What it is?
Angiopathy is a condition of retinal vessels in which capillary circulation changes due to disturbances in their nervous innervation. This occurs due to low blood filling of the vessels or their prolonged spasm.
Medicine does not distinguish angiopathy as an independent disease; modern scientific approaches classify it as one of the manifestations of the underlying disease.
Such a symptom complex can be a consequence of metabolic or hormonal disorders, injuries and intoxications, as well as the consequences of such bad habits as smoking or drug addiction. Most often, angiopathy is diagnosed in the adult population (over 30 years of age); a small percentage occurs in childhood and adolescent forms of the pathology.
This condition, if detected and treated in a timely manner, is reversible. Only in advanced cases does the disease lead to serious complications:
- development of dystrophy and atrophy of the retina and optic nerve;
- decreased acuity and narrowing of visual fields.
Stages of retinal angiopathy
Treatment of angiopathy is prescribed by an ophthalmologist after a thorough examination. The success of therapy directly depends on procedures aimed at getting rid of the underlying disease.
Diagnostics
With such problems, you can contact an angiosurgeon or endocrinologist. After examination and collection of complaints, the doctor prescribes laboratory, instrumental and hardware assessment of the following indicators:
- biochemical screening – glucose, creatinine, urea levels, blood clotting status;
- ECG, echo CG at rest and with exercise;
- X-ray examination;
- arteriography of the lower extremities - assessment of patency using a contrast agent;
- Dopplerography - ultrasound examination of the condition of blood vessels;
- in the presence of purulent discharge from an ulcer - bacteriological examination with an antibiogram;
- determination of transcutaneous tension - assessment of oxygen levels in the tissues of the extremities;
- computer capillaroscopy.
Diagnostic procedures are carried out not only to make a diagnosis, but also during treatment to assess the condition of the vessels over time.
ICD-10 code
According to the international typology of diseases, angiopathy does not have its own code, since it is not assigned the status of an independent disease. Therefore, coding is based on the pathology that caused vascular imbalance in the retinal tissue. These can be various diseases:
- traumatic injuries to the eyes, face, neck, head;
- high intracranial or blood pressure;
- osteochondrosis, cervical spondylosis ;
- diabetes;
- hypo- or avitaminosis;
- blood diseases;
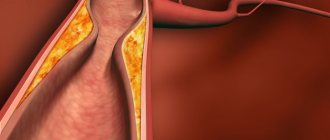
- atherosclerosis, vasculitis;
- intoxication with microbial toxins or poisoning with chemicals (radiation);
- strong physical and psycho-emotional stress, causing prolonged spasms of the capillaries;
- presbyopia or tissue degeneration in the eye apparatus.
Causes
Hypertensive retinal angiopathy occurs exclusively when there is a violation of blood pressure, and the causes of the disease can be very different: diabetes mellitus, high and low blood pressure, head injuries and their consequences.
Systematic vascular inflammation, spinal curvature and osteochondrosis disrupt the normal functioning of the circulatory system, also contributing to the occurrence of the disease.
It may also be useful for you to learn about how retinal hemorrhage occurs and what can be done about such a problem.
Elderly patients are mainly affected by angiopathy. In addition, the progression of this disease is facilitated by:
- congenital defects in the formation of retinal vessels;
- excessive alcohol consumption;
- intoxication of the body;
- nicotine addiction;
- excess body weight;
- work in hazardous production;
- unbalanced diet;
- existing chronic diseases (atherosclerosis, diabetes mellitus).
Kinds
Angiopathy has its own classification:
1. Juvenile (Eales disease), refers to rare pathologies with unknown etiology. The disease affects young people and manifests itself:
- inflammation of the capillaries and veins and proliferation of connective fibers in the retina;
- hemorrhages in the tissue of the eye;
The prognosis of the disease is serious, as it can provoke retinal detachment and partial or complete loss of vision, as well as the development of cataracts or glaucoma.
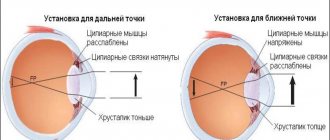
2. Retinal angiopathy of the hypertensive type is caused by high blood pressure in patients; because of this, the vessels of the eyes are often in a narrowed state, which prevents normal blood supply to the retina, and often occurs with pronounced changes in the fundus.
3. Traumatic angiopathy develops with injuries to the head, neck or chest. Here, mechanical compression of veins and capillaries or increased intracranial pressure is possible. The pathology causes temporary or long-term loss of visual acuity, damage to the nerve plexuses innervating the eyes, and degenerative changes in the cells of the retina and vitreous body.
4. The hypotonic type of the disease is characterized by overflow of blood vessels and their pathological expansion, therefore there is a risk of increased thrombus formation and hemorrhages in the eye tissue.
5. Diabetic angiopathy is a consequence of the progression of this disease. Improper cellular metabolism causes changes in the structure of blood vessels (thinning or obesity), so normal blood circulation through them is disrupted.
6. The age-related form of the disease occurs due to the aging of the body, worn-out vessels can no longer cope with the loads, their tone decreases, and degenerative changes appear.
There are cases when angiopathy occurs of a mixed type, i.e. their development causes a whole “bouquet” of internal diseases, for example, diabetes mellitus coupled with atherosclerosis or arterial hypertension occurring against the background of obesity. In such cases, the course of the pathology worsens and requires more intensive drug therapy.
Treatment
Along with the general principles of treatment of retinopathy, therapy includes the correction of metabolic disorders, optimization of control over glycemic levels, blood pressure, and lipid metabolism. Therefore, at this stage, the main therapy is prescribed by an endocrinologist-diabetologist and a cardiologist. The level of glycemia and glucosuria is carefully monitored, and adequate insulin therapy for diabetes mellitus is selected; Angioprotectors, antihypertensive drugs, antiplatelet agents, etc. are prescribed. Intravitreal steroid injections are performed to treat macular edema. Patients with progressive diabetic retinopathy are advised to undergo laser coagulation of the retina. Laser photocoagulation makes it possible to suppress the process of neovascularization, achieve obliteration of vessels with increased fragility and permeability, and prevent the risk of retinal detachment. There are several main techniques used in retinal laser surgery for diabetic retinopathy. Barrier laser coagulation of the retina involves the application of paramacular coagulates in a “lattice” pattern, in several rows, and is indicated for non-proliferative retinopathy with macular edema. Focal laser coagulation is used to cauterize microaneurysms, exudates, and small hemorrhages identified during angiography. In the process of panretinal laser coagulation, coagulates are applied over the entire retinal area, with the exception of the macular area; this method is mainly used at the preproliferative stage to prevent its further progression. When the optical media of the eye are clouded, an alternative to laser coagulation is transscleral cryoretinopexy, based on cold destruction of pathological areas of the retina. In the case of severe proliferative diabetic retinopathy, complicated by hemophthalmos, traction of the macula or retinal detachment, vitrectomy is performed, during which blood and the vitreous itself are removed, connective tissue cords are dissected, and bleeding vessels are cauterized.
Retinal angiopathy in a child
Changes in the tone of blood vessels in the eyes in children in infancy can be observed with a change in body position or hysterical crying. This occurs due to the immaturity of the circulatory and nervous system of babies and is not a pathology. The painful condition of the blood vessels in the eyes in children is indicated by a prolonged spasm of the veins and capillaries, diagnosed during examination in a hospital (maternity hospital, children's hospital) or in an outpatient setting.
The most common cause of retinal angiopathy in both eyes in newborns is increased intracranial pressure. In older children, these are injuries, metabolic disorders, systemic autoimmune diseases and hereditary pathologies.
Can cause vasospasm of the eyes in children:
- severe viral diseases and bacterial infections (tuberculosis, meningitis, brucellosis, complicated influenza, etc.);
- parasitic diseases (toxoplasmosis and advanced helminthic infestations);
- poisoning by mercury vapor, chlorine and other chemicals;
- inflammatory eye diseases and excessive visual stress at school or at home (passion for computer games, watching television);
- renal pathologies;
- rheumatism;
- lack of protein foods, vitamins or minerals;
- severe physical fatigue, over-acclimatization, prolonged nervous excitement.
Video:
Prevention
The main preventive measure of GAS is blood pressure control. This is especially important for people who have a hereditary tendency to hypertension.
Preventative measures will help prevent the disease:
- do exercises every day; ride a bike, walk, run at an easy pace.
- eat right;
- do not drink alcohol;
- maintain normal weight;
- take vitamins;
- control your psycho-emotional state, avoid stress;
- get plenty of rest and sleep.
There is no need to take any special measures to prevent GAS - the above recommendations should be followed by any person who cares about their health.
Symptoms
Clinical signs of the disease appear:
- in decreased visual acuity;
- in the appearance of flickering, white or dark spots before the eyes, “fiery flashes, lightning, flashes”;
- increased eye fatigue when reading, watching TV or working on a PC;
- in the formation of a network of capillaries on the mucous membrane of the eyes, in redness of the conjunctiva, in the detection of pinpoint hemorrhages;
- in reducing the fields of lateral vision;
- a feeling of pulsation inside the eyes;
- in pathological changes in the fundus (during an objective examination by a doctor).
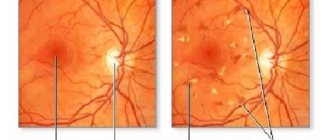
Degrees of the disease
In modern ophthalmology, it is customary to classify this disease depending on the degree of vascular damage. The determination is made by a specialist based on comprehensive diagnostic measures.
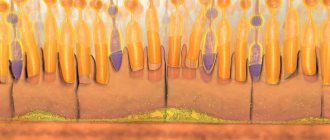
Angiopathy of the first degree is caused by physiological changes in the organs of vision. In this case, the veins dilate, the volume of the retinal arteries decreases, the structure of the vessels is disrupted, and their tortuosity increases. But what eye drops to improve vision should be used first and what they are called is indicated here.
The second degree is marked by organic modifications in the structure of the eyes. The strong growth in the caliber of the vessels and their branching makes them look like copper and then silver wire, due to the narrowing of the central light strip of the vessel. Further, the damage to the vessels grows, they take the form of a thin, colorless line, and subsequently the vessels become clogged with blood clots. But what to do when blood vessels in the eyes often burst and what remedies can help with such a problem.
On the surface of the optic nerve head, capillaries dilate and new growths form; the fundus of the eye becomes yellow-waxy.
It is also worth paying attention to what a macular hole in the retina looks like.
In the third degree, which is called angioretinopathy, as a result of the ingress of blood particles, the retina swells and white lesions appear. The final stage of the third degree is caused by complete or partial swelling of the surface of the optic nerve. But how inflammation of the optic nerve occurs and how it is treated can be seen here.