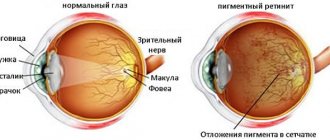
Retinal dystrophy is a dangerous condition in which gradual, often asymptomatic, destruction of the retina occurs, causing a noticeable deterioration in visual functions. One of the types of dystrophy is PVHRD - peripheral vitreochorioretinal dystrophy of the retina. This degenerative process is often a consequence of impaired blood supply to the fundus and can be eliminated either conservatively or surgically.
Causes
PVKhRD - what is it? This is dystrophy of the peripheral retina, which is common and can occur at any age. The exact mechanism of development of the pathology is unknown. The following factors can provoke the appearance of peripheral vitreochorioretinal dystrophy:
- high blood pressure;
- genetic predisposition;
- myopia;
- hypermetropia;
- diabetes;
- vascular atherosclerosis;
- inflammatory processes;
- damage to the organs of vision;
- infectious diseases;
- intoxication of the body.
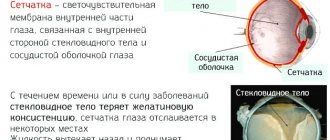
Under the influence of a number of factors, the blood supply to the visual apparatus is disrupted, material metabolism is disrupted, as a result of which the walls of the retina become thinner and the vitreous body is damaged. Such degenerative changes lead to visual impairment, and in the presence of provoking factors such as physical or emotional stress, excessive visual stress or exposure to vibration, rupture or detachment of the retina may occur.
Causes
In most cases, peripheral chorioretinal dystrophy is a hereditary disease. A high risk of development is provoked by the presence of myopia. Rarely, the pathology may occur as a consequence of farsightedness. Such disorders may be systemic or related to ocular pathologies. Main reasons for development:
- genetic predisposition, presence of PVCD in parents;
- myopia;
- inflammatory processes;
- injuries;
- complications after operations;
- diabetes;
- intoxication of the body;
- viral diseases;
- disorders of the cardiovascular system;
- prolonged exposure to the sun without the necessary protection;
- vitamin deficiency.
Young people often face such a lesion due to severe myopia.
Symptoms
A peculiarity of the occurrence of peripheral vitreochorioretinal dystrophy of the retina is its asymptomatic course, which complicates the timely diagnosis of the problem. The first signs of PVCRD are often observed already in the presence of retinal tears. Dystrophic changes in the periphery of the eye can be suspected by the following symptoms:
- flashing “flies” before the eyes;
- bright flashes of light;
- blurred vision;
- color vision impairment;
- decreased visibility in the dark;
- narrowing of the field of view.
Central vision is not impaired in PVCRD, only a gradual deterioration in peripheral visual functions is observed. If treatment is not started promptly for a retinal rupture and the degenerative process continues to progress, then bleeding into the vitreous or retinal detachment is possible, which ultimately leads to loss of vision.
Some types of peripheral retinal dystrophy
It is very important to correctly determine the type of peripheral retinal dystrophy, since the choice of treatment method and prognosis depend on this. Let's look at some of the most important types of this disease.
Lattice dystrophy
It is considered one of the most dangerous and unfavorable types of illness. More than half of the cases end in retinal detachment and have a poor prognosis. A genetic predisposition to this pathology is assumed; it is more common in men; as a rule, it is detected in two eyes at once. When examining the fundus, it appears as a series of narrow white stripes that form something similar to a lattice.
"Snail Trail"
Also refers to unfavorable forms with a high risk of complications. Multiple inclusions in the form of streaks with thinning and perforated defects are found on the retina. Such zones can merge and form ribbon-like zones, which resemble a snail's mark. As a result of this shape, large, rounded retinal tears can develop.
Frost-like dystrophy
It is hereditary in nature, usually bilateral and symmetrical. When examining the fundus, large white or yellowish inclusions in the form of snow flakes or frost attract attention. The disease progresses slowly and does not lead to complications as often as the previous two forms.
Cobblestone degeneration
It is also called the “bear trail”. Elderly people with high myopia are at risk. Upon examination, the ophthalmologist sees individual white lesions, around which small pigment inclusions are identified. The pathology is characterized by slow progression and a favorable prognosis.
Ophthalmoscopic picture in some forms of peripheral retinal degeneration
Microcystic dystrophy (hand-shaped)
When examining the fundus, a large number of small cystic formations are revealed on its periphery, which can merge and form larger cysts. With trigger factors (falls, injuries), cysts can rupture with the formation of retinal tears. The disease progresses slowly and has a favorable prognosis.
Retinoschisis
Most often this is a hereditary pathology (malformation of the retinal membrane). It is characterized by retinal separation, which develops due to the formation of fluid-filled cysts. The disease can also be acquired, for example, due to severe myopia in old age.
Classification
Modern medicine identifies several types of peripheral vitreochorioretinal dystrophy of the retina:
- Lattice. The most common type of pathology, which is most often inherited and is diagnosed mainly in men. With lattice PVCRD, degenerative changes occur in the upper outer quadrant of the fundus in the form of a lattice of empty vessels, between which cysts, tears and thinned walls of the retina are visible. With this form, both organs of vision are most often affected, and retinal detachment is observed.
- Frost-like. Degenerative changes have the appearance of empty vessels, between which there are pigment spots and foci of degeneration, similar to snow flakes. This form of the disease is hereditary and is characterized by symmetrical damage to both eyes. It is characterized by a long course and a reduced likelihood of retinal breaks.
- "Trace of the snail" . Dystrophic changes have the appearance of shiny white ribbon-like stripes with multiple holes and areas of thinning, reminiscent of a snail's footprint. The pathology is accompanied by large ruptures.
- "Cobblestone pavement" . Distant areas of the peripheral retina are affected, most often in the lower parts of the right or left eye. Degenerative changes take the form of individual white spots surrounded by pigment spots.
- Small cystic . Dystrophic processes are observed in the extreme parts of the periphery and take the form of multiple round red cysts that can merge to form large formations. Mechanical damage provokes rupture of cysts.
Sometimes a form of PVCRD is diagnosed as retinoschisis - a hereditary retinal separation that occurs as a result of age-related changes or against the background of myopia.
Causes of the “invisible danger”
The peripheral zone of the retina (retinal membrane of the eye) is practically invisible during a routine ophthalmological examination of the fundus, so very often this disorder is diagnosed already at the stage of pronounced clinical symptoms and complications, which negatively affects the prognosis.
Important! Dystrophy (or degeneration) of the peripheral portion of the retinal membrane occurs quite often, and the pathology affects both people with visual impairment and absolutely healthy people.
The causes of the disease are very diverse and not fully understood. The main one is a violation of normal blood circulation in the eyeball. For example, in people with myopia (myopia), due to the irregular shape of the eye (increase in its length), the membranes of the eye are stretched in the periphery, metabolic disorders occur, which are accompanied by changes in hemodynamics and cause peripheral tissue degeneration. This is why people with myopia are more likely to develop peripheral retinal dystrophy than people with other types of refraction.
The problem can occur at any age and is observed equally often in both men and women. There are many factors predisposing to the disease, including: genetic predisposition, myopia of any degree, inflammatory eye lesions, traumatic brain injuries and injuries to the organ of vision. Among general somatic diseases, it is worth noting diabetes mellitus, arterial hypertension, systemic atherosclerosis, past generalized infections and intoxications, and autoimmune lesions.
Ophthalmoscopic picture
Under the influence of trigger factors (physical activity, sudden changes in atmospheric pressure, vibration, etc.) in areas where the retina is thinned and degeneratively changed, ruptures and then detachment of the retinal membrane may occur.
An increased risk of developing peripheral dystrophy is also observed during pregnancy. Against the background of hormonal changes in a woman’s body, various ophthalmological changes occur, which, in the presence of initial myopia, can contribute to its progression and the development of degenerative processes in the peripheral zone of the retina.
Diagnostic methods
Peripheral vitreochorioretinal dystrophy is asymptomatic for a long time, which is why it is often diagnosed in the presence of large tears and significant deterioration of vision. It is impossible to detect PVCRD using a routine examination of the fundus, so ophthalmoscopy is performed with maximum pupil dilation and using a special Goldmann lens, which allows for a detailed examination of the most distant parts of the retina.
Read in a separate article: Macular degeneration of the retina: what is it, dry and wet forms
In addition, the following diagnostic measures can be carried out:
- perimetry;
- sclerocompression;
- visometry;
- refractometry;
- optical coherence tomography;
- EFI;
- Ultrasound.
Some modern clinics have special equipment that allows you to study the periphery of the retina in color, detect areas of rupture and estimate their size as accurately as possible.
Disease prevention
Important! Prevention of complications in the form of rupture or detachment during PCRD primarily involves timely diagnosis, which should be carried out by persons at risk.
Such patients need to undergo regular ophthalmological examinations (at least once or twice a year).
Persons at risk include:
- aged people;
- pregnant women (examination for PCRD in this case should be carried out at the very beginning and at the end of pregnancy);
- people with myopia;
- persons with a genetic predisposition to the disease;
- patients with diabetes mellitus and other ailments leading to circulatory disorders in the peripheral system.
Such persons require periodic examination of the fundus .
This allows you to prevent the onset of the development of the disease and perform timely surgical intervention, as a result of which the risk of developing PCRD can be reduced or completely eliminated.
Drug treatment of PVCRD
At the initial stages of development of peripheral vitreochorioretinal dystrophy, as well as several months after laser intervention, drug therapy is prescribed, aimed at improving material metabolism and compensating for degenerative processes. The following medications may be prescribed for the treatment of PVCRD:
- Riboflavin;
- Trimetazidine;
- Taurine;
- Nicergoline;
- Pentoxifylline;
- Atropine;
- Tropicamide.
To achieve the best effect, the ophthalmologist prescribes several drugs at once, the combination of which can eliminate degenerative processes, prevent complications and restore visual functions.
An effective remedy for PVCRD are tablets with Spirulina platentis extract.
Physiotherapy
To achieve a better result and quickly eliminate degenerative processes, in addition to the main method of treatment, physiotherapy is prescribed to help strengthen the muscular system and normalize ophthalmotonus. The following physiotherapeutic procedures may be recommended:
- magnetic therapy;
- electrophoresis;
- electrical and photostimulation;
- laser stimulation.
Along with physical therapy, various computer programs may be prescribed. Amblyocor, visual gymnastics.
Physiotherapeutic procedures for PVCRD are low in effectiveness, so they must be combined with vitamin therapy.
Laser surgery
The best treatment method for PVCRD is laser coagulation of the retina, the essence of which is gluing the thinned areas of the retina or cutting off torn tissue. Laser coagulation is carried out on an outpatient basis under local anesthesia, its duration is no more than 20 minutes.
Laser intervention is effective and safe, the recovery period is quick and without complications. For the speedy formation of adhesions during the first 2 weeks after surgery, you should refrain from physical and visual stress, thermal procedures and taking alcoholic beverages and vasodilators.
Treatment of pathology
Treatment of PCRD is carried out primarily in order to eliminate the likelihood of retinal detachment.
The main procedure in this case is laser coagulation of a preventive nature , which affects areas adjacent to existing ruptures.
This makes it possible to achieve “gluing” or soldering of damaged areas .
Remember! This is an outpatient operation, which almost always has a favorable prognosis, but after such procedures it is important to follow the doctors’ recommendations regarding the rehabilitation period.
Otherwise, the process of formation of adhesions may proceed incorrectly and lead to certain postoperative pathologies.
In particular, you need to avoid heavy physical activity and stay at rest for as much time as possible.
Physical work, immersion under water, and no exposure to various types of vibrations and shocks are completely excluded. All sports are also excluded.
PVHRD during pregnancy
During the gestation period, the immune system weakens, as a result of which the likelihood of developing various degenerative processes increases. If a pregnant woman has been diagnosed with PVCRD of the eye, then laser coagulation is prescribed. In the absence of contraindications, the operation is possible at any time, but it is not recommended to do it later than 31 weeks. With this diagnosis, doctors in most cases recommend giving birth by cesarean section, since natural childbirth can cause retinal detachment.
Treatment
Dystrophy of the “snail track” type can only be eliminated with a laser, especially if there is retinal detachment. In order to stop the progression of the disease in time, you need to regularly visit the ophthalmologist’s office. This will help the doctor timely identify the initial signs of degenerative disorders and monitor their dynamics.
In most cases, laser coagulation provides a lasting positive effect, and the risk of postoperative complications is low. It is performed in a clinical setting using local anesthesia.
This procedure isolates damaged areas of the retina to prevent them from spreading to healthy tissue. In some cases, repeated laser coagulation is prescribed in order to consolidate the result.
Prevention
The prognosis for peripheral vitreochorioretinal dystrophy of the retina in most cases is favorable; after completing a course of treatment, degenerative phenomena disappear and vision is restored. PVCRD is asymptomatic and is often detected at an advanced stage. To avoid this, it is recommended to undergo an annual preventive medical examination with an ophthalmologist and take the following preventive measures:
- avoid excessive visual strain;
- control blood sugar levels;
- Check your blood pressure regularly and stabilize it if necessary;
- Healthy food;
- to refuse from bad habits;
- to live an active lifestyle;
- promptly treat concomitant diseases;
- strengthen the immune system.
If degenerative processes have already occurred, then it is necessary to avoid physical overload, vibration exposure and extreme sports. Timely treatment can help avoid severe complications.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Occurrence of disease
Peripheral retinal dystrophy is most often diagnosed in patients suffering from myopia. This feature is explained by the fact that with myopia, the length of the eyeball increases. Because of this, the retina is stretched and its thickness becomes smaller. The risk group includes people who have reached old age.
This group also includes people suffering from diabetes, hypertension, and atherosclerosis. As a result of medical research, it was revealed that bad habits, poor diet and daily routine also play a significant role in the formation of the disease. There are often cases when the disease is hereditary.
It is on the periphery of the retina that dystrophic (degenerative) processes often develop