1449
0
The choroid of the eye is the posterior part of its choroid, located under the sclera. It is susceptible to various diseases, including the appearance of melanomas. Choroidal melanoma of the eye is the most common primary tumor, developing in most cases accidentally, without any obvious cause.
We will tell you in more detail about what choroidal melanoma is, its symptoms and causes, how it is treated, and what the prognosis for life is after surgery or other tumor removal procedures.
Etiological factors
Most cases of choroidal melanoma are sporadic, that is, caused by one or another mutation of the melanocytic precursor cell, which can give rise to a pathological tumor clone. In addition, there is an assumption about the hereditary cause of this disease. The influence of such a typical provoking factor for skin melanoma as increased insolation for this tumor is also not excluded.
Elderly people are at risk (the average age of tumor manifestation is 60 years). Men get sick a little more often. Those with fair skin and hair, nevi and freckles are prone to developing choroidal melanoma.
Classification
Based on the location of the malignant neoplasm, the following types of melanoma of the visual organ are distinguished:
- Eyelids (high degree of malignancy).
- Conjunctiva (spreads and metastasizes early).
- Choroid (uveal melanoma). Lesions of the iris, ciliary body and choroid are described separately (85%).
Also, ocular melanoma is classified according to the TNM system - taking into account the size of the tumor, metastases to the lymph nodes and other organs.
Melanoma of the century
Malignant eyelid lesions are rare and are provoked by excessive sun exposure. Oncologists are also studying the role of genetic predisposition in the development of this disease. People over 30 years of age get sick; gender does not matter. Melanoma can form from a nevus of the eyelid or appear on unchanged skin.
Patients complain of the appearance of a formation in the eye area, which changes its color or enlarges, and bleeds. In severe cases, the tumor ulcerates. The edges of the formation are uneven, pigmentation is uneven.
Oncologists differentiate eyelid melanoma from nevus and pigmented basal cell carcinoma. The diagnosis is confirmed by histological examination. Treatment is only radical surgery. The eight-year survival prognosis ranges from 93% for superficial melanoma to 33% for deep tumor invasion.
Conjunctival melanoma
Conjunctival melanoma is a disease with a poor prognosis. It occurs in young people (20–30 years old) and even in children. But more often they get sick after 55 years. The appearance of a malignant tumor is caused by the degeneration of nevus cells or acquired melanosis (most often). In 5% of cases, no previous diseases are detected.
The predominant localization is the conjunctiva of the eyeball (in 70% of cases). Usually pigmented, but non-pigmented tumors also occur. More often, conjunctival melanoma looks like a node and grows quickly. Less commonly, it is represented by multiple lesions prone to fusion. Its surface is smooth, shiny, and scattered deposits of pigment are noticeable.
Conjunctival melanoma is surrounded by a network of blood vessels. Over time, ulcers become noticeable on its surface, and the tumor begins to bleed.
This form of the disease is characterized by the elimination of satellites (small tumors). If melanoma is non-pigmented, they are not visible during examination due to their small size. This worsens the prognosis. In 50% of cases, the conjunctival neoplasm spreads to the cornea.
This melanoma is characterized by exophytic growth, so patients complain of blurred vision, sensation of a foreign body in the eye, discomfort, pain, and hemorrhages. The diagnosis is made during examination; radiophosphorus diagnostics and ultrasound are used for confirmation. A biopsy is performed if removal of the eyeball (enucleation) is planned.
Treatment depends on the size of the tumor. This may be partial removal or enucleation. Surgical intervention is complemented by application radiation therapy. The prognosis for five-year survival with combined treatment and the absence of metastases is 95%.
Iris melanoma
This tumor often appears as a node without clear boundaries. Color varies from brown to light pink. Vessels are visible on the uneven surface of the neoplasm. In addition to the nodular form, a mixed form is distinguished. Its growth is planar, and pigment is sprayed around.
If melanoma spreads to the pupil, its shape changes. When the lens grows into the posterior chamber of the eye, it shifts and becomes cloudy; when it grows into the anterior chamber, intraocular pressure increases. Tumor satellites are often found on the iris.
If the tumor is diffuse, persistent intraocular hypertension develops early and is the main symptom. Heterochromia may be observed - different colors of the iris.
A rare asymptomatic form of the tumor is tapioca melanoma. It is characterized by slow growth. Upon examination, the ophthalmologist sees neoplasm vessels, pigment accumulations along the edge of the pupil, nodules on the iris. They can merge. With tapioca melanoma, a hyphema often forms - blood accumulates in the anterior chamber.
Ciliary body melanoma
The tumor rarely affects only the ciliary (ciliary) body; more often, neighboring structures are involved in the process with the formation of iridociliary or cilichoroidal melanoma. There are two forms of neoplasm - non-pigmented and pigmented.
Damage to the ciliary body is characterized by slow growth and absence of symptoms. Hypotonia of the eyeball is sometimes observed. As the tumor grows, the lens shifts and becomes cloudy, causing vision impairment. If it grows into the anterior chamber, the iris becomes folded, the shape of the pupil changes, and light sensitivity decreases. Sometimes the reaction to light is completely absent.
In later stages, glaucoma develops.
Choroidal melanoma
The tumor (uveal melanoma) is presented in two forms - nodular and diffuse. It can be located post-equatorially (more than 50%) and in the equatorial zone. Rare localizations include multicentric and binocular variants.
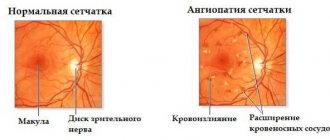
At the beginning of tumor growth, a gray, yellow-brown or green round lesion is detected. As the disease progresses, newly formed vessels grow and pigmentation intensifies. Sweating of fluid from the vessels leads to retinal detachment.
Sometimes the tumor resembles a mushroom - due to the rupture of the vitreous plate, hemorrhages are visible on its surface. The faster eye melanoma grows, the higher the risk of hemorrhages into the surrounding tissue and retina.
Upon examination, the ophthalmologist sees indirect signs of a malignant lesion:
- Rubeosis of the iris (newly formed vessels).
- Retinal detachment.
- Uveitis, scleritis, iridocyclitis.
- Hemorrhage into the vitreous body (hemophthalmos).
- Secondary increase in intraocular pressure.
- Cloudy lens.
- Endophthalmitis (inflammation of internal structures).
- Subatrophy (reduction in the size of the eyeball).
Most often people aged 60 years get sick. A tumor is diagnosed in the following situations:
- Accidentally - during a fundus examination during a routine examination.
- When there is a decrease and distortion of vision, changes in visual fields, complaints of photopsia - flashes of light, shiny balls before the eyes.
- With the development of pain syndrome - due to secondary glaucoma, uveitis.
Morphologically (according to cellular structure), several variants of uveal melanoma are distinguished.
Clinical picture
Patient complaints depend on the size and location of choroidal melanoma, as well as on the presence of accompanying complications, which include: secondary retinal detachment, the appearance of degenerative processes in the retina, and clouding of the lens.
At the initial appointment with an ophthalmologist, a decrease in visual acuity, the appearance of blind spots (scotomas) in front of the eye, and hemianopsia (loss of half the visual field) are usually determined. In case of late treatment, patients complain of pain in the eye (secondary glaucoma), dilation of the vascular network. Also, a pigment spot (extraocular growth of a neoplasm) can be detected on the sclera.
Book a consultation 24 hours a day
+7+7+78
Clinical manifestations and diagnosis
At the initial stage, diagnosis is almost impossible, especially if the choroidal melanoma is located outside the site of greatest acuity in the retina, the so-called macula. Mostly, patients complain of:
- a sharp deterioration in vision, as well as a decrease in its acuity;
- distortion of visible things;
- incorrect perception of shape, color, size, spatial arrangement of objects and phenomena;
- blurred image or pinkish tint;
- “floating” opacities that are black or red in color;
- the appearance of dark spots or a blind spot (scotoma) in the field of vision.
If there is reason to believe that there is any malignant neoplasm, you should urgently consult an ophthalmologist for advice. The doctor collects the patient’s medical history, determines the condition of his eyes, and prescribes all the necessary laboratory or instrumental tests to clarify the diagnosis. First of all, it is necessary to do a general and biochemical blood test, as well as urine.
The ophthalmoscopy method is used to determine whether there are any pathological formations on the surface of the choroid, their size, nature and shape are specified. For melanoma of the choroid of the eye, radioisotope examination, ultrasound and diaphanoscopy are also used, when neoplasms are viewed using a narrow beam of light. The procedure itself takes place in a very darkened room. In addition, it is important to make a timely diagnosis using computed tomography or MRI.
Stages of development of choroidal melanoma
According to the international classification, there are 4 stages of development of this tumor. Criteria for the prevalence of the tumor process:
- T1 - melanoma size 10 mm or less, thickness - 2.5 mm or less.
- T2 - the size of the neoplasm is 10–16 mm, the greatest thickness is 2.5–10 mm.
- T3 - measuring 16 mm and/or thickness more than 10 mm without spreading beyond the eyeball.
- T4 - the largest tumor size is 16 mm and/or thickness more than 10 mm with extension beyond the eyeball.
There are also 4 clinical stages of choroidal melanoma. Each of them is characterized by certain symptoms of the disease:
- The first, so-called “quiet eye” stage, is characterized by the absence of significant clinical manifestations and complaints. Retinal clouding may be present, and visual field defects may also be detected.
- The second stage is characterized by the appearance of pain in the eyes, inflammation, redness of the eyeball, and swelling of the eyelids.
- At the third stage, choroidal melanoma extends beyond the boundaries of the eyeball, exophthalmos is formed, and the sclera loses its integrity.
- The fourth stage is accompanied by generalization of the process. The patient's general condition is deteriorating. Patients complain of severe pain, body weight decreases, and intoxication increases. Metastases of melanoma appear in internal organs: liver, lungs, bones. Damage to one or another organ provokes the appearance of corresponding symptoms. A further decrease in visual acuity, a feeling of veil or fog before the eyes may be detected. These manifestations are caused by bleeding into the vitreous body and clouding of the lens.
Symptoms of the second and third stages of choroidal melanoma are pronounced when the tumor is located in the central or paracentral part of the fundus. Peripheral localization of the tumor is characterized by a long absence of subjective sensations. In this case, melanoma is detected either by chance or at the stage of tumor disintegration and its secondary manifestations.
Diagnostic methods
During primary development, it is quite difficult to determine eye melanoma. An ophthalmoscope can be used to diagnose a tumor. The neoplasm looks like a small nodule on the membrane of the eye.
- the iris of the eye has an uneven contour;
- unusual knots;
- pigmentation.
Stages of development of choroidal melanoma of the eye
Before starting treatment for a patient, doctors determine the stage of tumor development.
There are 5 stages of education:
- 0 – very rarely detected due to very small size;
- 1 – no signs or symptoms are observed, only minor visual defects appear;
- 2 – the tumor develops in the inner part of the eye, without going beyond its apertures, pain is felt and inflammation appears;
- 3 – at this stage, the disease affects the lymphatic system and grows into nearby structures;
- 4 – metastases affect vital organs.
The first 2 stages are operable, and timely treatment leads to complete recovery or clinical remission. The third stage is more serious and not so easy to treat; sometimes repeated surgery is necessary and relapses are common. At the last stage of cancer, the chances of recovery are minimal, but therapy should be continued.
Types of eye melanoma
A classification of choroidal melanoma based on morphological characteristics has been developed. Depending on the cellular structure, the following types of this tumor are distinguished:
- Spindle cell.
- Epithelioid.
- Mixed (mixed melanoma).
- Fascicular.
- Necrotic.
This classification has certain disadvantages, since necrotizing choroidal melanoma is determined clinically, but it is impossible to determine its cellular identity due to extensive necrosis. Fusiform and fascicular types have a similar prognosis. In this regard, it is currently customary to distinguish only 2 types morphologically: spindle cell and epithelioid. The mixed form occupies an intermediate position. Its prognosis depends on the predominance of certain cells. Epithelioid cell melanoma of the choroid is considered to have the least favorable prognosis.
Eye melanoma: photos of the initial stage, treatment and prognosis
Ocular melanoma is a malignant tumor that arises in the vascular tract. Composition: melanin producing cells. The vascular tissue and sclera of the ciliary body are most often affected. The amount of melanin among the constituents is 6%.
Disease code according to the International Classification of Diseases (ICD-10) C43.3. The degree of malignancy depends on the age and location on the eye.
The tumor affects melanocytes (pigment cells), which produce pigment spots that serve as the basis for the formation of the disease.
The first symptom is the appearance of pigment. More often, the disease appears in middle-aged or elderly people. Melanoma is more common in men than women. The fatality rate is 60% or people do not live long.
The danger threatens if prevention is not carried out, drugs are used that reduce the risk of disease progression, or after surgery. Life expectancy is short.
Treatment is carried out by doctors from the field of oncology or ophthalmology, as well as microscopic surgery.
Consequences
But cancer treatments are dangerous and come with consequences. For example, bleeding, cataracts, complete loss of vision, etc. Eye surgery is painful, traumatizes the organ, which will lead to discomfort when blinking or closing the eyes. However, the chance of recovery after surgery is high.
If there is a predisposition to the appearance of a cancerous tumor in the eye, disease prevention is necessary to reduce the risk of the disease. Predisposition factors for the disease include:
- Working outdoors, which involves exposure to dust, small particles, sunlight, or irritation of the retina by light, heat or cold.
- The skin color is too white, as is the hair (or red), the eyes are blue or green.
- The number of moles and birthmarks on the body, which contribute to the appearance of eye tumors, turning into skin cancer.
- Genetic predisposition to ocular melanoma or diseases of this type.
- Number of burns on the skin.
- Aging.
- Leading an unhealthy lifestyle.
- Poor care.
Prevention that prevents eye melanoma
For prevention, you need to carefully observe the processes and changes occurring in the body. After 40 years, a full examination is carried out annually, including an examination of vision and the presence of diseases. In sunny weather, you should protect your eyes by wearing sunglasses with special lenses to prevent ultraviolet radiation.
At the first suspicion of a disease, you should consult a doctor for examination and identification of the disease. New growths should not be ignored. Remember that the more you start the disease, the less chance you will have to recover and avoid death.
To summarize, it is worth noting the following points:
- To be safe and reduce the risk of a tumor, preventive care and an annual examination are carried out.
- If you notice a change in the color of the eye shell, you should be wary and undergo an examination to determine whether it is a malignant neoplasm or not.
- If your fears are confirmed, do not give up. It is necessary to carry out the prescribed treatment to bypass the disease. An operation that is determined by the desired result is suitable for this.
- After 40 years, it is worth observing yourself more often, noting the appearance of moles and spots on the body, which may accompany eye melanoma.
- When the disease appears, it is worth monitoring the progress of the stages of tumor development.
- Do not ignore possible manifestations of the disease.
The main thing is not to forget to monitor your vision, starting from childhood, in order to protect yourself in the future. To do this, you should isolate yourself from things that accompany eye cancer.
Select the city, desired date, click the “find” button and make an appointment without waiting in line:
Source: https://onko.guru/zlo/melanoma-glaza.html
Diagnostics
Considering the clinical features of choroidal melanoma, its diagnosis, especially in the initial stages, presents certain difficulties. In addition to the analysis of patient complaints and clinical and anamnestic data, the results of the following instrumental studies are taken into account:
- Biomicroscopy.
- Ophthalmoscopy.
- Ultrasound examination of the eye.
- Diaphanoscopy, etc.
Choroidal melanoma is a neoplasm with a high risk of metastases. Therefore, when examining a patient, it is also necessary to use methods for diagnosing metastatic foci: ultrasound of the abdominal organs and lymph nodes, lung radiography, CT, MRI.
General information
Choroidal tumors are benign or malignant neoplasms of the choroid of the eyeball. Nevus is the most common benign formation of the organ of vision. The frequency of its detection during ophthalmoscopy is 2%. At the same time, during autopsy this pathology is diagnosed in 6.5-20% of patients.
In females and males, nevi are detected equally. The prevalence of uveal melanoma among all eye pathologies is 5%. The risk of developing this choroidal tumor increases significantly with the age of the patient and after 69 years of age increases by 50 cases every year (per 1 million population).
Choroidal tumors
Treatment options for choroidal melanoma
There are organ-preserving methods of treating this tumor and a surgical method without preserving the eye. In cases where it is not possible to save the eye, enucleation is performed - isolated removal of the eyeball or exenteration - excision of the entire contents of the orbital cavity along with the eyeball.
Indications for enucleation:
- The tumor is of significant size.
- Spread of melanoma to the optic disc.
- Complete absence of visual function.
- Extrabulbar tumor growth.
- Secondary glaucoma.
After removal of the eyeball, an internal prosthesis is implanted and subsequent external prosthetics is performed. These measures not only allow you to achieve a good cosmetic result, but also prevent facial deformation.
Organ-preserving methods of treating choroidal melanoma include:
- Radiation therapy. Depending on the method of delivering radiation, radiation therapy for this disease is carried out by contact or remote methods. Contact radiation, or brachytherapy, is the implantation of radioactive elements near the site of melanoma.
Indications for brachytherapy:
- No signs of decay.
The diameter of the neoplasm is up to 15 mm.
- The distance from the optic disc is at least 2 times the diameter of the disc itself.
- Laser coagulation in combination with thermotherapy. Transpupillary thermotherapy is a type of laser treatment for melanoma using deep local hyperthermia. The method is based on the possibility of deep penetration of infrared radiation through chorioretinal tissue. Transpapillary thermotherapy is an effective independent treatment for small choroidal melanomas (up to 4 mm in diameter).
- Cryodestruction. This method is based on extreme cooling of small melanoma lesions to −78 °C.
Brachytherapy is the most effective method of organ-preserving treatment for choroidal melanoma. Its use can reduce the likelihood of tumor metastases.
As part of systemic treatment, immune therapy is important. Also, when providing care to patients with choroidal melanoma in the later stages, the features of its metastasis are taken into account. This tumor is characterized by isolated liver damage by metastases. In such cases, chemoembolization of this organ is successfully used.
Such a common method of treating skin melanoma as targeted therapy is not used for choroidal melanoma, since this type of tumor does not have specific BRAF mutations.
Prevention
There are no specific measures to prevent choroidal melanoma of the eye. But depending on the stage and location of the tumor, doctors select individual methods and preventive measures. The main rule is regular visits to the ophthalmologist and preventive examination. You should constantly protect your eyes from sunlight. On hot sunny days, try to minimize going outside. Those who care about their health should regularly donate blood for liver enzymes.
But oncologists make some recommendations:
- not in direct sunlight, especially from 3 to 5 o’clock in the afternoon;
- wear sunglasses and protect yourself with special creams that protect the skin from UV rays;
- do not consume harmful substances - alcoholic beverages, drugs and tobacco products;
- engage in an active lifestyle, it strengthens the immune system;
- get a good night's sleep and organize your regular routine;
- eat healthy and balanced foods.
Forecast
The further prognosis of life and active work capacity is influenced by the stage and size of the tumor. According to statistics, the mortality rate for a tumor less than 1 cm is 16%, and for 15 mm it becomes 53%.
- in general diagnostics of the body, an unfavorable sign is the presence of a large number of epithelioid cells, which are detected by magnification. Lymphoid infiltration and loops of blood vessels that close and lead to the tumor;
- a chromosomal abnormality in tumor cells predicts an unfavorable course, survival over a five-year period is 50%;
- the large size of the tumor indicates the presence of complications;
- extrascleral growth of melanoma is a poor prognosis;
- Patients over 60 years of age are more likely to suffer from this type of disease and the mortality rate at this age is higher than in young people.
Similar article - Cleansing using the Ohanyan method
When suffering from choroidal melanoma, patients have a good chance of a full recovery and life. Since the disease in rare cases gives metastases to vital organs. But a large tumor can only be treated through surgery and there is nothing left except removing the eyeball.
Therefore, specialists from any industry unanimously speak about regular diagnostics of the whole body. Today, medical institutions have a large amount of medical equipment that makes it possible to detect any disease in the early stages of development. This allows you to maximize your chances of recovery and future life.
According to statistics, over the past 100 years, the level of disease and mortality due to cancer pathology has increased significantly and is in solid second place, after diseases of the cardiovascular system. And the variety of formations is only acquiring new types. Any part of the body can be susceptible to cancer.
You should be attentive to your own body’s signals and, if you have any symptoms or suspicions of a disease, immediately contact a specialist and undergo all related tests.
Choroidal melanoma is a malignant pigmented tumor of the choroid of the eye (choroid). This tumor is one of the most common intraocular neoplasms. Choroidal melanoma is the main cause of mortality and disability in cancer patients with damage to the organ of vision. The disease can be practically asymptomatic, but at the same time has a high tendency to metastasize, so the problem of identifying it in the initial stages is extremely relevant.
Prognosis for life with choroidal melanoma
Life expectancy for this type of cancer depends on the location and size of the tumor, the patient’s age, the morphology of the tumor, the treatment performed and other features. The five-year survival rate in the initial stages of choroidal melanoma after the use of organ-preserving radical methods is 93%, and the ten-year survival rate is 89%. In later stages, when liver metastases are detected, the median survival is only 4-6 months. For patients with metastatic disease to other organs, the one-year survival rate is 76%.
Book a consultation 24 hours a day
+7+7+78
Prognosis and prevention of choroidal tumors
Specific measures for the prevention of choroidal tumors in ophthalmology have not been developed. All patients with an established diagnosis of a benign or malignant neoplasm of the choroid should be monitored by an ophthalmologist. After surgical treatment, it is periodically necessary to undergo preventive examination by a specialist, limit exposure to the sun, and avoid working at high ambient temperatures.
The prognosis for life and ability to work with a stationary form of nevus is favorable. The progressive variant should be considered a precancerous condition. The most malignant among choroidal tumors is melanoma; the prognosis for life is determined by the stage of development. Choroidal hemangioma is a prognostically favorable disease, but in some patients complete loss of vision is possible.
Diagnosis of uveal melanoma
The following methods are used in the diagnosis of malignant lesions:
- Fundus ophthalmoscopy and biomicroscopy with a dilated pupil.
- Diaphanoscopy, transillumination – for pigmented melanomas. This is a highly informative method, but it gives false-positive results for hemorrhages.
- Fluorescein angiography. The information content of the study is high; a spotty coloration of the neoplasm is determined.
- Ultrasound with Dopplerography. Allows you to confirm the diagnosis and determine the degree of vascularization of the formation.
- CT, MRI.
Before examining the patient, it is necessary to clarify the oncological history; familial uveal melanoma of the eye occurs in 0.37% of cases. Also, a tumor of the choroid is observed in primary multiple cancer, so the diagnosis must be comprehensive.