Causes
According to the method of inheritance, Best's dystrophy is classified as an autosomal dominant type. A gene located on the long arm of chromosome number eleven is directly related to the development of the disease.
It is impossible to identify the disease in advance; it is asymptomatic. In rare cases, patients may complain of problems reading small print, sometimes blurred vision, and metamorphopsia. Especially often, such a pathology is discovered by chance during the next ophthalmological examination.
Pathology that is inherited
More than a century ago, F. Best analyzed identical visual impairments that suffered from several relatives - representatives of the same family. Based on the work done, he concluded that macular degeneration of this type is hereditary.
Today, scientists know that a child inherits pathology from his parents, and the probability of transmitting a defective gene remains even if only the mother or only the father is its carrier (autosomal dominant type of inheritance).
Signs of the disease
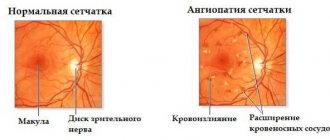
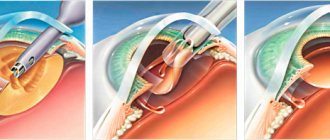
Best's dystrophy occurs due to the accumulation of transudate under the pigment epithelium. Such an accumulation can sometimes reach three times the diameter of the optic nerve head and lead to ophthalmological changes in the macula area of the eye. Depending on the intensity of such changes, it is customary to distinguish certain stages of the development of the disease:
- Previtellifoma stage, when small yellow spots and minimal pigmentation disturbance are found in the macula;
- Vitelliform stage with a vitelliform cyst in the macula;
- The stage of cyst rupture and resorption of its contents;
- Stage of fibroglial scar formation.
In its development, Best's disease does not always strictly go through stages; sometimes slight variations in the manifestations of the disease are possible. Changes, as a rule, are bilateral, asymmetrical. Visual acuity decreases only by the 3rd stage, remaining in the range from 0.02 to 1.0D. Over time, degeneration of the external components of photoreceptors is possible. Without proper adequate treatment, Best's disease can be complicated by the formation of a subretinal membrane and subretinal hemorrhages. In rare cases, this condition can lead to retinal detachment, as well as choroidal sclerosis.
How does pathology affect visual function?
At an early stage, the disease is often asymptomatic, does not affect the quality of vision, and can only be noticed if the child regularly undergoes routine ophthalmological examinations. During the examination, the doctor may detect specific changes in the fundus that indicate the onset of the development of Best's disease.
The first external symptom that may signal the development of childhood macular degeneration is a slight deterioration in visual acuity. During an examination at this stage, yellow dots can be seen in the center of the retina. The development of the disease leads to the growth of these points and the formation of cysts. If the patient complains of severe decrease and blurred vision, this may indicate that cysts have ruptured (a characteristic symptom of the third stage of the disease).
The most severe disturbances are characteristic of the fourth stage: vision is greatly reduced, scotomas appear in the visual field - areas of complete blindness.
Diagnosis of Best's disease
Diagnosis of childhood macular degeneration is based on the results of ophthalmoscopy, electroretinography and electrooculography readings. Fluorescein angiography is often used to confirm it. In complex situations, examination of the patient's family members may be necessary to assist in diagnosis.
In the case of a clearly defined yolk cyst, it is not difficult to make a diagnosis, but in case of unclear boundaries of the cyst and resorption of its contents, it is necessary to carry out a differential diagnosis. It is necessary to differentiate Best's disease from myopic maculitis, Stargardt's disease, serous macular edema, cystic degeneration of the macular zone, and choroiditis.
Best's disease - symptoms and treatment
To make a diagnosis of Best's disease, a number of examinations are necessary. First of all, it is necessary to register a specific ophthalmoscopic picture of the fundus, characteristic of each stage of the disease. Electrooculography (EOG) and electroretinography (ERG) should then be performed to assess the condition of the retina. In recent years, with the development of genetics, molecular genetic testing of the patient has become mandatory. At the same time, an ophthalmological and genetic examination of other family members is carried out.
Ophthalmoscopy can detect the first signs of Best's disease in the first and second decades of life. In the first stages, yellowish lesions appear in the macula, then vitteliiform cysts form, and when they rupture, the fundus of the eye resembles a “fried egg” picture. In the final stages, atrophic glial scars are formed in the macula, and in case of complications, a neovascular membrane and through macular holes are formed.
Electrooculography is a very important diagnostic method for Best's disease. With its help, it is possible to identify such a specific sign of the disease as a decrease in the Arden coefficient - the ratio of the biopotential of the eyes in the dark and in the light. This indicator will be reduced even at the zero stage of the disease with a normal ophthalmoscopic picture. In the case of adult vitelliform macular degeneration, electrooculography will not reveal changes.
Fluorescein angiography allows diagnosing Best's disease even at the preclinical stage. Changes in the retina depend on the stage of the disease. At the initial stage of the disease, small fenestrated defects and areas with local hyperfluorescence (glow) are visible. In the presence of a formed cyst, fluorescence is completely absent. At the third stage of the disease, hyperfluorescence is observed only in the upper part of the cyst, and is absent in its lower part [8].
With electroretinography (general and rhythmic), a decrease in the amplitude of “a” waves, an increase in the latent periods of “a” and “b” waves, as well as a suppression of the response from the central parts of the retina are observed [9].
Static computer perimetry reveals a decrease in the sensitivity of the macular region, and in the case of a ruptured vitelliform cyst, a central absolute scotoma (blind spot). At the same time, the boundaries of the visual field along the periphery remain normal.
Differential diagnosis
Best's disease must be distinguished from other diseases:
- Coats disease and other macular degenerations of the retinal pigment epithelium (X-shaped macular degeneration);
- acute chorioretinitis (primarily toxoplasmosis etiology);
- Stargardt's disease;
- vitelliform dystrophy of adults;
- retinal pigment epithelium detachment [11].
Coats disease is a congenital non-hereditary pathology in which abnormalities of the retinal vessels are observed. It can cause partial or complete blindness. In the first stages, Coats' disease, like Best's disease, occurs without symptoms and in most cases is diagnosed in children 2-8 years old during random preventive examinations carried out in kindergartens or schools. Unlike Best's disease, with Coats' disease, as a rule, only one eye is involved in the pathological process. Only 5-8% of patients have bilateral changes. Boys get it 3 times more often than girls [9].
In most patients with Coats' disease, the first ophthalmologic examination reveals a raised, round area of hard, yellowish exudate in the central retina, very similar to the vitelliform changes seen in Best's disease. These exudates in the central region of the retina are very often combined with hemorrhages behind the retina and the formation of new vessels, which is also characteristic of Best's disease.
Diagnosis of Coats disease is based on the results of examination of the fundus of the eye (ophthalmoscopy), as well as the central region and periphery of the fundus using either a head-mounted ophthalmoscope with 20-30 diopter lenses, or ophthalmobiomicroscopy with a three-mirror Goldmann lens. In most patients with Coats disease, during this examination, vascular anomalies are necessarily detected: micro- and macroaneurysms, telangiectasia (spider veins), arteriovenous shunts. Most often, these anomalies are located in the temporal half of the retina.
Changes in electrooculography in the initial and advanced stages of the disease, as in Best's disease, are not detected. But visual acuity in patients with Coats retinitis is low: in the presence of changes in the central region of the retina, it does not exceed 0.4, and in Best disease it remains normal for a long time [7].
Acute toxoplasmosis chorioretinitis is a parasitic eye disease, which is characterized by a mostly latent or chronic course. It usually affects only one eye, unlike Best's disease. With inadequate and untimely treatment, it can lead to a stable decrease in visual acuity.
Difficulties in diagnosis usually arise when examining patients with acquired toxoplasmosis and exudative-hemorrhagic changes in the central region of the retina, which are similar to vitelliform lesions with subretinal hemorrhages, as in Best's disease. Chorioretinal lesions in toxoplasmosis are combined with vitreous effusion of varying severity, and sometimes with changes in the anterior segment of the eye.
Patients, as a rule, complain of a sudden, sharp and significant decrease in central visual acuity, which in some cases changes to 0.01-0.2. With static perimetry, an increased threshold of brightness sensitivity, relative or absolute central scotoma is recorded. Electrooculography is usually unchanged.
To confirm and verify toxoplasmosis, it is necessary to perform immunological studies, determine antibodies to toxoplasma or isolate it using the PCR (polymerase chain reaction) method. In 95% of cases, toxoplasmosis chorioretinitis responds well to treatment, and visual acuity can be restored to its original values [12].
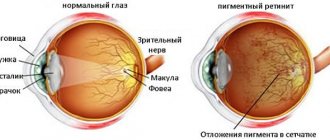
Stargardt disease is also called juvenile macular degeneration. This disease was first described by the German ophthalmologist K. Stargardt as a congenital lesion of the macula, which was inherited in one family.
As a rule, Stargardt's disease begins at a young (juvenile) age and is accompanied by damage to the central region of the retina, like Best's disease. It is characterized by rapid progression, even to the point of disability. Slow visual deterioration is extremely rare (with a dominant type of inheritance) [9].
This disease is always bilateral and symmetrical. Its characteristic signs are various processes: atrophy of the choroid (choroid of the eye), “bull’s eye”, a focus of dystrophy the color of “beaten (forged) bronze”, etc. With an advanced process, the foveal reflex (central fossa of the macula) is absent. In the macular region at the level of the retinal pigment epithelium, accumulations of brownish, dark pigment are observed, which is surrounded by areas of hyper- and depigmentation. These clusters are different from the vitelliform yellow lesions of Best's disease.
Vitelliform macular degeneration of adults , unlike Best's disease, develops in people 40-50 years old. It is characterized by bilateral symmetrical lesions of the macula with local changes. Foci of pathology, as a rule, have a round shape and a yellow tint. They are distinguished by the absence of progression and small size: the diameter of the lesions reaches 0.3-0.5 the size of the optic nerve head. At the same time, visual impairment is minimal.
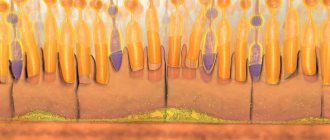
Substances like lipofuscin accumulate diffusely in various places: in the pigment epithelium, the inside of photoreceptors, Müller cells and even in the vitreous.
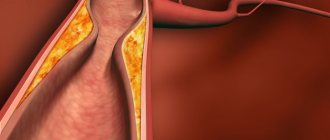
Retinal pigment epithelial detachment occurs when the normal connection of the retinal pigment epithelium to Bruch's membrane is disrupted. Causal factors include vascular, inflammatory and dystrophic processes.
The disease can exist for a long time without any dynamics, disappear spontaneously, and due to invasion of blood vessels from the choroid, transform into hemorrhagic detachment. Difficulties in diagnosis may arise with an atypical clinical picture of the disease and exudative changes in the central region of the retina.
Usually the disease affects only one eye. General electroretinography does not change, local electroretinography may be reduced. Electrooculography is usually normal. With fluorescein angiography, hyperfluorescence is recorded at the last stage of detachment.
Treatment of the disease
There is currently no effective and efficient treatment for Best's disease. Since the disease is usually asymptomatic and worries the patient, doctors, as a rule, do not take any special measures. In the case of the formation of a subretinal membrane, which can cause minor visual defects, laser coagulation of the retina is sometimes performed.
Compared with Best's disease, macular degeneration does not progress in adults and is associated with smaller lesions.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide treatment for identified pathologies. Experienced refractive surgeons, detailed diagnostics and examination, as well as the extensive professional experience of our specialists ensure a favorable outcome for the patient.
You can find out the cost of a particular procedure and make an appointment at the Moscow Eye Clinic by calling multi-line phone 8 (daily from 9:00 to 21:00, free for mobile phones and regions of the Russian Federation) or by filling out the online registration form.
Yakovleva Yulia Valerievna
Is vision loss inevitable in Best's disease?
Despite the fact that Best's disease is not curable today (there is only supportive therapy that slows down dystrophic and degenerative processes), ophthalmologists give a good prognosis for the preservation of visual function. The main condition is early diagnosis, which helps to start treatment on time, slow down the pathological process and preserve vision. This is why it is so important to visit an ophthalmologist at least once a year during childhood. If parents are aware of a family history, then visits to the doctor should be more frequent.
MagazinLinz.ru team
Diagnostics
A pulmonologist performs a physical examination, auscultation (listening) and percussion (tapping) of the respiratory system. The diagnosis of asbestosis is established on the basis of a carefully collected medical history, clarification of the circumstances and duration of exposure to asbestos, assessment of respiratory function (spirometry), and chest x-ray (or CT). These diagnostic data help the doctor evaluate lung function and the severity of the disease.
In some cases, additional research may be required to clarify the diagnosis:
- bronchoscopy - visualization of the mucous membranes of the trachea and bronchi (with a biopsy - for subsequent diagnostic examination of fluid or lung tissue);
- pleurocentesis - pleural puncture (to remove fluid between the lungs and the pleural cavity and examine the resulting material).
Examination for retinal dystrophy
For diagnosis it is necessary to conduct the following studies:
Visometry – visual acuity from normal (in the initial stage) to complete blindness. Cannot be corrected; - perimetry - narrowing of the field of view, from the appearance of scotomas to tubular vision; — Amsler’s test is the simplest subjective way to diagnose macular degeneration. The patient is asked to close one eye and look at a point in the center of the Amsler grid at arm's length, then slowly zoom in on the test without taking his eyes off the center. Normally, the lines are not distorted
Amsler test: 1. norm 2. Pathology
Refractometry – for diagnosing refractive errors (retinal degeneration is possible with high myopia); — biomicroscopy allows to identify concomitant pathologies; — ophthalmoscopy is performed after drug dilation of the pupil, preferably with a Goldmann lens for a more detailed examination of the retina, in particular the periphery. For different types of dystrophies, the doctor sees a different picture of the fundus; — determination of color vision – Rabkin’s tables, etc.; — electroretinography – indicators are reduced or not recorded in most hereditary dystrophies; - adaptometry - study of dark adaptation - reduction or absence of dark vision when cones are damaged; — fluorescein angiography to determine areas where laser coagulation of the retina is necessary; — optical coherence tomography of the retina
HRT (Heidelberg retinotomography); - Ultrasound of the eye; — general clinical tests; — consultation with a therapist, pediatrician, geneticist and other specialists according to indications.
Treatment of retinal dystrophy
Depending on the clinical picture and type of dystrophy, treatment is prescribed. Treatment is almost always symptomatic, since all degenerations, except secondary ones, are hereditary or predisposed.
The following treatment methods are used: conservative, laser, surgical (vitreoretinal surgery, scleroplasty for detachment, etc.)
Drug treatment:
Disaggregants (Ticlopidine, Clopidogrel, acetylsalicylic acid) - taken orally or parenterally; - vasodilators and angioprotectors (No-shpa, Papaverine, Complamin, Ascorutin); - anti-sclerotic drugs are prescribed mainly to elderly people - methionine, simvastatin, atorvastatin, clofibrate, etc.; — combined vitamin preparations (Okuwait-lutein, Blueberry-forte, etc.), as well as intramuscular B vitamins; - agents that improve microcirculation (pentoxifylline parabulbar or intravenously) - polypeptides from the retina of cattle (Retinalamin) parabulbar daily for 10 days. The sub-Tenon space is injected once every six months; - biogenic stimulants - aloe, FIBS, encad (used intramuscularly or subconjunctivally for the treatment of taperetinal dystrophy); — apply taufon drops, emoxipine drops topically, 1 drop 3 times a day, constantly or at the discretion of the doctor.
For the exudative form of age-related macular degeneration, dexamethasone 1 ml is administered parabulbarly, as well as furosemide intravenously. For hemorrhages, heparin, etamsylate, aminocaproic acid, and prourokinase are used. In case of severe edema, triamcinolone is injected into the sub-Tenon's space. Routes of administration, dosage and duration of treatment depend on each specific case.
Physiotherapy
also effective for retinal dystrophies: electrophoresis with heparin, no-spa, nicotinic acid, etc., magnetic therapy, and stimulation of the retina with low-energy laser radiation are used.
Laser coagulation of the retina is considered the most effective treatment method
, in which damaged areas are demarcated from healthy tissue, thereby stopping the development of the disease.
For the formation of vitreoretinal adhesions and neovascular membranes, vitrectomy
.
Hereditary retinal dystrophies have an unfavorable prognosis and almost always lead to blindness.
For age-related macular degeneration, inpatient treatment is indicated 2 times a year, and it is also recommended to wear sunglasses and quit smoking.
Ophthalmologist Letyuk T.Z.
Best's disease is a serious hereditary ophthalmic disease that occurs in 4 people out of 100 thousand. The main problem is that the disease is asymptomatic in the initial stages, and manifests itself when vision begins to rapidly decline.
Fortunately, Best's disease rarely leads to complete loss of visual function. The article will discuss the characteristics of the disease, what symptoms are characteristic of it, as well as the most effective methods of treatment.