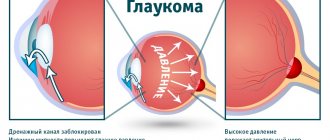
What is glaucoma
Glaucoma is a disease that damages the optic nerve. In this case, blind spots appear in the periphery. Damage to nerve fibers is irreversible.
The pathological condition goes undetected for a long time. The first signs appear in the later stages of the disease, when visual perception deteriorates.
The main reason is increased intraocular pressure, which is caused by an imbalance between the formation and outflow of fluid inside the eye. It is a clear liquid formed by the ciliary body that contains nutrients and immune defense substances. It passes through the chamber angle, an anatomical structure consisting of the cornea and iris.
If more water is produced than can drain, the pressure in the anterior chamber of the eye increases. Increased intraocular pressure leads to poor circulation of nerve cells, resulting in their damage.
Symptoms of the disease:
- headache;
- scotomas;
- the field of view narrows in an arc from the periphery inward;
- rainbow circles around bright light sources;
- problems with coordination and orientation in space.
A sudden attack of glaucoma leads to a sharp increase in IOP, interrupts the blood supply to the eye and causes blindness. Intraocular pressure and therefore the blood supply to nerve cells must be normalized as soon as possible.
Characteristics of stage II
Advanced (or II) stage of glaucoma also has characteristic signs that are determined by examining the visual field. In this case, the peripheral visual field narrows by more than 10°. The process can develop from the nasal side or spread concentrically.
The patient may complain of a gradual limitation of the field of vision, which moves from the area located on the side of the nose to the central part. This process is caused by trophic disorders in the optic nerve, which occur as a result of an increase in intraocular pressure.
Increased pressure prevents normal blood circulation in the vessels of the eye. What is the first thing that affects the optic nerve? Due to disruption of cellular metabolism and lack of oxygen, cellular apoptosis increases. Some cells die and are not restored.
With glaucoma, vision narrows by 10° in the peripheral visual field
Another recognized theory for the occurrence of glaucomatous optic neuropathy is the theory of mechanical influence. As a result of the pressure of the intraocular fluid, the cribriform plate bends in the prelaminar part of the optic nerve head. A bundle of nerve fibers passes through the plate. When the plate bends, deformation of the lattice tubules occurs, mechanical compression of the axons of large M-cells of the ganglion and, as a result, disruption of their conductivity.
Stage II of glaucoma is characterized by the onset of atrophy of nerve fibers at the level of the cribriform plate. When the transport of nutrients to the axons of nerve cells - from the terminals to the body - decreases and then completely stops, the mechanism of programmed death (apoptosis) is activated. As a result, toxic substances are released that affect an increasing number of nearby cells, expanding the area of death.
With the progression of central escalation, which tends to the edge of the optic disc, a gradual and uneven narrowing of the neural ring is observed. Glaucomatous scotoma is noted - an increase and deformation of the border of the blind spot, with which arcuate scotomas gradually merge. At stage II of glaucoma development, the processes continue to increase:
- disturbances in the outflow of intraocular fluid;
- intraocular pressure increases, reaching levels above tolerant for the optic nerve;
- the processes of hypoxia and ischemia of the tissues of the optic nerve head progress;
- glaucomatous optic neuropathy manifests itself;
- apoptosis of retinal ganglion cells begins.
The division of the course of the pathological process into stages II and III is arbitrary, since their severity varies significantly, depending on the individual characteristics and form of the glaucomatous process. However, stage II has a direct impact on the formation of stage III.
A healthy eye differs from a patient with glaucoma in the pathological processes in it
What is characteristic of stage III?
The advanced (or III) stage of the optic nerve degradation process continues the process of the previous stage. The processes of destruction of cells of the optic nerve head continue to increase, the deflection of the cribriform plate increases and, accordingly, the escavation of the optic disc increases, approaching the edge of the disc. The neural ring completely disappears—marginal subtotal escavation is noted.
The zone of decreased peripheral vision expands, reaching in individual segments a border only 15° distant from the point of fixation (the highest point of visual acuity, located at the top of the “hill” of vision). The field narrows especially quickly in the upper nasal segment. If at first this process stopped when intraocular pressure normalized, then stage III glaucoma is characterized by an increase in the rate of vision loss. The patient's vision is as if he is looking through a gradually narrowing tube.
Advanced glaucoma is expressed in an increase in the size of the eyeball. Upon examination, retinal vessels sharply bend over the edge of the optic disc are visible. Retinal edema reaches an extreme degree, which is noticeable by the expansion of the diameter of the blind spot. Destruction of ganglion cells and discoloration of the optic disc continue. The disc acquires a pronounced gray and sometimes slate gray tint (normally it is pink). The vascular bundle is displaced. The temporal edge of the optic disc becomes steeper and more “undermined.”
Degrees
Conventionally, there are 4 stages of glaucoma. When determining them, the condition of the optic nerve is assessed.
Initial degree
Peripheral vision does not change. With this type of glaucoma there are slight changes in the paracentral parts of the visual field. At the initial stage there are no signs. The excavation of the optic nerve head is widened.
Advanced degree
This type of pathology is characterized by a narrowing of the paracentral region by 10 degrees in the upper or lower nasal quadrant. The depression at the site where the nerve enters the connective tissue is marginal in nature and expanded.
Advanced stage
The boundaries of the field of visual perception are narrowed by 15 degrees or more. Subtotal excavation of the optic nerve disc is observed.
Such changes occur after several years of disease development. The optic nerve is significantly damaged, and certain visual areas are lost. Lack of treatment threatens blindness.
Terminal stage
It is impossible to preserve visual perception. Terminal glaucoma is incurable. Atrophy of the optic nerve is observed, pain appears, which is bursting in nature and spreads to the entire area of the head.
This stage is characterized by complete loss of visual acuity and field of vision. The patient only has light perception. That is, the visual analyzer perceives light and various degrees of its brightness, but does not see objects, faces and colors.
Classification of glaucoma
Glaucoma classification The necessity to make alterations in the glaucoma classification passed in Russian federations in accordance with modern data was resolved on the VII congress of ophthalmologist of Russia. The authors propose to classify glaucoma by the origin – on primary, secondary and associated with defects of ontogenesis; by the patient age – on congenital, infant, juvenile and adult glaucoma; by the mechanism of IOP increasing – on closure angle, open angle, mixed, with goniodisgenesis, pretrabecular block and intrascleral block; by the IOP level – on hypertensive and normotensive; by the optic nerve head damage – on beginning, advanced, far advanced and terminal; by the type of disease trend – on stabilized and unstabilized. All clinical glaucoma forms are united into the following groups: (1) primary congenital glaucomas, (2) congenital glaucomas associated with defects of ontogenesis, (3) primary open angle glaucomas of adults, (4) primary closure angle glaucomas, (5) secondary glaucomas. The resolution of the VII Congress of Russian Ophthalmologists noted significant progress in the study of the pathogenesis and clinical picture of glaucoma and proposed changes to its classification. The purpose of this article is to outline our approach to this problem. Background The first classification of glaucoma, proposed by A. Graefe in 1857, was based on clinical symptoms [11]. He divided glaucoma into acute inflammatory and chronic. Graefe also described amaurosis with excavation of the optic nerve, which Donders (1862) later called simple glaucoma. Graefe divided the course of the glaucomatous process into 4 stages: prodromal, developed, absolute and degenerative. In subsequent years, the Graefe–Donders classification was changed several times. It is not possible to consider all proposed classification schemes here. Two main trends can be distinguished in them: a gradual transition from classifications of a clinical nature to pathogenetic ones and from a static scheme to a dynamic one. The priority of the pathogenetic classification of glaucoma belongs to O. Barkan (1938), who, based on the results of gonioscopy, identified two types of glaucoma - narrow-angle and wide-angle [8]. Subsequently, Barkan's classification was terminologically changed: glaucoma was divided into closed-angle and open-angle. B. Becker and R. Shaffer (1961) based their classification [9] on local mechanisms responsible for increasing intraocular pressure (IOP). The authors divide glaucoma (primary and secondary) into 4 main groups: closed angle, open angle, combined and congenital (with dysgenesis of the anterior chamber angle). The most complete transition from a static classification of glaucoma to a dynamic one was carried out by B.L. Polyak [5]. His classification, approved by the All-Union Conference on Glaucoma in 1952, provided for the division of the glaucomatous process not only by clinical form (simple and congestive), but also by the stage of its development (by changes in the visual field and optic disc) and the state of IOP compensation. The main advantage of the classification of B.L. The Pole is that with its help you can monitor the dynamics of the glaucomatous process and make timely adjustments to treatment prescriptions. On the instructions of the board of the All-Union Society of Ophthalmologists A.P. Nesterov and A.Ya. Bunin [3] developed a new classification of primary glaucoma, which was approved by the III All-Russian Congress of Ophthalmologists (1975), the Plenum of the Board of the All-Union Scientific Society of Ophthalmologists (1976) and approved by the USSR Ministry of Health. This classification is well known to ophthalmologists in Russia and the CIS countries, who use it in their practice. The original version of the pathogenetic classification of glaucoma was proposed by M.M. Krasnov [2] in 1970. The author distinguishes hypersecretory and retention forms of primary glaucoma. The retention form, associated with a violation of the outflow of aqueous humor from the eye, can be of three types: angular, trabecular and intrascleral. S.N. Fedorov [7] in 1981 described 3 types of primary open-angle glaucoma: ciliary, ciliouveal and papillary. In the first of them, the lesion is localized in the posterior long and anterior ciliary arteries. In such cases, the development of the glaucomatous process is accompanied by pronounced dystrophic changes in the iris and ciliary body. Ciliouveal glaucoma is a consequence of damage to both the posterior long and posterior short ciliary arteries. The symptoms are the same, but changes in the choroid are added, and atrophy of the optic disc can continue even after normalization of IOP. In papillary glaucoma, the microvascular network that feeds the optic disc is affected, and atrophy of the optic disc develops at a normal IOP level. R. Ritch, M. B. Shields, and Th. Krupin [12] in the three-volume monograph “The Glaucomas” (USA, 1996), classify glaucoma into 8 groups, including: 1) congenital, 2) open-angle, 3) closed-angle, 4) associated with other developmental defects, 5) associated with other eye diseases, 6) associated with systemic diseases and medications, 7) associated with inflammatory processes in the eye and associated with the consequences of ophthalmic surgery. The authors believe that there are tension-dependent and tension-independent forms of glaucoma. The latter includes some cases of glaucoma with normal pressure. The glaucomatous process goes through 5 stages: 1 - initial changes (apparently of an etiological nature), 2 - obstruction of the outflow pathways of aqueous humor, 3 - increased IOP, 4 - optic nerve atrophy, 5 - progressive loss of the visual field. Optic nerve atrophy can be caused by vascular or structural abnormalities in the optic nerve head. The European Glaucoma Society (EGS), in a collective guideline published in 1998 [10], identifies 5 main groups of the glaucomatous process: 1 - congenital forms, 2 - primary and (3) - secondary open-angle glaucoma, (4) primary and (5) secondary angle-closure glaucoma. The EGS classification does not indicate the stage and degree of compensation of the glaucomatous process. An interesting classification of open-angle glaucoma was developed by V.V. Volkov in 2001 [1]. The author identifies 3 clinical forms of glaucoma: with increased IOP; with reduced tissue cerebrospinal fluid pressure in the optic nerve; with weakening of the strength of the lattice membrane of the sclera in myopic disease, senile involution and other dystrophies. The stages of glaucoma (from preglaucoma to the terminal stage) are diagnosed according to the state of the optic disc and visual field, and the state of stabilization and destabilization is determined depending on the dynamics of retinal photosensitivity in the central visual field, the magnitude of fluctuations, the number of scotomas with automatic threshold perimetry, as well as changes in optic nerve. Classification V.V. Volkova is based on many years of research by the author and his colleagues. It deserves a positive assessment, but can hardly be recommended for widespread use in the practical work of clinics and hospitals due to its complexity. The classification proposed in 2000 by E.I. Sidorenko [6] aims to eliminate the existing significant differences in classification schemes and terminology of pediatric and adult ophthalmology. Principles for constructing a new classification of glaucoma • The classification should include all types and forms of glaucomatous eye lesions, and not just primary adult glaucoma. • The classification will be used not only in specialized centers, but also in eye offices of district clinics. Therefore, it should not be overly complex. • Classification cannot be based on assumptions and should be based only on currently accepted approaches and facts. • The new classification should include the positive aspects of previous classifications. Terminology The term “glaucoma” unites a large group of eye diseases with different etiologies, but having a number of common features in pathogenesis, clinical picture and treatment methods. Glaucoma is characterized by an increase in intraocular pressure (IOP) beyond the tolerant level for the optic nerve (TVOP), the development of glaucomatous optic neuropathy with subsequent atrophy (with excavation) of the optic nerve head (ONH) and the occurrence of typical visual field defects. It should be noted that TVGD may be below the upper limit of statistically normal IOP under the influence of unfavorable factors (ischemia and hypoxia of the ONH, structural changes in the lamina cribrosa of the sclera). Basic classification features Glaucoma is classified by origin - primary, secondary and combined with developmental defects of the eye or other body structures, by the age of the patient - into congenital, infantile, juvenile and adult glaucoma, by the mechanism of increasing IOP - into open-angle, closed-angle, with angle dysgenesis anterior chamber, with a pretrabecular block and with a peripheral block, according to the level of IOP - into hypertensive and normotensive, according to the degree of ONH damage - into initial, developed, advanced and terminal, according to the course of the disease - into stable and unstabilized. Primary and secondary glaucoma Certain difficulties arise when distinguishing between primary and secondary glaucoma. In primary glaucoma, pathogenic processes that occur in the APC, the drainage system of the eye or in the ONH, preceding the onset of the disease, do not have independent significance. They represent only the initial stage of the pathogenetic mechanism of glaucoma. In secondary glaucoma, the pathogenetic mechanisms of the glaucoma process are caused by independent diseases. They do not always cause glaucoma, but only in some cases. Thus, secondary glaucoma is a side and unnecessary consequence of other diseases [4]. Main types of glaucoma All the variety of glaucoma processes is combined into 5 main groups: congenital primary glaucoma, congenital glaucoma combined with other developmental defects, primary open-angle glaucoma (POAG), primary angle-closure glaucoma (PACG), secondary glaucoma. Congenital primary glaucoma Symptoms of glaucoma may appear soon after birth or be preceded by a long latent period. In this regard, congenital, infantile and juvenile primary glaucoma is distinguished. Primary congenital glaucoma (PIG or hydrophthalmos) manifests itself in a child under 3 years of age, recessive inheritance (sporadic cases are possible), pathomechanism – dysgenesis of the anterior chamber angle (ACA) and increased IOP, clinical symptoms – photophobia, lacrimation, blepharospasm, increase in the size of the eyeball , swelling and increase in the size of the cornea, excavation of the optic disc. Primary infantile glaucoma (PIG) occurs in children aged 3 to 10 years, the inheritance and pathomechanisms are the same as those of PIG. IOP is increased, the size of the cornea and eyeball are not changed, the excavation of the optic disc increases as glaucoma progresses. Primary juvenile glaucoma (PJG) occurs between the ages of 11 and 35 years, heredity is associated with disorders of chromosome 1 and TIGR, pathomechanisms are trabeculopathy and/or goniodysgenesis, increased IOP, changes in the optic disc and visual functions of the glaucomatous type. Combined congenital glaucoma Glaucoma can be combined with other congenital anomalies: microcornea, sclerocornea, aniridia, persistent primary vitreous body, peripheral or central mesodermal dysgenesis (Rieger, Frank-Kamenetsky syndromes, Peters anomaly), homocysteinuria, Marfan syndrome, Marchesani syndrome, Lowe syndrome, Sturge fibromatosis –Weber, neurofibromatosis, chromosomal disorders. Primary open-angle glaucoma This group includes the following nosological forms. Simple primary open-angle glaucoma (POAG) occurs over the age of 35 years, the pathomechanism is trabeculopathy and functional canalicular block, increased IOP, changes in the optic disc, retina and visual functions characteristic of glaucoma. Exfoliative open-angle glaucoma (EOAG) is associated with (pseudo)exfoliation syndrome, develops in advanced or senile age, and is characterized by deposits of exfoliative material in the anterior segment of the eye, trabeculopathy, canalicular block, increased IOP and glaucomatous changes in the optic disc, retina and visual function. Pigmentary glaucoma (PG) develops in young and middle ages in individuals with pigment dispersion syndrome, often combined with a simple form of POAG; spontaneous stabilization of the glaucomatous process is possible. Normal pressure glaucoma (NTG) occurs over the age of 35 years, IOP is within normal values, but the level of individual TVGD is reduced (pseudonormal pressure glaucoma according to V.V. Volkov). Changes in the optic disc, retina and visual functions characteristic of glaucoma. The disease is often combined with vascular dysfunction. Primary angle-closure glaucoma The following pathogenetic forms of primary angle-closure glaucoma (PACG) are distinguished. Angle-closure glaucoma with pupillary block (PAG-1) occurs in middle-aged or elderly people, occurs in the form of acute or subacute attacks with a subsequent transition to a chronic form due to the formation of goniosynechia. Risk factors: hypermetropia, small anterior chamber, narrow AP, large lens, thin iris root. Pupillary block, which occurs when the pupil is moderately dilated, leads to protrusion of the iris root and blockade of the apical system. Iridectomy stops the attack and prevents both the occurrence of new attacks and the transition of PACG to a chronic form. Angle-closure glaucoma with a flat iris (PACG-2) also has an acute and then chronic course. Risk factors, in addition to those noted above, are a thickened iris root, anterior position of the ciliary crown and the base of the iris. Seizures occur as a result of blockade of the UPC by the thickened basal fold of the iris when the pupil dilates. Iridectomy does not prevent the development of attacks in PACG-2. “Creeping” angle-closure glaucoma (PACG-3) occurs without attacks, as a chronic disease in which the periphery of the iris fusions with the anterior wall of the APC. The reasons for the obliteration of the CPC have not been established. Angle-closure glaucoma with vitreolenticular block (PAG-4) can be primary in nature, but more often develops after antiglaucomatous operations. The risk factors are the same as for PACG-2, but the anatomical features are more pronounced. Aqueous humor enters not only the posterior chamber, but into the vitreous body, the iridolenticular diaphragm moves anteriorly, and a vitreolenticular block appears at the level of the ciliary crown and UPC. The disease has the character of a permanent acute attack (glaucoma maligna). Secondary glaucoma Secondary glaucoma has a wide variety of clinical forms. Depending on the etiology, they can be combined into 7 main groups [5]. Inflammatory and post-inflammatory glaucoma: • caused by scleritis and keratitis • postveal Phacogenic glaucoma: • phacotopic • phacomorphic • phacolytic Vascular glaucoma: • neovascular • phlebohypertensive Dystrophic glaucoma: • with retinal detachment • with iridocorneal endothelial syndrome • hemolytic Traumatic glaucoma : • contusion • wound • burns • radiation • postoperative Neoplastic glaucoma • with intraocular tumors • with orbital tumors and endocrine exophthalmos Glaucoma caused by corticosteroids. Stages of glaucoma The division of the continuous glaucoma process into 4 stages is conditional. In the diagnosis, stages are designated by Roman numerals from I – initial to IV – terminal. In this case, the state of the visual field and optic disc are taken into account. Stage I (initial) - the boundaries of the visual field are normal, but there are slight changes in the paracentral parts of the visual field. The excavation of the optic disc is expanded, but does not reach the edge of the disc. Stage II (developed) – pronounced changes in the visual field in the paracentral region in combination with its narrowing by more than 10° in the upper and/or lower nasal segments, excavation of the optic disc is of a marginal nature. Stage III (advanced) – the border of the visual field is concentrically narrowed, and in one or more segments it is located less than 15° from the point of fixation, marginal subtotal excavation of the optic disc. Stage IV (terminal) – complete loss of vision or preservation of light perception with incorrect projection. Sometimes a small island of the visual field is preserved in the temporal sector. Level of intraocular pressure When making a diagnosis, the following gradations of IOP level are used: A – IOP within normal values (Po < 22 mm Hg), B – moderately increased IOP (Po < 33 mm Hg) and C – high pressure (Po > 32 mmHg). Dynamics of the glaucoma process There are stabilized and unstabilized glaucoma. In the first case, with long-term observation (at least 6 months), no deterioration in the state of the visual field and optic disc is detected, in the second, such changes are recorded during repeated studies. When assessing the dynamics of the glaucomatous process, the level of IOP and its correspondence to the target pressure are also taken into account.
The authors propose to classify glaucoma by the origin – on primary, secondary and associated with defects of ontogenesis; by the patient age – on congenital, infant, juvenile and adult glaucoma; by the mechanism of IOP increasing – on closure angle, open angle, mixed, with goniodisgenesis, pretrabecular block and intrascleral block; by the IOP level – on hypertensive and normotensive; by the optic nerve head damage – on beginning, advanced, far advanced and terminal; by the type of disease trend – on stabilized and unstabilized. All clinical glaucoma forms are united into the following groups: (1) primary congenital glaucomas, (2) congenital glaucomas associated with defects of ontogenesis, (3) primary open angle glaucomas of adults, (4) primary closure angle glaucomas, (5) secondary glaucomas. The resolution of the VII Congress of Russian Ophthalmologists noted significant progress in the study of the pathogenesis and clinical picture of glaucoma and proposed changes to its classification. The purpose of this article is to outline our approach to this problem. Background The first classification of glaucoma, proposed by A. Graefe in 1857, was based on clinical symptoms [11]. He divided glaucoma into acute inflammatory and chronic. Graefe also described amaurosis with excavation of the optic nerve, which Donders (1862) later called simple glaucoma. Graefe divided the course of the glaucomatous process into 4 stages: prodromal, developed, absolute and degenerative. In subsequent years, the Graefe–Donders classification was changed several times. It is not possible to consider all proposed classification schemes here. Two main trends can be distinguished in them: a gradual transition from classifications of a clinical nature to pathogenetic ones and from a static scheme to a dynamic one. The priority of the pathogenetic classification of glaucoma belongs to O. Barkan (1938), who, based on the results of gonioscopy, identified two types of glaucoma - narrow-angle and wide-angle [8]. Subsequently, Barkan's classification was terminologically changed: glaucoma was divided into closed-angle and open-angle. B. Becker and R. Shaffer (1961) based their classification [9] on local mechanisms responsible for increasing intraocular pressure (IOP). The authors divide glaucoma (primary and secondary) into 4 main groups: closed angle, open angle, combined and congenital (with dysgenesis of the anterior chamber angle). The most complete transition from a static classification of glaucoma to a dynamic one was carried out by B.L. Polyak [5]. His classification, approved by the All-Union Conference on Glaucoma in 1952, provided for the division of the glaucomatous process not only by clinical form (simple and congestive), but also by the stage of its development (by changes in the visual field and optic disc) and the state of IOP compensation. The main advantage of the classification of B.L. The Pole is that with its help you can monitor the dynamics of the glaucomatous process and make timely adjustments to treatment prescriptions. On the instructions of the board of the All-Union Society of Ophthalmologists A.P. Nesterov and A.Ya. Bunin [3] developed a new classification of primary glaucoma, which was approved by the III All-Russian Congress of Ophthalmologists (1975), the Plenum of the Board of the All-Union Scientific Society of Ophthalmologists (1976) and approved by the USSR Ministry of Health. This classification is well known to ophthalmologists in Russia and the CIS countries, who use it in their practice. The original version of the pathogenetic classification of glaucoma was proposed by M.M. Krasnov [2] in 1970. The author distinguishes hypersecretory and retention forms of primary glaucoma. The retention form, associated with a violation of the outflow of aqueous humor from the eye, can be of three types: angular, trabecular and intrascleral. S.N. Fedorov [7] in 1981 described 3 types of primary open-angle glaucoma: ciliary, ciliouveal and papillary. In the first of them, the lesion is localized in the posterior long and anterior ciliary arteries. In such cases, the development of the glaucomatous process is accompanied by pronounced dystrophic changes in the iris and ciliary body. Ciliouveal glaucoma is a consequence of damage to both the posterior long and posterior short ciliary arteries. The symptoms are the same, but changes in the choroid are added, and atrophy of the optic disc can continue even after normalization of IOP. In papillary glaucoma, the microvascular network that feeds the optic disc is affected, and atrophy of the optic disc develops at a normal IOP level. R. Ritch, M. B. Shields, and Th. Krupin [12] in the three-volume monograph “The Glaucomas” (USA, 1996), classify glaucoma into 8 groups, including: 1) congenital, 2) open-angle, 3) closed-angle, 4) associated with other developmental defects, 5) associated with other eye diseases, 6) associated with systemic diseases and medications, 7) associated with inflammatory processes in the eye and associated with the consequences of ophthalmic surgery. The authors believe that there are tension-dependent and tension-independent forms of glaucoma. The latter includes some cases of glaucoma with normal pressure. The glaucomatous process goes through 5 stages: 1 - initial changes (apparently of an etiological nature), 2 - obstruction of the outflow pathways of aqueous humor, 3 - increased IOP, 4 - optic nerve atrophy, 5 - progressive loss of the visual field. Optic nerve atrophy can be caused by vascular or structural abnormalities in the optic nerve head. The European Glaucoma Society (EGS), in a collective guideline published in 1998 [10], identifies 5 main groups of the glaucomatous process: 1 - congenital forms, 2 - primary and (3) - secondary open-angle glaucoma, (4) primary and (5) secondary angle-closure glaucoma. The EGS classification does not indicate the stage and degree of compensation of the glaucomatous process. An interesting classification of open-angle glaucoma was developed by V.V. Volkov in 2001 [1]. The author identifies 3 clinical forms of glaucoma: with increased IOP; with reduced tissue cerebrospinal fluid pressure in the optic nerve; with weakening of the strength of the lattice membrane of the sclera in myopic disease, senile involution and other dystrophies. The stages of glaucoma (from preglaucoma to the terminal stage) are diagnosed according to the state of the optic disc and visual field, and the state of stabilization and destabilization is determined depending on the dynamics of retinal photosensitivity in the central visual field, the magnitude of fluctuations, the number of scotomas with automatic threshold perimetry, as well as changes in optic nerve. Classification V.V. Volkova is based on many years of research by the author and his colleagues. It deserves a positive assessment, but can hardly be recommended for widespread use in the practical work of clinics and hospitals due to its complexity. The classification proposed in 2000 by E.I. Sidorenko [6] aims to eliminate the existing significant differences in classification schemes and terminology of pediatric and adult ophthalmology. Principles for constructing a new classification of glaucoma • The classification should include all types and forms of glaucomatous eye lesions, and not just primary adult glaucoma. • The classification will be used not only in specialized centers, but also in eye offices of district clinics. Therefore, it should not be overly complex. • Classification cannot be based on assumptions and should be based only on currently accepted approaches and facts. • The new classification should include the positive aspects of previous classifications. Terminology The term “glaucoma” unites a large group of eye diseases with different etiologies, but having a number of common features in pathogenesis, clinical picture and treatment methods. Glaucoma is characterized by an increase in intraocular pressure (IOP) beyond the tolerant level for the optic nerve (TVOP), the development of glaucomatous optic neuropathy with subsequent atrophy (with excavation) of the optic nerve head (ONH) and the occurrence of typical visual field defects. It should be noted that TVGD may be below the upper limit of statistically normal IOP under the influence of unfavorable factors (ischemia and hypoxia of the ONH, structural changes in the lamina cribrosa of the sclera). Basic classification features Glaucoma is classified by origin - primary, secondary and combined with developmental defects of the eye or other body structures, by the age of the patient - into congenital, infantile, juvenile and adult glaucoma, by the mechanism of increasing IOP - into open-angle, closed-angle, with angle dysgenesis anterior chamber, with a pretrabecular block and with a peripheral block, according to the level of IOP - into hypertensive and normotensive, according to the degree of ONH damage - into initial, developed, advanced and terminal, according to the course of the disease - into stable and unstabilized. Primary and secondary glaucoma Certain difficulties arise when distinguishing between primary and secondary glaucoma. In primary glaucoma, pathogenic processes that occur in the APC, the drainage system of the eye or in the ONH, preceding the onset of the disease, do not have independent significance. They represent only the initial stage of the pathogenetic mechanism of glaucoma. In secondary glaucoma, the pathogenetic mechanisms of the glaucoma process are caused by independent diseases. They do not always cause glaucoma, but only in some cases. Thus, secondary glaucoma is a side and unnecessary consequence of other diseases [4]. Main types of glaucoma All the variety of glaucoma processes is combined into 5 main groups: congenital primary glaucoma, congenital glaucoma combined with other developmental defects, primary open-angle glaucoma (POAG), primary angle-closure glaucoma (PACG), secondary glaucoma. Congenital primary glaucoma Symptoms of glaucoma may appear soon after birth or be preceded by a long latent period. In this regard, congenital, infantile and juvenile primary glaucoma is distinguished. Primary congenital glaucoma (PIG or hydrophthalmos) manifests itself in a child under 3 years of age, recessive inheritance (sporadic cases are possible), pathomechanism – dysgenesis of the anterior chamber angle (ACA) and increased IOP, clinical symptoms – photophobia, lacrimation, blepharospasm, increase in the size of the eyeball , swelling and increase in the size of the cornea, excavation of the optic disc. Primary infantile glaucoma (PIG) occurs in children aged 3 to 10 years, the inheritance and pathomechanisms are the same as those of PIG. IOP is increased, the size of the cornea and eyeball are not changed, the excavation of the optic disc increases as glaucoma progresses. Primary juvenile glaucoma (PJG) occurs between the ages of 11 and 35 years, heredity is associated with disorders of chromosome 1 and TIGR, pathomechanisms are trabeculopathy and/or goniodysgenesis, increased IOP, changes in the optic disc and visual functions of the glaucomatous type. Combined congenital glaucoma Glaucoma can be combined with other congenital anomalies: microcornea, sclerocornea, aniridia, persistent primary vitreous body, peripheral or central mesodermal dysgenesis (Rieger, Frank-Kamenetsky syndromes, Peters anomaly), homocysteinuria, Marfan syndrome, Marchesani syndrome, Lowe syndrome, Sturge fibromatosis –Weber, neurofibromatosis, chromosomal disorders. Primary open-angle glaucoma This group includes the following nosological forms. Simple primary open-angle glaucoma (POAG) occurs over the age of 35 years, the pathomechanism is trabeculopathy and functional canalicular block, increased IOP, changes in the optic disc, retina and visual functions characteristic of glaucoma. Exfoliative open-angle glaucoma (EOAG) is associated with (pseudo)exfoliation syndrome, develops in advanced or senile age, and is characterized by deposits of exfoliative material in the anterior segment of the eye, trabeculopathy, canalicular block, increased IOP and glaucomatous changes in the optic disc, retina and visual function. Pigmentary glaucoma (PG) develops in young and middle ages in individuals with pigment dispersion syndrome, often combined with a simple form of POAG; spontaneous stabilization of the glaucomatous process is possible. Normal pressure glaucoma (NTG) occurs over the age of 35 years, IOP is within normal values, but the level of individual TVGD is reduced (pseudonormal pressure glaucoma according to V.V. Volkov). Changes in the optic disc, retina and visual functions characteristic of glaucoma. The disease is often combined with vascular dysfunction. Primary angle-closure glaucoma The following pathogenetic forms of primary angle-closure glaucoma (PACG) are distinguished. Angle-closure glaucoma with pupillary block (PAG-1) occurs in middle-aged or elderly people, occurs in the form of acute or subacute attacks with a subsequent transition to a chronic form due to the formation of goniosynechia. Risk factors: hypermetropia, small anterior chamber, narrow AP, large lens, thin iris root. Pupillary block, which occurs when the pupil is moderately dilated, leads to protrusion of the iris root and blockade of the apical system. Iridectomy stops the attack and prevents both the occurrence of new attacks and the transition of PACG to a chronic form. Angle-closure glaucoma with a flat iris (PACG-2) also has an acute and then chronic course. Risk factors, in addition to those noted above, are a thickened iris root, anterior position of the ciliary crown and the base of the iris. Seizures occur as a result of blockade of the UPC by the thickened basal fold of the iris when the pupil dilates. Iridectomy does not prevent the development of attacks in PACG-2. “Creeping” angle-closure glaucoma (PACG-3) occurs without attacks, as a chronic disease in which the periphery of the iris fusions with the anterior wall of the APC. The reasons for the obliteration of the CPC have not been established. Angle-closure glaucoma with vitreolenticular block (PAG-4) can be primary in nature, but more often develops after antiglaucomatous operations. The risk factors are the same as for PACG-2, but the anatomical features are more pronounced. Aqueous humor enters not only the posterior chamber, but into the vitreous body, the iridolenticular diaphragm moves anteriorly, and a vitreolenticular block appears at the level of the ciliary crown and UPC. The disease has the character of a permanent acute attack (glaucoma maligna). Secondary glaucoma Secondary glaucoma has a wide variety of clinical forms. Depending on the etiology, they can be combined into 7 main groups [5]. Inflammatory and post-inflammatory glaucoma: • caused by scleritis and keratitis • postveal Phacogenic glaucoma: • phacotopic • phacomorphic • phacolytic Vascular glaucoma: • neovascular • phlebohypertensive Dystrophic glaucoma: • with retinal detachment • with iridocorneal endothelial syndrome • hemolytic Traumatic glaucoma : • contusion • wound • burns • radiation • postoperative Neoplastic glaucoma • with intraocular tumors • with orbital tumors and endocrine exophthalmos Glaucoma caused by corticosteroids. Stages of glaucoma The division of the continuous glaucoma process into 4 stages is conditional. In the diagnosis, stages are designated by Roman numerals from I – initial to IV – terminal. In this case, the state of the visual field and optic disc are taken into account. Stage I (initial) - the boundaries of the visual field are normal, but there are slight changes in the paracentral parts of the visual field. The excavation of the optic disc is expanded, but does not reach the edge of the disc. Stage II (developed) – pronounced changes in the visual field in the paracentral region in combination with its narrowing by more than 10° in the upper and/or lower nasal segments, excavation of the optic disc is of a marginal nature. Stage III (advanced) – the border of the visual field is concentrically narrowed, and in one or more segments it is located less than 15° from the point of fixation, marginal subtotal excavation of the optic disc. Stage IV (terminal) – complete loss of vision or preservation of light perception with incorrect projection. Sometimes a small island of the visual field is preserved in the temporal sector. Level of intraocular pressure When making a diagnosis, the following gradations of IOP level are used: A – IOP within normal values (Po < 22 mm Hg), B – moderately increased IOP (Po < 33 mm Hg) and C – high pressure (Po > 32 mmHg). Dynamics of the glaucoma process There are stabilized and unstabilized glaucoma. In the first case, with long-term observation (at least 6 months), no deterioration in the state of the visual field and optic disc is detected, in the second, such changes are recorded during repeated studies. When assessing the dynamics of the glaucomatous process, the level of IOP and its correspondence to the target pressure are also taken into account.
Literature 1. Volkov V.V. // Proposals for constructing a classification of open-angle glaucoma. - Oculist. – 2001. – N 1. – P.22–23. 2. Krasnov M.M. // Materials of the symposium on the pathogenesis of primary glaucoma. – M. – 1970. – P. 47–53. 3. Nesterov A.P., Bunin A.Ya. Vestn. Ophthalmol. – 1977. – N 5. – P. 38–43. 4. Nesterov A.P. // Glaucoma. – M. Medicine. – 1995. 5. Polyak B.L. // Vestn. Ophthalmol. – 1952. – N 3. – P. 38–43. 6. Sidorenko E.I.// Klin. Ophthalmol. – 2000. – N 4. – P. 117–119. 7. Fedorov S.N. // Issues of pathogenesis and treatment of glaucoma. M. 1981. – P. 3–7. 8. Barkan O. // Amer. J. Ophthalmol. – 1938. – Vol. 21. – P. 1099 –1007 9. Becker B., Shaffer RN // Diagnosis and Therapy of Glaucoma. Mosby-St. Louis. – 1961 10. European Glaucoma Society // Terminology and Guidelines for Glaucoma. – 1998. – Savona Italy. 11. Graefe A.// Graefes Arch. Ophthalmol. – 1857. – Bd 3. – S. 456. 12. Ritch R., Shields MB, Krupin Th. // The Glaucomas (2nd ed.). – Vol. 2. – Mosby. – St. Louis 1996.
Diagnostics
Only an ophthalmologist is able to determine the presence or absence of a pathological condition and the form of the disease. To do this, a number of diagnostic tests are carried out:
- IOP measurement. Non-contact tonometry is used. It is especially effective when the cornea is thick. The procedure is precise and painless. Anesthetic drops are used.
- If IOP rises and falls throughout the day, several measurements are taken. IOP is determined every 2 hours. This helps determine the rate of progression of the disease.
- Pachymetry is the measurement of the thickness of the cornea. The procedure is recommended for all patients during the initial examination. Corneal thickness does not affect visual perception, but does influence the interpretation of intraocular pressure.
- The field of view is an important part of the examination. The ophthalmologist finds out how much it has worsened from the periphery.
- Optical coherence tomography (OCT) examines the back of the eye using light waves close to the retina. The test is quick, simple and painless; no eye drops are needed. The resulting image is more meaningful than a regular color photograph. Analyzes the size and thickness of the fibers that make up the optic nerve. The measurements are then displayed on a color map. Digital recording of nerve structure makes it easier to find changes in the nerve. Changes can be detected early and treatment adjusted quickly.
Prevention of glaucoma
All methods of preventing glaucoma are aimed at preventing the onset of the disease and slowing down the process of its development.
As a basic measure, it is recommended that people, especially those over 40 years of age, undergo regular examinations by an ophthalmologist. This will allow timely identification of the disease at an early stage and initiation of therapy.
Experts also advise giving up bad habits, following a daily routine, eating right and spending time in the fresh air more often.
A good method of preventing glaucoma is taking eye drops. The drug should be used only as prescribed by a doctor.
Another effective way is glasses.
Treatment
Eye drops
The pathology is treated medicinally with eye drops. Medicines are used at the initial stage of the disease. Eye drops can reduce intraocular pressure and prevent further nerve damage. The medications should be used constantly, according to the regimen prescribed by the ophthalmologist.
Eye drops reduce the formation of fluid or improve its outflow. They prescribe Taufon, Travatan, Arutimol, Xalatan, Okumed, Azopt, Fotil, Normoglaucon and others.
The best are Kosopt, Fotil and Proxocarpin. Medicines have a double effect and a longer therapeutic effect. The drugs are instilled once a day.
Operation - laser treatment
In severe cases, laser procedures can reduce intraocular pressure. At the same time, laser operations are constantly being improved to provide gentle treatment with optimal reduction of IOP and minimal trauma. Therapy is aimed at improving fluid outflow.
In severe cases, an iridotomy is performed. The surgeon makes a small hole in the iris with a laser. Separates the anterior and posterior chambers of the eye from each other.
With laser iridotomy, pressure equalization is created between the two chambers and aqueous humor flow is improved.
Surgical intervention - trabeculotomy, goniotomy, microimplants, canaloplasty
Surgical methods for treating glaucoma are also aimed at improving fluid outflow and reducing intraocular pressure.
Two classic operations, trabeculotomy and goniotomy, are performed more often than others. In this case, an opening is created in the tissues of the chamber angle, where the trabecular meshwork is located, improving outflow.
A new method of surgical treatment of glaucoma is canaloplasty. The catheter is placed in the central drain, the Helmet channel. Keeps the channel open at all times, allowing the drainage system to remove excess fluid.
Microimplants are a new method of treatment that provide fluid outflow. This treatment option reduces the recovery period, comparable to the result of canaloplasty.
Is it possible to recognize the first signs of the disease?
Signs of glaucoma in the early stages are nonspecific and often go unnoticed by the patient. Often, only severe pain with nausea and vomiting, which are characteristic of an acute attack of the disease, or progressive deterioration of vision, force the patient to consult a doctor. Early stage glaucoma is diagnosed much less frequently.
The following symptoms may indicate early glaucoma:
- pain in the area of the eyebrow or eyeball;
- a feeling of unusual hardness of the eyeball when palpated through a closed eyelid;
- deterioration of visual acuity;
- the appearance of “blind spots” before the eyes.
For people whose close relatives suffer from increased IOP, it is important to undergo preventive examinations with an ophthalmologist at least once every six months. This disease (especially some of its forms, for example, juvenile) is associated with genetic mechanisms of inheritance.
Developed
Symptoms
Signs of glaucoma at the second, advanced stage are still minor and invisible to humans .
Intraocular pressure at an advanced stage can be consistently high, reaching 30-40 mm Hg. Art. Sometimes attacks of angle-closure glaucoma occur, accompanied by pain.
Some people report a bursting sensation inside the eye.
How to determine
Developed glaucoma of the 2nd degree is determined not by the pressure inside the eye, but by the fields of vision and changes in the disc . There is a pronounced narrowing of the visual fields on the side of the nose by 10 degrees or more. Such a change can already be detected by conventional perimetry. The area of cattle is increasing. When examining the bottom, an increase in the excavation of the disk is determined, in some places right up to its edge.
Treatment
At an advanced stage, treatment consists of using drops to reduce pressure, most often in combination . To overcome addiction to the drug, the drops are changed every 3 months. Additionally, be sure to use vitamin drops and antioxidants. These drugs slow down nerve death. Surgical treatment according to indications if drops are ineffective, if it is impossible to stabilize the process.
IMPORTANT : If it is not possible to achieve low pressure with possible combinations of drops, then sclerectomy is used: the internal portion of the sclera is removed and the fluid will flow out through the resulting window.
Forecast
The prospects at this stage are still good . The changes in the optic nerve have not yet reached critical levels and with regular treatment the disease stabilizes and does not progress.
What it is
The main criterion for the disease is high intraocular pressure . It is created by a clear liquid - aqueous humor. In healthy eyes, moisture appears and leaves regularly. Her
excess is absorbed into the trabecular meshwork, which is located in the corner in front of the iris. This angle is called the front angle. There is a posterior angle behind the iris, where fluid forms.
In angle-closure glaucoma, fluid remains in the posterior chamber and does not enter the anterior chamber angle due to its closure. The open-angle form differs in its development mechanism - the angle is free, and moisture does not leave due to the pathology of the trabecular meshwork.
Both of these forms go through the same stages in their development, from imperceptible changes to complete blindness. Based on these stages, a classification of the disease has been created. But is it possible to cure glaucoma and at what stage ? We will try to answer this question in detail.
REFERENCE : Glaucoma is treated in specialized clinics by glaucomatologists. But a local physician or general practitioner may suspect the disease during preventive examinations.