The retina, like any other organ, is supplied with blood through microcirculation. This is a small plexus of vessels through which blood flows along with oxygen, vitamins, nutrients, trace elements, and minerals.
Without this action, metabolic processes in the retina will decrease, which will lead to a lack of tissue renewal. Additionally, hypoxia occurs due to the lack of oxygen supply. Gradually, the affected area begins to peel off, and vision function suffers. To avoid complications, it is necessary to identify the condition in time and carry out treatment.
Causes of angiosclerosis
There are various diseases in which damage to the vascular endothelium of the eyes develops:
- Cardiovascular disorders, which cause increased blood pressure. If it manifests itself in the area of the retina and fundus of the eye, the pathology manifests itself quickly. An ophthalmologist may suspect systemic disease in the early stages. Subsequently, high pressure causes the vascular wall to lose its elasticity and the capillaries become tortuous. Thickenings and narrowings form along the entire length of the vessel, and it becomes uneven. When examined, the capillaries become silvery.
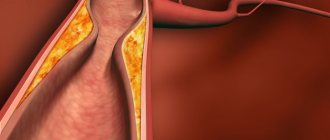
- Violation of lipid metabolism, resulting in the formation of atherosclerosis. Plaques move throughout the vascular network and penetrate the microcirculation of the eyes. For this reason, the endothelial wall becomes golden in color. If fatty deposits reach the macula, the patient's vision is deformed until it disappears completely.
- Hyperglycemia in diabetes mellitus. This is one of the forms of complications from the disease. Plaques are formed, consisting of fats and carbohydrates, which penetrate the microcirculation of the eyes.
- Injuries to the eyes or head. Vascular damage and bleeding occur.
- Cardiovascular diseases, as a result of which blood flows to the organs of vision in reduced quantities.
- Consumption of alcohol, cigarettes, drugs. Promotes deterioration of blood vessels.
Angiosclerosis is not an independent pathology. It is caused by systemic diseases, so it becomes a complication of them.
What is the disease and why is it dangerous?
Angiosclerosis is one of the pathologies of the vascular walls that cover the fundus of the eye. With the disease, the walls of blood vessels become dense and thickened, which leads to disruption of the blood supply to the membrane. The result is the formation of retinal edema.
Angiosclerosis is one of the stages in the progression of retinopathy in humans, characterized by damage to the retina of the eyeball. The disease is dangerous due to the fact that its further progression can cause complications - swelling of the retina, hemorrhage into it and the vitreous body. Such severe pathologies against the background of angiosclerosis are also possible, such as ischemia of the nerve endings of the retina and the formation of blood clots in the veins, as well as in the main artery.
The disease can cause a person to develop blindness. Angiosclerosis has a code according to ICD 10 under the designation H35 “Other diseases of the retina.”
At-risk groups
Not all patients develop the disease. Certain prerequisites are required for its formation. Therefore, the risk group includes the following categories of patients:
- diabetics;
- hypertensive patients;
- patient with cardiovascular disorders;
- patients exposed to head injuries;
- persons with lipid metabolism disorders;
- patients with atherosclerosis;
- persons who use drugs, cigarettes, alcohol.
It is recommended that the above categories of patients undergo periodic examination by an ophthalmologist. Based on the state of the microvasculature in the eye area, more serious systemic disorders can be identified.
Symptoms of atherosclerosis
Non-specific symptoms of atherosclerotic manifestations in the eye area are characteristic. The patient may suspect visual impairment based on the following signs:
- the appearance of non-existent circles, spots, lines before the eyes;
- pain in the head or eyes that occurs at rest or during physical activity;
- decreased visual acuity, double vision;
- headache, dizziness, nausea;
- deterioration of lateral vision, loss of any area from visibility;
- changes in pupil accommodation when exposed to bright light or in the dark.
Since the condition in most cases is caused by systemic diseases, additional symptoms appear that are characteristic of a particular disease. Therefore, a comprehensive examination of the patient using instrumental and laboratory examination methods is necessary.
Diagnosis of angiosclerosis
To make an accurate diagnosis, it is necessary to use a set of diagnostic measures:
- Anamnesis collection. This is data collected from the words of the patient or his close relatives. Complaints and disturbing symptoms are indicated. Based on them, the doctor selects further diagnostic procedures.
- Fundus examination. To do this, a solution is first instilled into the eyes, which eliminates the accommodation of the pupil. The condition of the lens, eye chambers, retina, and microvasculature vessels is examined.
- Measuring ocular vessels using fluorescein angiography. Their condition, degree of patency, and wall quality are assessed. The doctor can detect a violation of the tortuosity of the capillaries, swelling of the nerve tissues, disruption of the choroid plexuses, and changes in the lumen inside the capillary. The technique is carried out by introducing a drug that has fluorescence (glow). The substance moves along the capillary, determining the location of narrowing and expansion of the walls.
- MRI, CT. Used to confirm the diagnosis obtained from previous methods. The condition of the choroid plexus is assessed not only in the eyes, but also in other organs.
- Lab tests. Donate blood for a lipid profile. The amount of fat in the blood is detected. Using the technique, atherosclerosis can be suspected. Check your glucose if you suspect diabetes.
Diagnostic data allows you to confirm or refute the presumptive diagnosis.
Diagnostics of the fundus and retina
The doctor begins diagnosing vascular disease of the eyes by studying the history of the disease, external examination and interviewing the patient. Next, the ophthalmologist prescribes an additional examination. A biochemical blood test will show the level of low-density lipoprotein, which indicates cholesterol levels in the blood.
An ophthalmological examination may include several types of diagnostics that determine the condition of blood vessels, retina, vitreous body, lens, and optic nerve.
A simple way to examine the fundus is to use drops that dilate the pupil. However, this method using mydriatic drugs does not give the doctor a complete picture; some parts of the retina remain unstudied.
For detailed and accurate diagnostics, computer technology, MRI, ultrasound, ECG and other techniques are used:
| Diagnostic methods | a brief description of |
| Tonometry | Using a tonometer device to determine pressure levels inside the eye. |
| Electrophysiological study of the eye | EPI allows you to examine and evaluate the performance of the optic nerve, the inner lining of the eyeball, and the visual area of the cerebral cortex. |
| Visometry | A procedure used in ophthalmology using a table to determine visual acuity. |
| Computer perimetry | Visual field testing is a quick, accurate and painless examination technique with which the doctor can determine the exact location and extent of the lesion. |
| Coherence tomography |
eyes
Treatment of angiosclerosis
To prescribe treatment, confirmation of the diagnosis is necessary.
For each cause of the disease there is its own specific therapy. The course and dosage is selected individually for each patient. It is forbidden to select treatment on your own, as this can have irreparable consequences for the body.
To improve the quality of blood circulation in the eye area, the following medications are used:
- helping to increase the amount of plasma in the blood;
- reducing the number of platelets;
- vascular wall protectors;
- reducing intraocular and vascular pressure;
- helping to accelerate metabolism, due to which tissues are renewed;
- products that help saturate eye tissue with vitamins, nutrients, trace elements, and minerals.
The drugs from the above list belong to conservative therapy. But if it does not produce an effect, the doctor may prescribe a laser coagulation procedure. This is a special device that locally eliminates accumulated blood. With its help, local blood supply and oxygen delivery to tissues are improved.
Surgery is rarely used as it can cause complications during the procedure.
Complications of angiosclerosis
Disruption of the structure in the vascular endothelium without treatment can lead to complications. Some of them are fixable, others are irreversible:
- Retinal disinsertion. This is a condition in which microcirculation is disrupted and the tissue loses its functionality. A decrease in visual acuity gradually develops up to complete loss. The retina gradually separates from the membrane of the eye.
- Optic nerve atrophy. The process occurs due to a decrease or complete absence of blood supply to these tissues. The signal received from the organs of vision ceases to be sent to the brain, resulting in blindness.
- Necrosis of eye tissue. Due to the blood supply, the structure of the eyeball is nourished. In the absence of nutrients and oxygen, cells gradually die.
The sooner a developed complication is detected, the more effective the therapy will be. Therefore, people who are at risk need to be periodically observed by an ophthalmologist to prevent irreversible processes.
The most negative complication for a person is complete loss of vision, which will be impossible to restore.
Forecast
The prognosis of the condition depends on the stage at which it was detected. If the doctor suspects defects of the retina and microvasculature in the early stages, they are completely restored after treatment. In this case, the prognosis is favorable.
Without treatment, eye tissue gradually dies. Retinal detachment and optic nerve atrophy occur. If the disease was detected in the final stages, the prognosis for the patient is unfavorable. He will completely lose his sight. If the disease is caused by systemic disorders, it is important to prevent further spread of the process, since the death of the patient is possible.
Stages of pathology
Hypertensive angiosclerosis of the retina goes through the following stages:
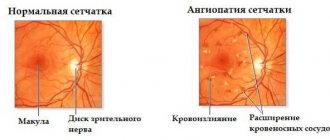
- Development of angiopathy. The vessels change under the influence of frequent pressure surges, but their structure is not yet damaged. The stage is reversible.
- The development of angiosclerosis, accompanied by spasms of the vascular walls. When veins and arteries cross, a bend occurs in the former. The vessels cease to be elastic.
- Development of angioretinopathy . Retinal swelling appears and hemorrhages occur. Cloudiness occurs in certain areas of the shell. Visual acuity decreases.
- Neuroretinopathy . The optic disc swells along with the retina. Hemorrhages are frequent.
In humans, the disease can progress quickly. Within a year, it can reach the final stage, at which complete loss of vision occurs.
Prevention
To prevent the development of atherosclerosis in the area of the blood vessels of the eyes, it is necessary to adhere to certain rules:
- Periodic vision examination by an ophthalmologist. Diagnostic tests and laboratory procedures must be performed.
- Treatment of systemic diseases in a timely manner. It is recommended to adhere to the dosages prescribed by your doctor.
- Complete healthy nutrition. With the development of atherosclerosis, it is recommended to use a diet that excludes fatty, spicy, and fried foods.
- Keep high blood pressure under control. Use antihypertensive drugs to avoid eye complications.
- Use hypoglycemic agents and follow a diet to prevent the development of complications from diabetes.
Angiosclerosis is a dangerous condition that can lead to complete blindness. There are various reasons for its appearance that need to be eliminated in time. All drugs and their dosages are selected by an ophthalmologist or therapist individually for each patient. It is recommended to periodically check vision and fundus to prevent progression of the process.
Causes of atherosclerosis of the ocular vessels
Among the most common causes of the disease, pathological changes are observed in the form of:
- Arterial hypertension;
- Generalized atherosclerosis.
With high blood pressure, the vascular walls throughout the body are first affected.
Ophthalmologists are among the first to detect hypertension by changes in the circulatory network of the eye, since one of the accessible places to recognize these changes is the fundus of the eye.
Having discovered vasospasm or atherosclerosis in the vessels of the nerve membrane of the eye, they firmly confirm hypertension.
The cause of hypertension and other diseases associated with disorders of the vascular system is elevated plasma cholesterol over a long period. The causes of retinal atherosclerosis are fatty deposits in the vessels, which interferes with normal blood circulation.
This can happen for several reasons:
- Due to sleep disturbances, constant overwork or being under stress;
- Lack of physical activity and, as a rule, a decrease in metabolic processes in the body;
- The cause may be excess weight, fat accumulation and metabolic disorders;
- Smoking and alcohol, which are provocateurs of vascular spasms and their damage;
- Wrong foods that contribute to the development of vascular plaques due to “bad” cholesterol in large quantities.
With atherosclerotic lesions, plaques form that interfere with normal blood circulation, and oxygen ceases to flow sufficiently. And this is a direct path leading to the formation of blood clots, poor coagulation and serious pathology of the vascular system. As a result of these negative manifestations, the fundus of the eye, its stem branches and the central vein become easily vulnerable.
Limited blood supply atrophies retinal tissue, damages small capillaries, forms blood clots and reduces the elasticity of the arteries.
Sometimes the disease is not detected for years, since the signs of the disease are often concomitant. The clinical picture is often expressed by spasms in the circulatory system of the eye, blockage in thin arteries and their rupture. Therefore, often, the disease can only be identified during a crisis period, with a sharp drop in vision and the formation of edema.