Most people who are born with good vision take it for granted and usually think little about its value. A person usually begins to appreciate vision when he encounters the first limitations of his capabilities due to loss of vision.
The very fact that the ability to see clearly is lost often upsets a person, but, as a rule, not for long. If preventive measures or efforts to preserve vision are undertaken for some time, the situation is soon smoothed out by spectacle correction or lenses, and prevention stops.
Perhaps only expensive surgical treatment forces citizens to take more seriously the preservation of the results achieved through surgery. What are the causes of decreased vision? Which situations can be resolved routinely, and which require an immediate visit to the doctor and emergency care?
Options for visual impairment
- Decreased visual acuity
- Double vision
- Lack of binocular vision
- Visual field pathologies
- Color vision disorders
- Blindness
Decreased vision clarity
The norm of visual acuity for children over the age of five and adults is 1.0. This means that the human eye is able to clearly distinguish two points located at a distance of 1.45 meters, provided that the owner is looking at them at an angle of 1/60 degree.
Clarity of vision is lost with myopia, farsightedness, and astigmatism. These disorders relate to ametropia, that is, a condition where the image is projected outside the retina.
Myopia
Myopia or myopia is a condition where light rays project an image in front of the retina. At the same time, distance vision deteriorates. Myopia can be congenital (due to an elongated shape of the eyeball, when there is weakness of the ciliary or extraocular muscles) or acquired. Myopia is acquired as a result of irrational visual stress (reading and writing in a lying position, failure to maintain the best vision distance, frequent eye fatigue).
The main pathologies leading to the acquisition of myopia are spasm of accommodation, increased thickness of the cornea, traumatic dislocations and subluxations of the lens and its sclerosis in the elderly. Myopia can also be of vascular origin. Weak myopia is considered to be about minus three. Moderate - from minus 3.25 to minus six. Anything more is severe myopia. Progressive myopia is called when its numbers constantly increase against the background of stretching of the posterior chambers of the eye. The main complication of severe myopia is divergent strabismus.
Farsightedness
Farsightedness is the inability to see close up normally. Ophthalmologists call it hypermetropia. This means that the image will be formed behind the retina.
- Congenital farsightedness is natural and is caused by the small longitudinal size of the eyeball. It may disappear as the child grows or may persist. In cases of abnormally small eye size, insufficient curvature of the cornea or lens.
- Senile (when vision declines after 40) is a consequence of a decrease in the ability of the lens to change its curvature. This process goes through the stage of presbyopia (first temporary in people from 30 to 45), and then permanent (after 50-60 years).
Age-related deterioration of vision after 65 occurs because the accommodation of the eye (the ability to adjust the curvature of the lens to the needs of a person) is practically absent.
Both the lens (losing elasticity or changing curvature) and the ciliary muscle, which is no longer able to bend the lens normally, are to blame for this. In the early stages, presbyopia can be compensated for by bright lighting. It doesn’t help in the later stages either. The first manifestations of the pathology are the inability to read close typeface within the distance of comfortable vision (25-30 centimeters), blurriness of objects when quickly moving the gaze from distant objects to close ones. Farsightedness can be complicated by increased intraocular pressure.
Astigmatism
Astigmatism in a primitive explanation is different visual acuity horizontally and vertically. In this case, any point is projected in the eye so that it turns out to be a blurry ellipse or figure eight. The pathology is associated with a violation of the shape of the lens, cornea or the entire eye. In addition to blurred vision, astigmatism is accompanied by double vision of objects, their blurring, and rapid eye fatigue. It can be combined with myopia (complex myopic) or farsightedness (complex hyperopic), and can also be mixed.
Working hard
— Many people believe that glasses or lenses are needed when it is impossible to do without them, and in other cases “the eye must work.”
- This is wrong. Incorrect vision correction or non-use of correction means, overstrain of the eye muscles can lead to deterioration of vision. According to WHO, uncorrected refractive errors are the most common cause of decreased vision and the second most common cause of low vision (persistent vision loss).
All-seeing eye. Let's analyze popular statements about vision Read more
— At what age does vision usually deteriorate?
- More often during the development of the body and eyes, as well as during their aging. In children and adolescents (up to 18–20 years of age), vision may deteriorate due to the progression of myopia. And after 40–45 years, almost all people begin to complain of decreased near vision due to age-related farsightedness. Changes in vision are also possible in later life, when age-related changes or eye diseases may appear due to aging processes.
— There are many methods (both medical and folk) that are recommended to improve vision. Is it possible to cure myopia?
— The issue of increasing visual acuity can be resolved after examination by a specialist and finding out the cause of decreased vision. If there are no eye diseases, in particular diseases of the retina or optic nerve, cataracts, etc., and decreased vision is associated with refractive error (myopia, farsightedness, astigmatism), vision can be improved with the help of properly selected glasses and contact lenses. For myopia, not only vision correction methods are used, but also eye treatment methods. However, it is not yet possible to completely cure myopia.
Pediatric ophthalmologist: “A computer is safer for the eyes than a smartphone” Read more
— What is considered more effective?
— Each method has its own advantages. Glasses are a simple, reliable and affordable method. Today, when there are no problems with choosing frames, glasses can be considered as a fashion accessory.
The popularity of contact lenses is due to their wearing comfort and obvious advantages. They do not change appearance, provide freedom of movement (for example, when playing sports), increase and normalize visual functions.
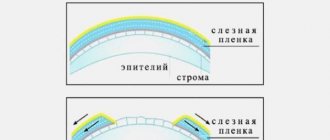
In some cases, for example, to stop the progression of myopia in children, so-called night (orthokeratological) lenses are used. These are hard lenses of a special design that change the profile of the cornea and its refractive properties. The main advantage of the method is that the patient wears the lenses only while sleeping (however, wearing them at night increases the risk of possible complications). This method requires careful selection of patients and selection of lenses, constant monitoring of eye condition. In addition, the long-term consequences of using these lenses have been little studied, so they should be recommended to those patients who, for various reasons, cannot use traditional means of vision correction - glasses and contact lenses. It is also impossible to say unequivocally that the use of night lenses stops the progression of myopia.
Click to enlarge
Double vision
This condition is called diplopia. With it, a visible object can double horizontally, vertically, diagonally, or two images are rotated relative to each other. The oculomotor muscles are to blame for everything, the work of which is not synchronized and which do not allow the eyes to converge to the target object as they should. Often, damage to the muscles themselves or the nerves that supply them in systemic diseases begins with diplopia.
- The classic cause of double vision is strabismus (convergent or divergent). At the same time, a person cannot manage to direct both central foveae of the retina strictly along the course.
- The second typical picture is alcohol poisoning. The toxic effect of ethanol disrupts the combined movement of the eye muscles.
- Temporary double vision has been played out many times in movies and cartoons: when a hero is hit on the head, not only do sparks fly from his eyes, but the picture before his eyes moves apart.
These are all examples of binocular (two eyes) diplopia.
- Double vision in one eye can develop when the cornea is too convex, the lens is subluxated, when the calcarine groove of the occipital region of the cerebral cortex is affected.
Factors Contributing to Unexpected Blindness
— Loss of vision (amorosis in Latin) can be a consequence of deposits on the lens or disruption of the functioning of the lens. Diseases of the eye retina also cause sudden blindness. Whatever the reason, people with sudden deterioration of vision should be immediately placed under therapy. Data collected in the first minutes after the onset of sudden blindness will help establish the correct diagnosis.
— A sudden deterioration in vision in one eye can be a consequence of retinal disease, as well as a broken eye nerve. The reason for this is improper blood flow in the retina. Most often, it feels like part of the vision has been covered with some kind of canvas. So in patients with a similar illness, temporary weakness or complete temporary failure of one or two limbs is observed. The duration of loss of limb function can last from one hour to a day.
- In almost ninety percent of cases, a sudden deterioration in vision occurs due to improper functioning of the heart; a retinal embolism occurs due to a plaque inside the aortic arterial system. Also, sudden blindness in one eye is a symptom of an upcoming stroke. In such situations, it is necessary to immediately examine the patient to prevent a stroke. It is necessary to take one hundred to three hundred grams of aspirin to prevent a stroke.
You may be interested in Your child’s eyes are watering: reasons and what to do
— In young people, migraine may be the cause of temporary, sudden blindness in one eye. The effect of migraine on vision occurs through a migraine aura. However, in order to avoid a stroke, it is necessary, with the help of a special examination, to exclude unusual pathologies in the arterial system and cardiovascular system from the list of probabilities.
Neuropathy
Neuropathy of the nerves of the eyes occurs as a result of improper blood flow to the nerve. Due to the lack of blood from the occipital cerebral region to the eye, the organ begins to gradually lose its functionality. This disease manifests itself as visual impairment in one eye and is not accompanied by pain. Symptoms include swelling and abnormal growths around the optic disc.
Very often, ischemic neuropathy is detected in people with arterial pathologies and diabetes. In old age, the cause of ischemic neuropathy can be temporal arteritis. A symptom of this disease is the absence of blood pulsation in the artery passing through the temple.
It is much less likely to encounter such a type of ischemic neuropathy as ischemic neuropathy of the occipital lobe. The cause of this type of neuropathy is anemia and low pressure in the blood vessels. Due to an excessively sharp drop in blood pressure, an attack of the optic disc nerve occurs.
There is also a known disease that results in a sudden deterioration of vision, this is toxic neuropathy. The cause of toxic neuropathy is a high content of methyl, ethyl, and carbon monoxide in the blood. Thus, this disease can develop with excessive alcohol consumption.
Optic neuritis
This disease is an inflammatory process of the optic nerve, especially its retrobulbar part, thereby sharply or gradually worsening vision. Due to the fact that the optic nerve itself is located deep in the orbit, inflammatory processes are difficult to detect. There are no symptoms on the optic nerve head. With this disease, vision loss occurs at a young age and a relapse of the disease may occur. Methylprednisolone will help restore inflamed areas of the optic nerve. It must be administered intravenously.
Intracranial pressure
Loss of vision, especially sudden loss, can be a consequence of increased intracranial pressure. This is accompanied by short-term losses of visual abilities, which usually occur when changing body position. Loss of vision in this case continues for two to three minutes. With this disease, intravenous administration of methylprednisolone into the patient’s body will help. Since the disease can cause serious complications, it is necessary to consult a specialist.
You may be interested in Eye burns: causes, symptoms, treatment
Infarction of blood vessels in the posterior part of the brain as a factor in vision loss
Acute sudden blindness is a consequence of an infarction of the blood vessels in the posterior parts of the brain. The so-called basilar artery becomes blocked, or the pressure of the blood vessels sharply decreases, resulting in rupture of the blood vessels.
With this type of disease the following may occur:
- dizziness, - double vision.
Blindness in this case is called cortical and differs from bilateral blindness, which occurs when the optic nerve is damaged, the reaction of the pupils to external stimuli is preserved. In many situations, patients deny the onset of visual impairment and state that the lights are off and it is very dark around.
Hysteria as a cause of vision loss
Sudden blindness also has a psychogenic background and is a consequence of acute psychosis expressed in hysteria. Patients based on hysteria, in many cases who are young ladies, declare that the world has plunged into darkness. Psychosomatic symptoms will go away after calming down; it is necessary to monitor the patient and avoid nervousness and stressful situations.
Just as with an infarction of the posterior lobes of the brain, with hysteria the reaction of the pupils is absolutely normal. There are no table symptoms. Due to the calm and even overly relaxed state of consciousness of patients with hysteria, it is very difficult to detect this illness before the onset of blindness.
Binocular vision disorders
The ability to see with two eyes allows a person to expand the field of vision, improve its clarity by 40%, see the volume of an object, and evaluate its approximate size and shape. This is stereoscopic vision. Another important purpose is distance estimation. If one eye does not see or the difference in the eyes leaves several diopters, the weaker eye, which can cause diplopia, begins to be forcibly switched off by the cortex from the vision process.
First, binocular vision disappears, and then the weak eye may go completely blind. In addition to myopia and farsightedness with a large difference between the eyes, uncorrected astigmatism also leads to the subfrontal phenomenon. It is the inability to estimate distance without glasses correction that forces many to use glasses or contacts while driving.
More often, binocular vision is absent with strabismus. To be honest, almost no one has an ideal balance between the position of the eyes, but since even with deviations in muscle tone, binocular vision is preserved, this does not require correction. If convergent divergent or vertical strabismus deprives a person of vision with both eyes, he has to undergo surgery or, at best, wear glasses.
Causes of gradual vision loss
There are many organs and tissues in our body that need to be monitored and cared for. Many people periodically undergo rejuvenation procedures and various treatments for the digestive organs, but most do not care about maintaining vision and eye condition. Eyes are one of the most important organs that provide us with the important ability to see. With the help of our eyes we can observe the world around us and receive information. This is such an ordinary thing that people don’t even always understand the meaning of this feeling. It is necessary to take care of the eyes on an equal basis with other organs, and perhaps even more.
You may be interested in Iridocyclitis: causes, symptoms, treatment
The modern world is full of computers, televisions, advertising monitors, various sources of bright light, which have an irritating effect on the eyes and thus vision deteriorates over time. If some people, at the initial signs of vision deterioration, take measures to restore and improve the health of their eyes, many do not pay due attention and continue to live. Such people are advised to take care of their eyes more often so that they do not have to deal with their treatment and restoration of vision.
Of course, in most cases the cause of visual impairment is:
- computers, - televisions, - incorrect reading, - constant exposure to bright light.
However, these reasons cause only partial impairment of vision, which can be restored with standard procedures. Long-term visual impairment has much deeper reasons. Therefore, you should not postpone the examination and subsequent eye treatment.
Distortion of visual fields
The part of the surrounding reality visible to the fixed eye is the field of vision. In spatial terms, this is not a field at all, but rather a 3D hill, at the top of which visual acuity is highest. Worsening towards the base, more along the slope near the nose and less along the temporal. The field of vision is limited by the anatomical protrusions of the facial skull, and at the optical level by the capabilities of the retina.
For white color, the normal visual field is: inward - 55 degrees, upward - 50, downward - 65, outward - 90. (see picture of the visual field).
For one eye, the field of view is divided into two vertical and two horizontal halves.
Visual fields can change in the form of scotomas (dark spots), in the form of concentric or local narrowings (hemianopsia).
- A scotoma is a spot in which nothing is visible if it is absolute or blurred if it is relative. There may also be mixed scotomas with absolute blackness inside and relativity along the periphery. Positive scotomas are felt by the patient. Negative ones are revealed only during examination. An example of a physiological scotoma is the Mariotte blind spot in the outer part of the visual field (projection of the optic disc, where there are no cones and rods).
- Optic nerve atrophy - loss in the central part of the field indicates macular degeneration of the retina or optic nerve atrophy, often age-related.
- Retinal detachment - if, as if a curtain were blocking off the peripheral part of the field of vision from any side, it is most likely a retinal detachment (then distortion of lines and shapes, and image floating may be observed). The causes of detachments are a high degree of myopia, trauma or degeneration of the retina.
- Bilateral loss of the outer halves of the fields is a common sign of a pituitary adenoma that interrupts the optic tract at the site of decussation.
- With glaucoma, half of the fields closer to the nose fall out. They can be combined with a rainbow when looking at the light, or mist in the eyes. The same loss occurs with pathologies of uncrossed optic fibers in the area of the cross (for example, with an aneurysm of the internal carotid artery). Read more about the symptoms of glaucoma.
- Cross loss of parts of the fields (for example, internal on one side and external on the other) is more often observed with tumors, hematomas or inflammatory processes in the central nervous system. In addition to half the fields, quarters of them may also fall out (quadrant hemianopsia).
- If the prolapse appears in the form of a translucent curtain, this is evidence of a change in the transparency of the media of the eye: the lens, cornea, vitreous body.
- Retinal pigmentary degeneration causes concentric narrowing of the visual fields or tubular vision. At the same time, high visual acuity is maintained in the center of the field, and the periphery practically disappears. If concentric vision develops evenly, then glaucoma or cerebrovascular accidents are most likely to blame. Concentric narrowing is also characteristic of peripheral chorioretinitis (inflammation of the posterior retina).
Causes of visual impairment in one eye and treatment.
Most eye diseases cause decreased vision in both eyes. However, there are times when it only gets worse on one. It can cause serious illness at any age. At the first symptoms, you should consult a doctor so as not to start the disease, if it exists.
Let's try to list the main causes of unilateral visual impairment. Once you know them, you will understand how to save yourself from the consequences.
First, unilateral vision impairment can cause retinal detachment. The disease manifests itself in the appearance of spots or veils before the eyes. This occurs after a tear in the peripheral zone of the retina, as a result of which intraocular fluid flows into these zones, and the retina detaches, which is caused by injury, heavy lifting, and myopia. In this case, surgery may be necessary.
Secondly, Leber syndrome causes loss of vision in one eye, in which the cells of the retina and optic nerve are destroyed. A person develops a “blind spot” first in one eye, and subsequently in the other. This is a genetic disease, but there are also factors that lead to it, for example, alcohol and tobacco abuse, nervous shock, and previous infections. An effective treatment method has not yet been developed.
Thirdly, this is glaucoma or its closed-angle form. It is accompanied by pain in the eye, redness of the white, intraocular pressure, as well as nausea and vomiting. When treating, the first step is to reduce intraocular pressure.
Next is cataract. Loss of vision in one eye often indicates some pathology, including cataracts. It usually appears with age, but can also occur as a result of injury or illness. They get rid of it through surgery. Also, vision may decrease in one eye due to strabismus. The muscles in one eye work less well, resulting in decreased vision. It is usually typical for children and it is easier to get rid of it in childhood.
The next reason is amblyopia, in which one eye is practically not involved in the visual process. It develops against the background of strabismus or congenital pathology of the lens or cornea. Also typical for children. At the same time, the child rarely complains about a defect, which is easier to correct in childhood.
And finally, loss of vision is caused by injuries of a mechanical or chemical nature: debris or household chemicals that get into the eye, damage from glass or a blunt object, burns and frostbite.
There are many reasons, and the symptoms are varied. The main conclusion to be drawn is this: when the first signs of deterioration appear, consult an ophthalmologist. Professional and timely diagnosis will save your vision and prevent serious undesirable consequences.
Deviations in color perception
- Color blindness is a congenital defect in distinguishing between red and green that is not recognized by the patient. More often detected in men.
- Temporary shifts in the perception of white are a consequence of surgery to remove the lens affected by cataracts. Shifts towards blue, yellow, and red colors may develop, that is, white will be bluish. yellowish reddish, like an unregulated monitor.
- After cataract removal, the brightness of colors may also change: blue becomes more saturated, and yellow and red fade and become pale.
- A shift in perception towards long waves (yellowing, redness of objects) may indicate retinal or optic nerve dystrophy.
- Objects become discolored due to old degeneration of the macular region, which is no longer progressing.
Most often, color disturbances affect the central part of the visual field (within 10 degrees).
Causes of visual impairment
- Changes in the transparency of the eye media (pathologies of the cornea, lens).
- Muscle pathologies
- Retinal abnormalities
- Optic nerve lesions
- Deviations in the cortical center
Normally, the transparent media of the eyeball (cornea, lens, vitreous body) transmit and refract light rays like lenses. With pathological infectious-inflammatory, autoimmune or dystrophic processes in these lenses, the degree of their transparency changes, which becomes an obstacle to the path of light rays.
Pathologies of the cornea, lens
Keratitis
Keratitis is inflammation of the cornea. Bacterial often becomes a complication of untreated conjunctivitis, a consequence of infection during eye surgery. Pseudomonas aeruginosa is especially dangerous, which has repeatedly led to cases of massive outbreaks of keratitis in ophthalmology hospitals with insufficient asepsis and antiseptics (more about Pseudomonas aeruginosa and its treatment).
- The pathology is characterized by clouding, ulceration of the cornea, pain and redness in the eye.
- Photophobia is also present.
- Lacrimation and decreased shine of the cornea up to the formation of an opaque cataract.
More than half of viral keratitis is caused by herpes (dendritic keratitis). In this case, a damaged nerve trunk is visible in the eye in the form of a tree branch. A creeping corneal ulcer is the result of a herpetic lesion or chronic injury to the cornea by foreign bodies. Amebic keratitis often leads to ulcers, which affects lovers of cheap, low-quality lenses and those who do not follow hygienic rules for using lenses.
When the eye is “burned” by welding or looking at the sun with an unprotected eye, photokeratitis develops. In addition to ulcerative keratitis, there is non-ulcerative keratitis. The disease can affect only the superficial layers of the cornea or be deep.
Corneal opacities are the result of inflammation or dystrophy; a cataract is a scar. Opacities in the form of clouds or spots reduce visual acuity and cause astigmatism. The thorn limits vision to light perception.
Cataract
Cataract is clouding of the lens. At the same time, metabolism is disrupted, structural proteins are destroyed, elasticity and transparency are lost. The congenital form of the disease is the result of viral, autoimmune or toxic influences on the fetus in utero or genetic pathology.
Cloudiness of the lens is acquired, as age-related dystrophy, the result of mechanical or chemical trauma, radiation exposure, poisoning with naphthalene, ergot, mercury vapor, thallium, trinitrotoluene). Posterior capsular cataract is the lot of people over 60 who quickly lose vision, nuclear cataract gradually increases the degree of myopia, age-related cortical cataract makes the surrounding blurry.
Vitreous opacification
Cloudiness of the vitreous body (its destruction) is perceived by the patient as threads or dots floating in front of the eye when moving the gaze. This is a consequence of thickening and loss of transparency of individual fibers of the vitreous body, which develop with age-related dystrophy, arterial hypertension and other vascular pathologies, diabetes mellitus, with hormonal changes or glucocorticoid therapy. Opacities are perceived in the form of simple or complex (webs, balls, plates) figures. Sometimes areas of degeneration are perceived by the retina, and then flashes appear in the eyes.
Treatment of short-term blindness
First of all, treatment of temporary vision loss is aimed at eliminating the cause that provoked the development of the disease.
Most often, with short-term blindness, the patient is prescribed to take special restorative vitamins. These include:
- Ascorbic acid. The drug contains vitamin C, which promotes collagen synthesis, regeneration of affected tissues and blood clotting.
- Retinol. This product contains vitamin A, which affects cell reproduction and growth.
- Thiamine. The main active substance is vitamin B1, which helps normalize eye pressure.
- Tocopherol. The medicine has the ability to prevent retinal detachment. The active ingredient of the drug is vitamin E.
In addition to vitamins, the doctor may prescribe special eye lotions based on beneficial substances and herbs.
Traditional medicine also offers treatment for temporary loss of visibility with the help of various medicinal plants, which are used in the form of solutions, infusions, decoctions, compresses and baths.
To ensure your vision always remains good, you need to visit an eye doctor several times a year.
If the disease takes you by surprise, it is better not to wait for it to go away on its own. If you do not consult a doctor in a timely manner, complications may develop, including complete loss of vision. In addition, as mentioned above, short-term blindness in most cases is only a symptom of a serious and dangerous disease.
By identifying the type of thrombosis, the doctor can make an accurate diagnosis. Based on the data obtained, the specialist determines the possible course of the disease and the possibility of restoring vision.
Most often, patients are diagnosed with vascular obstruction. Arterial blockage is less common. In case of vascular obstruction, the prognosis is very favorable, and the probability of maintaining vision is high.
The earlier a retinal infarction is diagnosed, the fewer cells have time to die. Sometimes a few minutes are not enough to be able to restore vision.
After 40–50 minutes of instant loss of vision, it can no longer be restored.
| No-shpa and papaverine | Help relieve vasospasm and reduce intraocular pressure. |
| Trental | Improves blood circulation. |
| Various thrombolytics | They clear the lumen of the arteries by dissolving blood clots. |
| Heparin and other anticoagulants | Reduce blood clotting (dosage must be agreed with your doctor). |
| Angioprotectors | Strengthens the walls of blood vessels. |
| Antibiotics | They allow you to rid the vessel of a clot of microbes that has blocked the lumen. |
| Diprospan and dexamethasone | Relieves swelling. |
| Cardiomagnyl and other antiplatelet agents | The platelets are not allowed to fuse. |
In case of acute vascular obstruction, eye injections are prescribed. They use means to dissolve the blood clot.
These medications include:
- fibrinolysin;
- urokinase;
- plasminogen;
- streptokinase;
- hemazu.
| HBO |
|
| Laser coagulation method |
|
Muscle pathologies
Vision depends on the ciliary and oculomotor muscles. Their dysfunction also impairs vision. The entire range of movements of the eyeball is provided by only six muscles. They are stimulated by 6, 4 and 3 pairs of nerves in the cranial region.
Ciliary muscle
The ciliary muscle helps the lens to bend, participates in the outflow of intraocular fluid and stimulates the blood supply to certain parts of the eye. Muscle function is disrupted by vascular spasm in the vertebrobasilar region of the brain (for example, vertebral artery syndrome in osteochondrosis), hypothalamic syndrome, spinal scoliosis and other causes of cerebral blood flow disorders. The cause may also be traumatic brain injury. This leads primarily to a spasm of accommodation, and then to the development of myopia. Some works by domestic ophthalmologists have revealed a relationship between injuries to the cervical region of fetuses during childbirth and the development of early forms of acquired myopia in babies.
Oculomotor nerves and muscles responsible for eye movement
The oculomotor nerves regulate not only the muscles that control the eyeball, but also the muscles that constrict and dilate the pupil, as well as the muscle that lifts the upper eyelid. Most often, the nerve suffers from microinfarction due to hypertension and diabetes. Damage to all nerve fibers leads to the following symptoms of visual impairment: divergent strabismus, double vision, drooping of the eyelid, dilation of the pupil without reaction to light, poor near vision due to accommodation paralysis, limitation of eye movements inward, up and down. Often, with strokes, nerve damage is included in the program of pathological syndromes (Weber, Claude, Benedict).
Abducens nerve damage
Damage to the abducens nerve (which can cause meningioma, internal carotid artery aneurysm, nasopharyngeal cancer, pituitary tumor, head trauma, intracranial hypertension, complicated otitis, central nervous system tumors, multiple sclerosis, stroke, vascular infarction along the nerve due to arterial hypertension or diabetes mellitus) prevents you from moving your eye to the side. The patient suffers from horizontal double vision, which intensifies when looking in the affected direction. In children, congenital lesions of the abducens nerve are included in the program of Mobius and Duane syndromes.
When the trochlear nerve is affected, double vision appears in the vertical or oblique plane. It intensifies when you look down. The head often takes a forced position (turning and tilting in the healthy direction). The most common causes of nerve damage are traumatic brain injury, microinfarction of the nerve, and myasthenia gravis.
Classification
The following types of blindness are distinguished:
- complete - as a rule, it is congenital;
- scotoma – partial (fragmentary) loss of vision;
- hemianopia – loss of up to half of the visual fields in each eye.
Color blindness is classified as a separate type of blindness, in which the patient cannot distinguish shades of colors.
Causes
Various pathological disorders can cause short-term blindness:
- increased intracranial pressure;
- vertebral artery thrombosis;
- benign or malignant intracranial neoplasms;
- acute glaucoma;
- retinal detachment;
- inflammation of the peripheral optic nerves;
- disruption of the central nervous system;
- diabetes;
- congenital or degenerative diseases, eye injuries;
- neovascular macular degeneration.
There are other causes of temporary blindness. Thus, during a hypertensive crisis and stroke, sharp and regular jumps in blood pressure can lead to partial or complete loss of vision. In this case, complex restorative treatment is required.
Retinal pathologies
- Retinal detachment (idiopathic, degenerative or traumatic) occurs at the site of membrane ruptures against the background of diabetic retinopathy, myopia, trauma, or intraocular tumor. Often the retina detaches after clouding of the vitreous body, which pulls it along with it.
- Spot degeneration, vitelline degeneration, macular degeneration are hereditary pathologies that are worth thinking about when a child’s vision declines very significantly in preschool age.
- Hydrocyanic dystrophy is typical for people over 60.
- Strandberg-Grönblad syndrome is the formation of stripes in the retina that resemble blood vessels and replace cones and rods.
- Angiomas are vascular tumors of the retina that occur in adolescence and lead to retinal tears and detachment.
- Varicose veins of the retina (Coats' retinitis) are dilation of the venous vessels, which leads to hemorrhages.
- Albinism with underdevelopment of the pigment layer of the retina gives a pink coloration of the fundus and discoloration of the iris.
- Thrombosis or embolism of the central retinal artery leads to sudden blindness.
- Retinoblastoma is a malignant tumor of the retina that grows into it.
- Inflammation of the retina (uveitis) causes not only blurred vision, but also flashes and sparks in the field of vision. Distortions in the shapes and outlines and sizes of objects may be observed. Sometimes night blindness develops.
Signs of optic nerve diseases
- If the nerve is completely interrupted, the eye on the affected side will go blind. His pupil narrows and does not react to light, but may narrow if shined into the healthy eye.
- If some of the nerve fibers are damaged, then vision simply decreases or loss of vision occurs (see distortion of visual fields).
- Most often the nerve is affected by injuries, vascular diseases, tumors, and toxic lesions.
- Nerve anomalies – coloboma, hamartoma, double nerve disc.
- Disc atrophy (against the background of multiple sclerosis, ischemia, trauma, neurosyphilis, after meningoencephalitis) causes a narrowing of the visual fields and a drop in its acuity, which cannot be corrected.
This and cortical disorders are discussed in the next two sections.
Prevention
To avoid ocular infarction, it is necessary to pay attention to preventive measures.
To do this you need:
- completely give up the smoking habit;
- avoid stress or at least reduce its duration to a minimum;
- do not allow the nervous system to overstrain;
- help prevent the occurrence of cardiovascular diseases and diabetes, and if they are present, be sure to be treated;
- eat foods rich in vitamins, add vegetables and fruits to your diet;
- prevent the formation of blood clots in the blood vessels of the eyes;
- use products that help regulate blood viscosity (only with a doctor’s prescription and under his supervision).
Temporary loss of vision
Eye fatigue
The most commonplace situation is called asthenopia. This is eye strain due to irrational visual load (for example, sitting for many hours in front of a monitor screen, TV, reading from a sheet in low light, driving a car at night). In this case, the muscles that regulate the functioning of the eye become overstrained. Pain in the eyes and lacrimation appear. It is difficult for a person to concentrate on small print or details of an image, and blurriness or a veil may appear before his eyes. This is often combined with a headache.
False myopia
Accommodation spasm (false myopia) often affects children and adolescents. Its clinical picture is similar to asthenopia. Transient visual impairment near or far is caused by fatigue and spasm of the ciliary muscle, which changes the curvature of the lens.
Night blindness - nyctalopia and hemeralopia
Deterioration of vision at dusk is a consequence of a deficiency of vitamins A, PP and B. This disease is popularly called night blindness, and its scientific names are nyctalopia and hemeralopia. At the same time, twilight vision suffers. In addition to hypovitaminosis, diseases of the retina and optic nerve can lead to night blindness. There are also congenital forms of pathology. At the same time, visual acuity weakens, color perception decreases, a person’s spatial orientation is disrupted, and visual fields are narrowed.
Vascular spasms
Transient visual disturbances may indicate vascular spasm in the retina or brain. Such situations are associated with hypertensive crises (sharp jumps in blood pressure), chronic cerebral circulatory disorders (against the background of atherosclerosis, vertebral artery syndrome, cerebral amyloidosis, blood diseases, vascular anomalies, vasculitis, venous hypertension). As a rule, there is blurred vision, flickering of spots before the eyes, and darkening of the eyes. Combined symptoms may also occur, for example, hearing and vision impairment or dizziness, blurred vision.
Migraine
A migraine attack may be accompanied by temporary blurred vision against the background of severe vasospasm. Often, pain in the head is accompanied by the appearance of an aura in the form of flickering scotomas (flickering or floating dark spots in front of the eyes).
Intraocular pressure
If intraocular pressure is normal from 9 to 22 mmHg, then an acute attack of glaucoma can raise it to 50-70 or higher. In this case, a sharp headache covering half the head and the eyeball accompany a one-sided process. If both eyes are affected, the whole head hurts. In addition, blurred vision, rainbow circles before the eyes, or dark spots (scotomas) may appear. Autonomic disorders (nausea, vomiting, heart pain) are often associated.
Medicines
Drug effects can also lead to transient myopia. This occurs when taking high doses of sulfonamides.
Why does vision disappear for several minutes?
Temporary (intermittent) blindness is a condition in which a person’s vision can suddenly disappear and also suddenly appear.
In this case, both eyes are not necessarily affected; one eye can also go blind. There is also the concept of “snow blindness,” when a person can temporarily go blind from bright light. This concept received its name after many cases of short-term vision loss were recorded in people while contemplating snow-covered expanses and bright sunlight. Vision loss can last from a few seconds to several minutes. Such visual impairment often worries older people who suffer from atherosclerosis and heart and vascular diseases. Intermittent blindness can be a harbinger of dangerous diseases such as heart attack or stroke.
Features of temporary blindness:
- a person stops seeing in both eyes or one eye at once;
- loss of vision may be accompanied by the appearance of “shadows” before the eyes;
- Most often, this condition occurs in older people who suffer from diseases of the cardiovascular system.
Even with short-term vision loss (for example, a few seconds), it is necessary to consult a doctor for an accurate diagnosis and treatment. He will conduct a vascular examination and prescribe medications that slow down blood clotting. It is always worth considering that a condition such as temporary blindness can indicate serious problems in the body. Therefore, it is very important to follow all the doctor’s recommendations to avoid relapses.
Causes of temporary blindness:
- increased intracranial pressure;
- blockage of the arteries of the spine, which are involved in the blood supply to the visual segment of the brain;
- spasm of the ocular arteries that supply the retina with blood.
All patients who have experienced short-term vision loss should follow some preventive measures that will help them avoid the occurrence of this condition again.
1. Take vitamins and medications as prescribed by your doctor. 2. Do special gymnastics for the eyes. 3. Regularly go for preventive examinations to an ophthalmologist. 4. Be sure to wear dark glasses so that bright light does not fall on the retina of your eyes. 5. Minimize alcohol consumption. Ideally, you need to eliminate it completely. 6. Lead a healthy lifestyle:
- Healthy food; - exercise; - try to avoid stressful situations; - adhere to positive thinking; - rest more.
Sudden deterioration of vision
Most often, a stroke, brain tumor, retinal detachment or eye injury are to blame for irreparable sudden loss of vision. Loss of vision can occur suddenly or within a few hours.
Reversible vision loss
If we are talking about acute reversible loss of vision in both eyes, then the culprit is an attack of oxygen starvation of the visual cortex (ischemic attack as part of a chronic cerebrovascular accident or ischemic stroke in the posterior cerebral artery basin) or an attack of severe migraine. In this case, there is not only a headache and blurred vision, but also a color perception disorder in the form of fading of objects.
- A rare form is postpartum blindness due to embolism of the branches of the posterior cerebral artery.
- After operations or injuries with loss of large volumes of blood and a drop in blood pressure, posterior ischemic optic neuropathy often develops. The consequence is an amblyopic attack.
- In case of poisoning with surrogate alcohol (methyl alcohol), chloroquine, quinine, and phenothiazine derivatives, bilateral vision loss (or at least central scotoma) occurs within the first 24 hours. Approximately 85% of patients recover; in the rest, blindness is complete or partial.
- There are also rare familial forms of temporary blindness lasting up to 20 seconds with a sudden change in lighting or body position.
Permanent vision loss
Sudden loss of vision in one eye is primarily suspicious for retinal dissection, central retinal vein thrombosis, or arterial occlusion.
- If the situation develops due to a head injury, exclude a fracture of the skull bones with damage to the walls of the optic nerve canal. This can only be corrected by emergency surgical decompression.
- An acute attack of glaucoma (increased intraocular pressure) is accompanied by redness of the eye, loss of vision, pain in the head, heart or abdomen, the density of the eyeball is comparable to the density of the table.
- The cause may also be ischemic optic neuropathy due to temporal arteritis and occlusion of the posterior ciliary artery. This is suggested by pain in the temple that appears and persists for several months, fatigue, joint pain, lack of appetite, and increased ESR in an elderly patient.
- An ischemic stroke can also cause blindness in one eye (see signs of stroke).
An ophthalmologist together with a neurologist should understand why vision suddenly decreases, since vascular pathologies most often come to the fore as the causes of sudden vision loss.
Other possible causes of temporary blindness
Temporary vision loss (total or partial) can also result from:
- migraine;
- sickle cell anemia (hereditary blood disease);
- acute angle-closure glaucoma (sudden increase in eye pressure);
- periarteritis nodosa (blood vessel disease);
- Optic neuritis (inflammation of the optic nerve);
- increased plasma viscosity (leukemia, multiple myeloma);
- papilloma;
- traumatic brain injury;
- a brain tumor.
Important! Vasospasm can also lead to temporary vision loss. This condition is the result of restricted blood flow due to sudden constriction of the eye's blood vessels.
Vasospasm can be caused by:
- exercise stress;
- sexual intercourse;
- long distance running.
Diagnostics
To get a complete picture of the state of the visual analyzer. An ophthalmologist or ophthalmologist today has a whole range of diagnostic capabilities. A number of studies are based on hardware methods. During the examination they usually use:
- Measuring visual acuity (using tables).
- Measuring the refractive capabilities of the eye (hardware method)
- Determination of intraocular pressure.
- Checking visual fields.
- Examination of the fundus (changes in the retina with a wide pupil) with examination of the optic nerve head.
- Biomicroscopy (examination of the eye through a microscope).
- Echobiometry (determining the length of the eye).
- Pachymetry (measuring the thickness and angle of curvature of the cornea).
- Computer keratotopography (determining the profile of the cornea).
- Ultrasound of ocular structures.
- Measuring the production of tear fluid.
Treatment of vision impairment
Most often, in case of vision problems, they resort to conservative correction or surgical treatment.
Conservative treatment
The conservative part of the program includes correction with glasses. Lenses, hardware techniques, gymnastics and eye massage (see eye gymnastics). For degenerative pathologies, vitamins are added.
- Spectacle correction allows you to reduce the risks of strabismus, retinal detachment due to myopia, farsightedness, and also correct complex types of visual impairment (astigmatism in combination with myopia or hyperopia). Glasses somewhat limit the field of vision and create difficulties when playing sports, but they do the job quite well, allowing you to supply your eyes with any type of necessary lenses.
- Aesthetes and those who make money thanks to their appearance resort to lenses. The main complaints about this type of correction are complex hygienic requirements. Risks of bacterial and protozoal complications, lack of full air penetration into the eye. In general, modern lenses offer both disposable and breathable options.
- Gymnastics and massage help improve blood supply to all structures of the eye, make the oculomotor and ciliary muscles work, and are suitable for correcting simple weak degrees of myopia or farsightedness.
- Hardware techniques – classes with an instructor with or without glasses on special installations that train the eye muscles.
Operational aids
- Cataracts today are successfully treated only by removing the clouded lens with or without its replacement.
- Tumor and some vascular processes can also be corrected exclusively by surgery.
- Laser welding of the retina allows you to solve the problem of tears or partial detachment.
- The PRK method is the earliest variation of corneal laser correction. The method is quite traumatic, requires long-term rehabilitation and is contraindicated for both eyes at the same time.
- Lasers are also used today to correct visual acuity (farsightedness of 4 diopters and myopia of 15, astigmatism within 3). The LASIK method (laser assisted keratomileusis) combines mechanical keratoplasty and laser beams. A corneal flap is peeled off with a keratome, the profile of which is adjusted with a laser. As a result, the cornea decreases in thickness. The flap is welded into place using a laser. Super-LASIK is a variation of the operation with very gentle grinding of the corneal flap, which is based on data on its curvature and thickness. Epi-LASIK allows you to avoid staining the corneal epithelial cells with alcohol and correct marginal distortions (aberrations) of vision. FEMTO-LASIK involves the formation of a corneal flap and its treatment with a laser.
- Laser correction is painless, leaves no stitches, and requires little time, including recovery. But some of the long-term results leave much to be desired (dry eye syndrome, inflammatory changes in the cornea may occur, the corneal epithelium may become excessively rough, and sometimes corneal ingrowths may develop).
- Surgical laser intervention is not performed on pregnant women, nursing mothers, or children under 18. This technique cannot be used on a single eye, with glaucoma, insufficient corneal thickness, autoimmune pathologies, with cataracts, immunodeficiency, progressive forms of myopia, operated retinal detachment, or with herpes.
Thus, the problems of vision loss are very diverse. They often progress, leading to complete loss of vision. Therefore, it is the early detection of pathologies of the visual analyzer, their prevention and correction that can protect a person from disability.
Author:
Postnova Maria Borisovna general practitioner
Treatment
Treatment of temporary vision loss in one eye begins with identifying the underlying disease.
For example, if blood clots have caused blindness, doctors concerned about the possibility of a stroke may recommend:
- blood thinners;
- medications to lower blood pressure;
- surgical intervention.
Your doctor may also recommend lifestyle changes, including:
- reducing consumption of fatty and processed foods;
- daily exercise;
- stress reduction.