubation can be reduced by preliminary administration of lidocaine (1.5 mg/kg IV) or fentanyl (3-5 mcg/kg IV). As a muscle relaxant for intubation, it is not succinylcholine (which causes an increase in IOP) that should be used, but non-depolarizing muscle relaxants. The vast majority of patients with penetrating wounds and ruptures of the membranes of the eyeball have a full stomach, which serves as an indication for rapid sequential induction of anesthesia.
Maintenance of anesthesia and intraoperative monitoring
During ophthalmic surgery, the anesthesiologist is away from the airway, which emphasizes the particular importance of pulse oximetry. Airway pressure monitoring allows rapid recognition of airway leakage or unintentional extubation. To avoid kinking and obstruction of the endotracheal tube, it is advisable to use reinforced or right-angled models. ECG monitoring allows you to diagnose arrhythmias caused by the oculocardial reflex. During ophthalmological operations, children, unlike most other surgical interventions, are not cooled, but, on the contrary, overheated, because they are covered from head to toe in sheets that leave only part of their face exposed. Capnography can distinguish this complication from malignant hyperthermia.
Ophthalmological operations cause significantly less pain and stress than, for example, interventions on the abdominal organs. If the consequences of the patient's movements were not so dangerous, superficial anesthesia would be quite acceptable. Most ophthalmic operations are not accompanied by significant nociceptive stimulation, which, combined with the need to maintain an adequate depth of anesthesia, can lead to arterial hypotension, especially in the elderly. To prevent and eliminate arterial hypotension, infusion solutions are transfused and small doses of ephedrine (2-5 mg IV) are used. In addition, adequate muscle relaxation (provided by non-depolarizing drugs) makes superficial anesthesia acceptable, which reduces the risk of arterial hypotension.
Vomiting due to irritation of the vagus nerve is a common postoperative complication, especially after strabismus surgery. Straining and increased central venous pressure associated with vomiting increase the risk of postoperative ophthalmological complications (due to increased IOP) and aspiration. To prevent vomiting, metoclopramide (10 mg in adults) or small doses of droperidol (20 mcg/kg) are administered intraoperatively. Ondansetron is highly effective, but is not always available and is therefore usually used when the risk of complications is particularly high (eg, a history of postoperative nausea and vomiting).
Awakening and extubation
Although modern suture materials and suturing techniques have significantly reduced the risk of surgical wound dehiscence, awakening from anesthesia should still be smooth. Extubation under moderately deep anesthesia prevents coughing. When the end of the operation is near, the residual effect of muscle relaxants is eliminated with the help of AChE inhibitors, after which spontaneous breathing is restored. The supply of inhalational anesthetics is not turned off until sputum has been suctioned from the respiratory tract. After suctioning out the sputum, the anesthetic is stopped and lidocaine (1.5 mg/kg IV) is administered, which has the ability to suppress the cough reflex. Extubation is carried out 1-2 minutes after the administration of lidocaine against the background of inhalation of pure oxygen. Until the cough and swallow reflex is fully restored, it is very important to properly maintain the airway. Obviously, if there is a high risk of aspiration, this extubation technique is contraindicated.
Severe postoperative eye pain is rare. The most painful operations are for penetrating wounds and ruptures of the membranes of the eyeball, scleral plastic surgery and enucleation. Low doses of opioid (eg, 15–25 mg meperidine for adults) are usually sufficient for analgesia. Severe pain indicates increased IOP, corneal damage, and other surgical complications.
Oculocardial reflex Read more: Regional anesthesia
Information about the work “Anesthesia for ophthalmic operations”
Section: Medicine, health Number of characters with spaces: 26764 Number of tables: 4 Number of images: 0
Similar works
Anesthesia in ophthalmology
27579
0
5
... many different tasks. Patients are often elderly and burdened with various concomitant diseases, especially diabetes and hypertension. Drugs used in ophthalmology can affect the course of anesthesia. For example, drugs for the treatment of glaucoma, including the b-blocker timolol or phospholine iodide, which has anticholinesterase properties, may prolong the effect...
Anesthesia in otorhinolaryngology and ophthalmology
27927
0
0
... times, when performing anesthesia, the anesthesiologist must have a working anesthesia or mechanical ventilation device, a set for tracheal intubation, and a suction device. Anesthesia in ophthalmology Specific problems of anesthetic support for ophthalmic operations are: 1) ensuring the immobility of the eyeball; 2) maintaining constant intraocular pressure; 3) prevention...
Features associated with child anesthesia
27259
0
0
...child. Therefore, it is advisable for a caregiver (eg, parent, nurse, other physician) to remain with the child during transport to the operating room and induction of anesthesia. Such accompaniment is very reassuring to a child, especially one who has already undergone a previous operation (for example, during an ophthalmological examination performed under general anesthesia after a surgery...
Features of anesthesia in maxillofacial surgery, otorhinolaryngology and ophthalmology
17741
0
0
... the pharynx and larynx can enlarge and lead to critical airway obstruction, making reintubation extremely difficult. 2. Anesthesia in otorhinolaryngology When performing surgical interventions in patients with pathology of the maxillofacial region, the most important condition for ensuring the safety of anesthesia is the reliable maintenance of airway patency and prevention...
How to put eye drops correctly?
contact lenses, it is better to remove them. To make instillation more convenient, you should pull back the lower eyelid with your finger, roll your eyes and drop the required amount of the drug into the space that forms between the pulled eyelid and the eyeball. After this, it is recommended to close your eyes for a few minutes. This will help enhance the effectiveness of the drops.
Some medications that are used to treat conjunctivitis may have a negative reaction after instillation. This is explained by the fact that due to the inflammatory process the mucous membrane becomes more sensitive. For this reason, she reacts sharply to the active components of the drug. Sometimes side effects may occur, for example: stinging, burning, pain in the eyes. You just have to endure these unpleasant sensations. In this case, there are no other means of dealing with discomfort. Replacing a drug, even with the permission of an ophthalmologist, does not always guarantee the absence of unpleasant sensations during instillation. Usually this is not due to the quality of the drops, but to the sensitivity of the mucous membrane of the eye.
Side effects
Patients often believe that eye drops do not have a strong effect on the body, and therefore do not have side effects. In fact, this is not so. Like any other medicines, ophthalmic drugs can also have their side effects and options for individual intolerance.
Formulations containing steroids or antibiotics can cause discomfort in the form of tingling or pinching for some time, from one to five minutes. More often, only on first use. However, if these sensations do not disappear for a long time, and appear every time the composition is used, you should consult a doctor for advice. In some cases, the sensitivity of vision may change, which must be reported to the attending physician. When using drugs with chloramphenicol, a sore throat, chills, and minor ruptures of the blood vessels in the eye may occur. An allergic reaction in the form of a rash, itching, swelling of the eyelids, quite severe dizziness and shortness of breath is also possible.
Formulations with prostaglandin analogues may cause a temporary change in the color of the iris, as well as the color of the skin of the eyelids. There may also be a change in eyelash growth, slight tingling, slight or very noticeable blurring of vision. In some cases, severe redness of the eyes, severe itching or burning occurs.
Side effects of using beta blockers include low blood pressure, decreased heart rate, high fatigue, shortness of breath, and in rare cases, a significant decrease in libido and depression. Alpha receptor agonists promote burning, tingling, and cause fatigue, migraines, and drowsiness. Sometimes there is severe dryness in the mouth and nose. High risks of developing an allergic reaction. Carbonic anhydrase inhibitors can also cause tingling, burning, and other discomfort in the eye area.
Lubricating eye drops are characterized by side effects such as pain in the eyes, decreased visual function, and redness. If such side effects do not go away within more than three days, you should consult a doctor.
Is it possible to choose eye drops yourself?
You cannot choose eye drops yourself. Their selection should only be carried out by an ophthalmologist. After collecting information about the patient’s complaints and general health, for example, the presence of chronic diseases, the doctor will be able to prescribe a drug to treat conjunctivitis. It becomes clear what to put in the patient’s eyes, but not everyone follows the ophthalmologist’s recommendations.
It often happens that a person visits a pharmacy, consults with a pharmacist, and chooses other eye drops. This is often due to the lower cost of the drug. Some patients ask the pharmacist which similar products have the same active ingredient and purchase a similar drug. This should not be done, since the main substance is usually not the only one included in the composition of the drops.