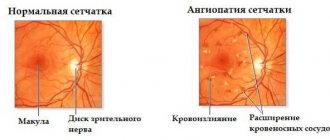
Macular degeneration (macular degeneration, age-related macular degeneration, AMD, CCRD) is the collective name for a group of retinal pathologies that can have different etiologies. But regardless of the cause, all these pathologies have a similar damaging effect on the area of the retina called the macula (macula), and therefore on central vision, since it is the area of the macula of the retina that provides the greatest visual acuity.
How does the macula work and what is it responsible for?
As you know, the retina is the inner layer of the eye, consisting of several layers of light-sensitive cells (photoreceptors). Receptors in the retina (cones and rods) perceive and transmit information in the form of light impulses to the overlying parts of the brain, where it is deciphered and converted into visual images. The entire chain of reactions described underlies the functioning of the vision system.
The macula (macula) is a small area of the retina located opposite the pupil and has an oval shape. This area of the retina got its name due to the accumulation of cells here containing yellow pigments (lutein and xanthine). The macula is responsible for the formation of the so-called central vision, that is, the central portion of the visible image. The cells of the macula are responsible for the eye's ability to see the smallest details of an image, its shape and color. We use central vision when we write, read, draw, or do work that requires concentration on small objects (threading a needle, stringing beads). It is central vision that helps recognize faces.
What not to do with macular degeneration
If a diagnosis of macular degeneration has been made, then it is strictly forbidden to let the disease take its course or self-medicate. It is necessary to carry out the treatment prescribed by the doctor and follow all recommendations. For age-related macular degeneration, the following is prohibited:
- eat high-fat foods;
- stay at the computer or TV for a long time;
- use optical correction tools;
- do thermal procedures;
- smoke and drink alcohol;
- drink plenty of fluids;
- exercise intensively.
If you have AMD, it is recommended to avoid eating salt and not going out in the sun without sunglasses.
Why does AMD occur?
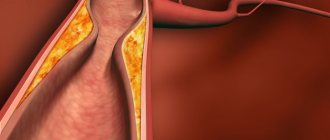
With macular degeneration, the photoreceptors of the macula are affected, resulting in impaired central vision. Macular degeneration can occur due to a large number of reasons, one of the main ones being dystrophic changes in the vessels of the retina. Disruption of normal oxygen transport through altered vessels causes oxygen starvation of retinal cells.
The risk of AMD increases with age: studies show that the highest incidence of macular degeneration is observed in the age group over 60 years. In addition to age, risk factors include excess weight and smoking, gender (women get sick more often than men), as well as detection of AMD in close relatives. The results of numerous scientific studies allow us to say with confidence that macular degeneration is a genetically inherited disease.
What it is?
Macular degeneration is an ophthalmological disease in which tissue damage to the retina occurs in its central part, which is commonly called the macula or yellow retina. In normal condition, the macula provides good color perception and high visual acuity. But with age, degenerative processes begin to occur in the structure of the eyeball, as a result of which central vision is impaired. Most often, this form of dystrophy occurs in older people, which is why it is also called age-related macular degeneration (AMD).
"Dry" form of macular degeneration
Currently, two forms of macular degeneration are distinguished: “dry” (non-exudative) and “wet” (exudative, neovascular). The first type of disease is detected in 9 out of 10 cases of AMD diagnosis. Approximately 10–20% of patients with nonexudative macular degeneration subsequently develop a “wet” form of AMD.
The development of the “dry” form of AMD is caused by atrophy of the tissues of the central parts of the retina due to age-related changes or, as a consequence, the deposition of yellowish pigment accumulations (drusen) here. Identification of drusen is one of the early pathognomonic symptoms of dry macular degeneration. The disease can develop in only one eye, or both eyes can gradually become involved in the pathological process.
Cost of treatment
The price of laser coagulation of the retina for the wet form of the disease is 11,000 rubles.
The cost of one intravitreal injection in our clinic is 19,000 rubles.
The cost of treating the dry form of macular degeneration depends on the individually selected drug therapy plan (inclusion of parabulbar or other injections, etc.).
If you have questions, you can ask our specialists using the feedback form on the website or by phone in Moscow 8 (800) 777-38 81 and (daily from 9:00 to 21:00).
Yakovleva Yulia Valerievna
Stages and symptoms of “dry” macular degeneration
The non-exudative form of macular degeneration occurs in three stages. Regardless of the stage of the disease, a patient with AMD does not experience any pain.
At the initial (early) stage, upon examination, the doctor identifies several small drusen in the fundus. There are no complaints or symptoms indicating changes in vision.
If, during an examination of the fundus, a large number of drusen or atrophy of the retinal pigment epithelium is detected, this indicates the transition of the disease to an intermediate stage. The patient may complain of a blurry spot appearing in the center of the visual field, as well as worsening vision at dusk or in poor lighting conditions.
The late stage of “dry” macular degeneration is characterized by the destruction of photoreceptors in the macular region of the retina, which is accompanied by symptoms of central vision impairment: the appearance of a blurred spot in the center of the visual field, which becomes darker and increases in size over time. It becomes difficult for the patient to read and write, and he has difficulty distinguishing the faces of others, even at close range.
Classification
There are two forms of AMD:
- Dry form - characterized by changes in the retinal pigment epithelium (formation and subsequent accumulation between the basement membrane of the RPE and the inner layer of Bruch's membrane, extracellular deposits of various sizes of eosinophilic material (yellow pigment) - the so-called drusen, which leads to disruption of retinal nutrition (Fig. below ).
- Wet form - characterized by the growth of newly formed blood vessels through Bruch's membrane into the space between the retina and the pigment epithelium. Neovascularization is accompanied by retinal edema, serous detachment of the neuro/retinal pigment epithelium, and hemorrhages (Figure below).
Druze
Diagnosis of non-exudative form of AMD
Examination of patients with suspected macular degeneration begins with determining visual acuity and examining the retina in conditions of a wide pupil (mydriasis). If drusen or other symptoms characteristic of macular degeneration are detected, additional examination methods are used: Amsler test, determination of visual fields, OCT, etc.
Without timely and complete treatment, progressive age-related macular degeneration leads to irreversible changes in the retina, manifested in the form of decreased visual acuity or blindness. To prevent vision deterioration, at the slightest suspicion of retinal damage, you should consult a doctor.
Symptoms
Macular degeneration of the retina varies according to the stages and forms of the disease. Let's look at the general symptoms:
- distortion of vision;
- hallucinations in the form of distorted straight lines;
- difficulty reading books;
- poor visibility in the dark;
- spots, dots before the eyes.
The listed symptoms appear in one or two eyes. In the second case, the person gradually gets used to the new state, and therefore triggers the disease.
How does a person with macular degeneration of the retina see:
You can watch the following video for more information about the symptoms of this disease:
Treatment of the “dry” form of macular degeneration
At the early stage of the disease, no specific treatment is usually used. Supplementation with antioxidants, including vitamins A, E and C, lutein and zeaxanthin, and zinc, has been found to prevent the progression of retinal symptoms in patients with non-exudative AMD. At the same time, taking vitamins and antioxidants does not have a preventive effect in patients at risk. For them, lifestyle changes will be more effective:
- to give up smoking;
- weight loss;
- protecting eyes from the harmful effects of direct sunlight;
- a diet that includes regular consumption of green leafy vegetables and fish;
- taking vitamin complexes containing folic acid (2.5 mg/day), vitamins B6 (50 mg/day) and B12 (1 mg/day).
The use of physiotherapeutic methods, including at home, has a good effect. Vacuum massage courses (AMBO-01 device) are recommended for patients undergoing drug treatment. Its use enhances the effect of medications and improves blood supply to the eyeball.
Of the surgical methods for CCRD, the most effective today is revascularization of the posterior pole of the eye. Activation of blood supply and metabolic processes can be performed using the patient’s own tissues or using an allograft. The operation not only stops the process of retinal degeneration, but also improves visual functions.
Ophthalmologists at our medical center specialize in the diagnosis and treatment of retinal diseases. Our specialists guarantee accurate diagnosis using modern equipment and use the most effective methods for treating eye diseases.
Causes
The etiology of the disease is not reliably known, but there is a close relationship between AMD and the influence of a number of factors:
- Age (after 55 years).
- Genetic predisposition (unfavorable family history).
- Cardiovascular diseases ( atherosclerosis , hypertension , hypotension ).
- Smoking.
- Increased body weight ( obesity ).
- Exposure to sunlight.
- An unbalanced diet deficient in omega-3 fatty acids, vitamins and minerals.
What is the essence of pathology
The name of the disease comes from the site involved in ischemia. The macula is an area of the retina characterized by light sensitivity and located in the central zone. It helps a person not only clearly see objects located in front of the eyes, but also distinguish colors or shades.
Macular degeneration should be understood as a whole group of pathological changes leading to deterioration of central vision. They arise due to damage to the retina of the eye. Macular sclerosis and degenerative processes represent its degeneration. In most cases, a person does not lose vision, but its quality deteriorates significantly, which interferes with reading, writing and other activities.
Anatomy of the eye.
The disease code according to ICD-10 is H35/3 (degeneration of the macula and posterior pole).
How is macular degeneration diagnosed?
To diagnose macular degeneration of the retina, your doctor will examine your eyes using a microscope. While the doctor performs the examination, a very bright light called a slit lamp will be shined into the eye. Different types of macular degeneration cause different microscopic changes in the eye, which your doctor will look for when examining your eye.
Dry macular degeneration
When the following signs are found during examination, it indicates that a person is developing dry macular degeneration:
- hyper- or hypopigmentation of the retina (areas of the retina are noticeably darker or lighter than others);
- patchy discoloration of the macula;
- large fat deposits around the macula;
- soft fatty deposits;
- destruction of the retinal pigment epithelium (the membrane that separates the retina from the choroid and supplies it with nutrients).
Wet macular degeneration
When the following signs are found during examination, it indicates that a person is developing wet macular degeneration:
- subretinal fluid (fluid accumulation around the retina);
- subretinal hemorrhages (bleeding around the retina);
- retinal scarring.
Diabetic retinopathy
When the following signs are found during examination, it indicates that a person is developing diabetic retinopathy:
- microaneurysms (stretching of microscopic blood vessels);
- hemorrhages;
- hard exudates (small yellow deposits that form from blood vessels leaking into the retina);
- changes in veins;
- formation of new veins;
- thickening of the retina.
Other eye examinations
If the examination reveals macular degeneration of the retina, other examinations may be performed:
- Fluorescein angiography: X-ray of the eye, performed after a fluorescent dye is injected into the blood vessels. This test can be used if wet macular degeneration is suspected. This allows the doctor to assess the extent, size and location of neovascularization (abnormal growth of blood vessels) and the extent to which blood is leaking from the blood vessels. Testing may also be performed to rule out nonmacular degenerative causes of visual impairment;
- Optical coherence tomography: a technique that uses a laser to create an image of the eye or other organs. It is used to assess the extent of retinal thickening and fluid accumulation in the retinal tissue.
- Indocyanine green angiography: A procedure similar to fluorescence angiography but using a different type of dye, can also be used to help the doctor assess the extent of abnormal blood vessel growth. This examination is usually not necessary as fluorescein angiography will provide this information.
Prevention
- What products do doctors recommend for age-related macular degeneration? — It has been proven that people who consume large quantities of vegetables and fruits and berries are less susceptible to the disease (blueberries are the most beneficial). Greens, carrots, spinach, cabbage, tomatoes, apples - they should always be present in the daily diet. Fat intake should be optimized. Eat fish and seafood at least twice a week.
- See an ophthalmologist regularly. After 60 years of age, it is recommended to visit a doctor at least once a year.
- Maintain visual hygiene: you cannot read, write, or do other things in rooms with insufficient lighting;
- Avoid eye strain;
- Protect your eyes during hazardous work (for example, welding) from ultraviolet rays. Sunglasses must have a high degree of protection.
- Take vitamins and minerals.
- Do not smoke or stay in smoky areas.
When a person is helpless, his quality of life decreases. To be active and independent, you need to take care of your health, especially your eyes. An active lifestyle, feasible physical exercise, and giving up bad habits will help delay vision loss for many years.
Video:
Related articles:
- Nystagmus of the eyeball: what is it and how is it treated?
- Farsightedness. How to restore vision?
- Cataract: causes, symptoms, treatment and prevention
- Allergies in the eyes: drops, medications for treatment, relieving redness and swelling
Intraocular injections
Source: glazalazer.ru This is the most common method of treating wet macular degeneration.
There are several drugs for intraocular administration, the most common of which is Lucentis. It relieves swelling from the retina and prevents the growth of abnormal blood vessels. It really does prevent it. However, few doctors convey to their patients the information of the International Congress of Ophthalmologists, which, based on the results of clinical observations, adopted the following procedure for working with the drug: if three consecutive injections of Lucentis do not have an effect, the drug is discontinued.
The fourth and any subsequent injections of Lucentis, even in patients with a positive reaction to the drug, are considered ineffective.
Regenerative therapy
The greatest effect in the treatment of macular degeneration of the retina is shown by the method of regenerative therapy. Clinics in Israel, Germany and Vietnam are conducting their research in the field of tissue technologies; doctors in Kyiv and Minsk are following a similar path, but have not yet proposed an effective technique.
Despite all the effectiveness of the method, you will not hear stories from our patients “how I cured macular degeneration” or “how I got rid of macular degeneration.” It is necessary to clearly understand that macular degeneration is a serious, steadily progressing disease.
No one knows the reasons for its occurrence and cannot influence them. Therefore, no one knows how to cure macular degeneration of the retina forever.
For this reason, in order to maintain the achieved result, the procedure must be repeated regularly - approximately once a year. Violation of the treatment regimen leads to a natural decrease in vision.