Causes of aphakia
The absence of a lens in the eye can be congenital or acquired; the latter type is more common. The congenital form is divided into 2 categories: primary and secondary. In the first variant, the lens did not develop due to genetic disorders, in the other, its rapid destruction occurred after initiation. If the lens is lost in one eye, aphakia is called monocular; if both organs are affected, it is called binocular.
The causes of the congenital form are determined by two factors:
- failures at the genetic level in the process of separation of the lens vesicle from the outer ectoderm at the stage of embryogenesis;
- idiobatic absorption of the lens due to random mutation.
The risk of getting the disease increases with age; one of the reasons for the acquired form is surgical removal of cataracts. It can also occur due to spontaneous dislocation of the lens, deep injuries to the eye.
Forms and stages of disease development
The lens may be missing in one or both eyes. Based on this feature, the following forms of the disease are distinguished:
- Monocular (one-sided) – a healthy lens is present only in 1 eye. This form is often accompanied by aniseikonia - a violation of vision of the true size of objects.
- Binocular (bilateral) is a common consequence of severe cataracts, due to which the lens is deformed in both eyes.
This disease significantly worsens the quality of life and can lead to disability.
Depending on the severity of the disease, the following stages are distinguished:
- Unilateral aphakia, vision drops to 0.4-1 diopter. There is a possibility of correction in the eye that sees better.
- Unilateral or bilateral with a significant decrease in acuity and narrowing of the visual field.
- Monocular, accompanied by other ailments affecting the healthy eye.
- The absence of a lens in one or both eyes results in serious ophthalmological pathologies, and vision deteriorates significantly.
According to the stages of the disease, patients are assigned a disability group: from limited VKK to group 1.
Important! At the first signs of pathology, you should immediately consult an ophthalmologist. Due to the disease, there is a possibility of becoming completely blind.
Symptoms of aphakia
A distinctive sign of the pathology is trembling of the iris, called iridodonesis. The iris is held in its normal position by the lens; without it, it becomes mobile and goes deeper. It is especially noticeable when the eyes move in different directions. Visual acuity decreases, accommodation worsens.
Other possible symptoms include:
- “fog” before the eyes;
- dual image;
- headache;
- noise in ears;
- inability to focus.
From a prognosis point of view, unilateral aphakia is considered unfavorable. Due to the formation of images on the retina of different sizes, a sharp deterioration in binocular vision occurs.
The congenital form of the disease is characterized by a progressive decline in vision; other clinical indicators do not indicate problems. Acquired symptoms depend on the underlying disease or injury that led to surgery.
The development of pathology in childhood is complicated by microphthalmia - a decrease in the size of the eyeball. This occurs due to the absence of a lens capsule - the vitreous body is limited only by the limiting membrane. The result is a hernia of the vitreous, which can lead to a dangerous rupture of the membrane. Surgical elimination of the problem can be complicated by keratitis and scars on the cornea.
Signs of aphakia
The presence of a pathological process in the visual apparatus may be indicated by the following complaints from patients:
- deterioration of vision, decrease in its acuity;
- the appearance of blurred vision before the eyes, veils, sensation of a foreign body;
- lack of accommodation, that is, a person does not see objects. The near and far points merge into one. This is the main sign of pathology;
- the right and left eyes do not receive a uniform image;
- Iridodonesis is a trembling of the iris that occurs when the eyeball moves. If previously the lens was a dense support, now the eye is deprived of such protection;
- impairment of binocular vision.
There is a significant deepening of the anterior chamber of the affected eye. Small remains or membrane of the lens are also found. If aphakia was preceded by surgery, the doctor may pay attention to the presence of a scar.
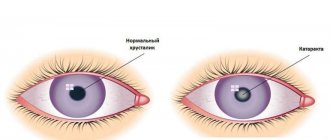
The photo on the right side clearly shows the main sign of aphakia, in which there is no clarity of objects, everything is blurry
Diagnosis of aphakia
If signs of aphakia are detected, you should immediately consult a doctor (delaying a visit is dangerous!). To diagnose aphakia, a comprehensive examination is used, the completeness of which depends on the cause of the disease. To detect the absence of a lens, the following examinations are carried out:
- refractometry;
- Ultrasound of the eye;
- biomicroscopy (using a slit lamp);
- examination of the eye chambers.
Additional tests may be ordered, depending on the specific case. This allows the ophthalmologist to determine the presence of a lens and, in its absence, the shape and degree of aphakia. If aphakia is caused by trauma, hematoma or scarring (an old wound) will be visible. If the ophthalmologist is not sure of the diagnosis, he may prescribe additional consultations with specialists in other fields.
Diagnostic measures
Diagnosis of the pathological condition is not difficult. An ophthalmologist conducts the following examinations:
- assessment of visual acuity;
- examination of eye chambers;
- biomicroscopy using a slit lamp;
- refractometry;
- ultrasound examination of the eyes.
All these methods make it possible to detect the absence of a lens, as well as to determine changes that develop in the eyes due to aphakia. The doctor also evaluates the person’s general condition, identifying signs of a disease that could cause aphakia.
So, in case of injury, hematomas and bleeding in the orbital area, the presence of a foreign object in the eye will be visible. If the injury occurred a long time ago, the doctor will see scars on the conjunctiva and cornea. If necessary, consultations with narrow specialists are prescribed.
The monocular form is considered the most unfavorable, since in this case a person perceives the world around him differently. This causes severe vision impairment, constant headaches and dizziness.
Additionally, see what aphakia looks like in humans:
Treatment of aphakia
One of the methods of vision correction in the absence of a lens is the purchase of glasses or contact lenses. The last option is more practical; it is suitable for any form of the disease, and also does not affect appearance. Suitable materials are selected for each age: for small children - soft silicone, for older children - soft breathable ones, even hard lenses are suitable for adults. The disadvantage of using corrective lenses is the need for frequent replacement, which means the cost of treatment.
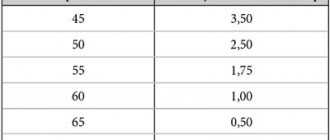
Glasses are prescribed only for bilateral aphakia; you need to purchase two pairs at once for near and distance, with the exception of myopia to the point of loss of the lens (needed only for near). Glasses for the correction of this disease have a highly convex shape, because the number of diopters ranges from +7 to +18.
Aphakic patients often suffer from astigmatism, which requires lenses with a cylindrical component. This makes making lenses a labor-intensive process and also detracts from their appearance. This correction is not suitable for children due to the heavy design of the glasses - it simply will not stay on the nose.
But appearance is not the only disadvantage of wearing glasses for aphakia. Due to the large plus, glasses can cause a ring scotoma - an entire area falls into the “blind spot”. This complicates everyday life and even makes it dangerous - when crossing the road, for example.
Surgical treatment begins with the removal of the natural lens. Then a plastic lens is installed in the patient’s eyeball, the parameters and size of which are calculated using special tables. Individual indicators are taken into account:
- refractive power of the cornea;
- eyeball length;
- anterior chamber depth;
- thickness of the lens.
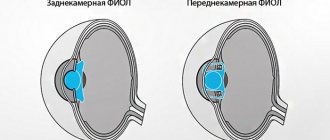
The patient’s activity and his wishes are also taken into account - for example, work related to a computer or driving. An intraocular lens (IOL) can be selected so that a person does not wear glasses during basic activities. Of the several types of IOLs, the best is considered to be the posterior chamber type, which occupies the most natural position in the eyeball. It does not interfere with the dilation of the pupil, and therefore does not impair the quality of vision.
Surgical treatment is carried out only after the final formation of the eye structure.
Treatment
Therapeutic measures for aphakia can be radical and non-radical. The latter includes vision correction using various types of lenses:
- contact correction with lenses directly adjacent to the cornea;
- glasses with diopters corresponding to the degree of vision loss.
Glasses are used for bilateral aphakia. If there is no lens in only one eyeball, spectacle correction can be used only if the patient has intolerance to contact lenses.
The selection of glasses is carried out individually, taking into account the degree of vision loss. Even a large number of diopters is not capable of fully correcting vision, since the refractive power of the lens is much greater.
The operation will help with the monocular form of aphakia. Surgical intervention consists of placing an intraocular lens - an artificial lens. The refractive power of such a lens is also selected individually, taking into account the degree of refraction of the remaining transparent media of the eye. There are several types of IOLs (intraocular lenses):
- fixed in the corner of the anterior chamber of the eye;
- pupillary clip lens – attached to the edges of the pupil;
- extracapillary;
- posterior chamber.
Surgical treatment of children with congenital aphakia of the eye is possible only from the age of two, when the formation of the structures of the eyeball is finally completed. Until this age, correction is carried out with glasses or contact lenses.
As the child grows, it is necessary to adjust the diopters in glasses or lenses. For newborn children, special silicone soft lenses are used, for older children - hard ones.
Drug treatment is ineffective and can only be prescribed to eliminate associated symptoms. Drops with vitamins, vasoconstrictors and moisturizers are prescribed.
Prevention
In ophthalmological practice there are no special preventive measures regarding the congenital form of the pathology. If you have chosen the right methods for correcting aphakia, then you will have a favorable prognosis.
Regarding acquired forms of pathology, experts recommend an annual examination by an ophthalmologist. This allows for timely diagnosis of diseases that provoke surgical removal of the lens. If your profession involves hazardous situations, use a mask or safety glasses. Since this disease is considered quite rare, the treatment of aphakia should be carried out exclusively by specialists.
Aphakia in children
Congenital uncomplicated aphakia is a very rare defect. However, congenital cataracts, which can lead to the development of this pathology, occur more often: in approximately one case per two thousand newborns.
Newborns must be examined by an ophthalmologist
Aphakia is a condition that parents can notice in their children themselves.
If you have any suspicions, be sure to contact a pediatric ophthalmologist immediately. There are several methods for correcting childhood aphakia, each of which is used at a certain age:
- For infants under 2 years of age, special soft contact lenses are used. Other means of correction are usually not used in such young children; this is due to the very active growth of the organ of vision during this period.
- Glasses are used from the age of two, when the child already begins to understand their purpose and the possibility of injury through glasses is reduced.
- Epikeratoplasty - also used from 2-3 years.
- Intraocular lenses are not used for younger children, as there is a risk of various complications with such an operation. This method is popular for correcting aphakia in children over 2 years of age.
When using glasses and contact lenses in children, constant supervision by a specialist is necessary, since the refraction of a growing eye is constantly changing, which means they will have to be changed regularly.
Diagnostics
The problem can be identified during the first visit to the ophthalmologist, but the diagnostic process must take an integrated approach, including a number of laboratory and instrumental examinations.
The first stage of diagnosis is aimed at the clinician performing the following manipulations:
- studying information regarding the course of pregnancy;
- familiarization with the patient's medical history;
- collection and analysis of life history;
- assessment of visual acuity of both eyes;
- examination of the visual organs using specially designed ophthalmic devices;
- a detailed survey of the patient regarding the first time of appearance and intensity of symptoms.
Then laboratory tests are carried out, including:
- general clinical blood and urine tests;
- blood biochemistry;
- blood sugar test.
The final step of diagnosis is instrumental examinations:
- visometry and perimetry;
- tonometry and biomicroscopy;
- ophthalmoscopy and refractometry;
- gonioscopy and ultrasonography of the eye.
Gonioscopy