Laser technologies in ophthalmology are a modern, innovative method for correcting and treating various visual impairments. The patient can get rid of glasses and contact lenses in just 1 day. The percentage of operations with good results is impressive; according to the LaSIK of Life Collaboration Project, approximately 96% of patients who underwent laser vision restoration are satisfied with the results of the procedure. However, in ophthalmological practice there are sometimes cases where vision after surgery not only is not restored, but even worsens.
Share
Tweet
Share
Cool
Send
ENHANCEMENT – additional correction after laser correction has already been carried out – the essence of the matter
According to medical indications, we can talk about additional vision correction when we have an increase in the axial length of the eye, regression after correction, or residual unplanned refraction (optics).
Most often, this is discussed no earlier than 3 months after the correction - this increases its accuracy.
Important:
- Each correction method has its own capabilities - this affects the choice.
- Each surgeon has certain skills - this influences the choice.
- Each clinic has a certain type of equipment - this affects the choice.
- Each patient has individual anatomical background and visual needs - this affects the choice, etc.
In short, it is similar to “poker” - there are many combinations, the patient and the surgeon do not have complete information (additional correction is often done years later, in another clinic), “trading” is possible in the selection process. This is not chess, in which both players see the position of all the pieces on the board.
Postoperative visual impairment: consequences
In some cases, it is noted that after correction, vision decreases. This can happen even long after surgery. This decline in vision is called regression of the operating effect. Most often this occurs with severe myopia or farsightedness. Patients with large pupils sometimes see distorted images in the dark. In addition, some report poor vision in dim lighting. This phenomenon explains the decrease in contrast sensitivity. There is a possibility of corneal opacification, retinal detachment, bulging of thin areas of the cornea, flap slippage and corneal failure. The following possible symptoms negatively affect visual function, causing severe discomfort:
In some cases, a regression of the surgical effect occurs, which is accompanied by pain and burning in the organs of vision.
- pain;
- adhesion of the eyelid and mucous membrane;
- sensation of a foreign object;
- burning sensation;
- fog in the eyes.
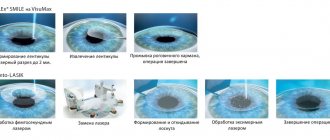
Additional correction methods after RELEX SMILE or SMILE
The method is the most modern, the most accurate and the most gentle when performed correctly.
There are the largest number of questions and myths about it. What is its fundamental difference is written in these articles: “Direct comparison of laser myopia correction methods” and “Why we do SMILE.” For SMILE, you can use the largest range of possible additional correction methods:
1. SMILE after SMILE (Sub-cap lenticule extraction)
If we are talking about myopia and astigmatism, then additional correction can be performed using the same SMILE method. Schematically it looks like this:
This method can also be used to correct myopia of more than 10 diopters (for example, -15.0 diopters) - in the form of a two-step procedure.
A method for highly experienced ReLEX SMILE surgeons who have experience working with thin lenticules. Is it possible to do this through the same 2 mm? Easy - for the second stage I use the same 2mm input! But for this, the thickness of the cornea must also be sufficient, as for additional correction in general.
2. Formation of the edge cut (side cut)
to form a valve cap (flap) - a kind of transition to femtoLASIK technology with a cap equal to the diameter of the “cap” with SMILE. It looks like this:
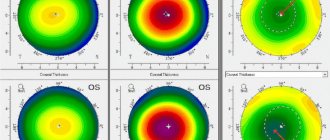
Can be used if you calculate that there is at least 300 microns left under the lid. The diameter of the lid should be sufficient, but the thickness of the lid in this case does not matter. Tomogram of the cornea after the formation of the marginal cut
3. CIRCLE
– a program that also allows you to form a flap cap and switch to femtoLASIK technology with a cap of a larger diameter than the diameter of the cap. This is a standard module recommended by the manufacturer for additional correction. The module is very useful, although Zeiss does not give access to it to everyone right away.
Schematically it looks like this:
The lid is lifted and excimer laser polishing is done. What is its advantage? This is necessary to obtain a large diameter optical zone = high-quality vision. Therefore, in case of additional correction of “alien” eyes after femtoLASIK (if the diameter allows), I often use CIRCL to create a new side cut with a smooth edge.
This is what the cornea looks like on a tomogram after CIRCLE
Schematic difference between SMILE and CIRCLE
Performing this procedure also requires the application of a vacuum cone and a laser operating time of about 15 seconds
Why is the safety of switching from SMILE to femtoLASIK, if additional correction is necessary, higher than lifting an already formed cap after femtoLASIK and repeat additional correction?
- because CIRCL allows you to expand the area for correction, and you cannot enlarge an already made cover;
- When we re-lift the cap (after femtoLASIK or LASIK), the edges become less smooth and the risk of epithelial ingrowth from the surface under the cap increases, and CIRCLE allows us to create a clear adaptive primary edge.
Hence, the quality of vision after such additional correction after SMILE is higher than the same additional correction after femtoLASIK. This is what the surface of the eye looks like under a microscope 10 minutes after CIRCLE
4. FemtoLASIK (Thin Flap LASIK) on top of SMILE.
If ReLEX SMILE is performed at a depth of at least 135 microns, then a “cap” can be used to form a thin cap on top.
And then everything is as usual - open the lid, evaporate as much as necessary and as much as the thickness of the cornea from below allows, close the lid. Schematically it looks like this:
Tomogram of the cornea after the formation of a thin cap in the “cap” SMILE The eye looks excellent and vision is 1.0
5. FemtoLASIK (Thick Flap LASIK) from below SMILE.
If ReLEX SMILE is performed at a depth of 100 microns, then the lower part of the cornea can be used to form a thick cap on top that includes the SMILE zone. And then everything is as usual - open the lid, evaporate as much as necessary and as much as the thickness of the cornea from below allows, close the lid. Schematically it looks like this:
6. PRK method (or transFRK)
– we can use it with a final corneal thickness of more than 350 microns.
Of course, it has all the disadvantages of PRK:
- soreness for several days
- Hayes risk,
- slow recovery of vision up to several weeks,
- starting (initial) hyperopic overcorrection associated with epithelial remodeling.
On the left – transPRK, on the right – classic PRK
7. Intrastromal keratoplasty (intrastromal keratotomy)
— using a femtosecond laser, you can make incisions in the stroma, thereby changing the curvature of the cornea. This is a modern modification of an ancient keratotomy.
Among the advantages - there is no loss of corneal tissue, there is no damage to the anterior surface of the cornea.
Schematically it looks like this:
8.
Implantation of a phakic IOL.
You can read how this is done here: “Calculation of intraocular phakic lenses.”
If there is enough space in the posterior chamber of the eye - more than 3 mm, then a phakic correction lens can be implanted, which does not need to be removed and is not visible at all. Then we don’t touch the cornea and leave our lens. We just put something useful in the eye. Previously performed correction in the cornea does not in any way interfere with either the calculations of the phakic IOL or its implantation.
Phakic intraocular lens implantation scheme
Is it possible to change eye color using laser correction?
Intervention using modern equipment is used not only to combat ophthalmological diseases. It helps change the hue of the iris. The operation lasts no more than a minute. Excess pigment is removed using a laser. The procedure helps correct color only in dark-eyed patients.
A month after the intervention, brown eyes will turn blue. However, do not forget that the effect is irreversible. Therefore, before deciding to have surgery, think carefully about everything. As a result of the correction, complications such as photophobia and diplopia may appear.
The operation does not require additional preparation and does not cause pain during the process. The device used to perform the operation resembles binoculars in appearance. The patient watches an animated video while the laser emits pulses. Doctors use low-power rays, so the melanin pigment disappears only from the surface. The shell itself remains unharmed.
Immediately after correction, the iris darkens as the process of cell death occurs. However, after a couple of weeks it will begin to lighten. The end result is visible after thirty days.
Additional correction methods after LASIK/femtoLASIK – technologies with a “lid”
1. Lifting the cover.
An important point is that the cornea already has a superficial flap of a certain thickness - the lid. This operation differs from correction using the LASIK method only in that the surgeon lifts a flap of the cornea that was cut off earlier, rather than cutting it off again. It is supported only by the epithelium in the case of LASIK, and “epithelium + cap edge” after femtoLASIK.
The lid itself never grows - even after several decades it can be lifted, but the edges after lifting never remain as smooth as the original ones.
And making a primary correction is always easier than any additional correction.
The procedure for forming a valve cap during LASIK
After LASIK, you can often lift the old cap with one movement of a spatula; after femtoLASIK, it takes more effort. This is both good and bad - what is easily lifted is easily displaced (for example, during injury) and vice versa.
Eye after lifting the lid
Before additional correction, it is necessary to determine the thickness of the previously formed lid and the thickness of the expected remainder of the cornea, so as not to get keratectasia, I wrote about it here: “Keratoectasia (keratoconus, “convex cornea”): what is it and what to do about it.”
After femtoLASIK, the edge of the cap is firmly held, so in order not to injure it, you can resort to forming a new marginal entrance (side cut) using CIRCLE.
Lifting risks involve:
- with ingrowth of the epithelium (the outer rapidly multiplying layer) under the lid - after all, the old edges will not fit as tightly as during the initial cut,
- the cover may be damaged,
- folds of the lid may form, interfering with vision.
- sometimes you have to deal with a initially wrinkled lid after the first correction, which was not smoothed out enough. Then it’s a whole story with removing the epithelium, soaking it, sewing it along the edges as with keratoplasty.
In short, no lid - no problems with the lid: for this you need to choose a premium SMILE or a budget transPRK.
2. SMILE in the “lid”
This technology can only be done if the lid is thick - old corrections with the first models of keratomas cut lids up to 200 microns thick. On the plus side, since the lid is cut off, it does not add strength, changing its thickness does not in any way affect the overall strength of the cornea, and SMILE is only 25 seconds, the next day there are no restrictions, we do not lift anything, the epithelium does not grow in, biomechanics does not suffer, and so on. etc. I've only used this technique a couple of times.
This is the operation diagram:
3.
SMILE under the “lid”
If the lid is thin, the cornea underneath is thick, this can be done. In this case, the biomechanics decrease as usual, but again only 25 seconds, the next day there are no restrictions, we don’t lift anything, the epithelium does not grow in.
Schematically it looks like this:
 And yes, those attentive noticed that the pictures were repeated as in the section about SMILE!
And yes, those attentive noticed that the pictures were repeated as in the section about SMILE!
4. PRK/transFRK
We work according to the usual program - we remove the epithelium, evaporate, process, put on a contact lens, wait for healing and remodeling of the epithelium.
There are also limitations for this method - when we calculate the diopters that need to be adjusted, we must calculate the thickness of the tissues for evaporation. There is no way to completely burn through the lid - so here the possibilities are limited by the thickness of the lid!
5. Phakic IOL
– we shouldn’t forget about it, especially in cases where you don’t want to touch the cornea and make it thinner, but need to make a correction.
Causes of decreased vision after surgery
Laser vision correction involves opening the cornea, which causes redness and minor hemorrhages in the postoperative period. Therefore, the following negative conditions may occur:
- corneal clouding;
- retinal detachment;
- thinning of a certain area of the cornea;
- lack of corneal functionality.
A complicated condition occurs in extreme cases and does not occur in all patients. A predisposition to the appearance of these conditions is formed when diseases of the eyeballs are already formed. The risk of decreased visual acuity after surgery occurs in the following categories of patients:
- those suffering from glaucoma, cataracts;
- having high myopia or hypermetropia;
- suffering from systemic diseases that the patient did not tell the doctor about.
In order not to cause a decrease in visual acuity, it is important for the patient, before the operation, to tell the doctor about all the disorders in his body that he knows about.
After laser vision correction, a temporary decrease in the functionality of the eyeballs is possible. The patient sees distant objects well, but poorly near ones. Vision may drop sharply and become blurred. The patient may experience a decrease in visual acuity at dusk.
Most often, such conditions are temporary and are associated with a violation of the integrity of the eyeballs. After all the tissues have healed, they go away.
Immediately after the operation, small hemorrhages form in the cornea, an inflammatory process. The first condition goes away on its own when the blood clots dissolve. To prevent complications of the inflammatory process, the doctor prescribes anti-inflammatory eye drops.
Methods of additional correction after photorefractive keratectomy - PRK/TRANSFRK
The method is ancient, I wrote about it here, too.
Therefore, there are plenty of patients after such a correction. There are many who have a characteristic haze - a “fogginess” in the cornea that reduces visual acuity and cannot be corrected with glasses.
This is what the installation for excimer laser correction LASIK and transPRK looks like.
Several options can be offered - but all this takes into account the residual thickness of the cornea:
1. ReLEX SMILE
I suggest it if the thickness of the cornea is sufficient and the transparency of the cornea is sufficient (light haze is not a hindrance). Recovery is extremely fast - just like after standard ReLEX SMILE, even less lacrimation.
2. Repeat PRK
– everything according to the traditional scenario: removal of the epithelium, working with an excimer laser on the surface of the stroma, treating the surface with a drug, a contact lens for several days. It is better to use it as a method to combat the previous haze, and with small corrections of up to 1-2 diopters.
3. FemtoLASIK or LASIK
– you can cut out the lid, lift and evaporate the required profile. LASIK is also much more dangerous in this case - on a flat cornea the cap may turn out to be defective.
4. Phakic IOL
– again, if there is space in the posterior chamber of the eye, but there is not enough cornea.
Contraindications
Laser vision correction is not a therapeutic procedure. It helps eliminate eye problems, but does not cure the disease. Unfortunately, this effective technique has a number of contraindications:
- Unstable visual process. As a person grows, the eyes also change for better or worse. Therefore, the operation is not performed on patients under eighteen years of age. To carry out correction using a laser, visual acuity must be stable for two years;
- Diseases of internal organs and systems. For example, diabetes or arthritis;
- Pathological processes in the visual apparatus (development of glaucoma or the presence of senile cataracts);
- Pregnancy and lactation period. The reason lies in the fact that at this time women experience hormonal instability. Also, during the recovery process, antibacterial drugs are often prescribed, which can have a negative impact on the health of the unborn baby or newborn baby;
- A sharp drop in visual acuity;
- Inflammatory processes affecting the eyes. Before performing the operation, it is necessary to undergo a course of therapy and get rid of them;
- The initial stage of dystrophic changes affecting the retina. In this case, it is first necessary to carry out laser coagulation, which will strengthen the weakened element;
- Destructive processes in the cornea (keratoconus, dry eye syndrome);
- Any ailment accompanied by a decrease in the body’s protective barrier. To strengthen the immune system, you need to take a vitamin and mineral course.
| Also, the procedure is not performed in the presence of malignant neoplasms, problems with the endocrine system and sexually transmitted diseases. |
Radial keratotomy - incision technique (manual, non-laser method)
From previous articles (“History of vision correction operations”, “The story of one eye and 20 operations (not to be read by the impressionable)”), we remember that this is the oldest method of the 80s of the last century. Accordingly, most people who have undergone radial keratotomy are well over 40-45 years old. In this case, the cornea looks like this - like a pie cut (not all the way through) into pieces, the direction of which coincides with the imaginary radii of the conditional circle of the cornea with a central zone with a diameter of at least 3 mm.
Most often we are faced with the appearance of farsightedness - the so-called hypermetropic shift (+) or astigmatism (±).
It is less common to have to do additional correction of myopia (-). If the lens is transparent and in good condition, choose:
1. FemtoLASIK or LASIK
This is an operation of choice, since the thickness of the lid is precisely specified and does not allow the cornea to move apart at the seams. And if it spreads in some place, then I collect such “petals”. There are surgeons who think that this is risky - the flap will not rise on the adhesions or will crumble. And they choose the much riskier and less desirable LASIK. LASIK - the formation of a lid using a microkeratome - a mechanism with blades - so it may not fit properly, it may turn out to be a “micro-flip” or “pizza”, but the blade easily cuts the scars. In addition, with femtolasik, the increase in intraocular pressure is moderate, much lower than with vacuum LASIK technology.
This way we can correct myopia, hyperopia and astigmatism after radial keratotomy.
2. Tightening seams
Over time, the cornea sags under the influence of intraocular pressure and its reduced rigidity, the lower scars stretch and fill with epithelium. Like stretch marks on the skin. It looks like this and leads to hypermetropia and astigmatism:
In this case, it is possible to “clean out” the epithelium from the keratotomy scars, tighten them with thin threads and thus obtain a “steeper” and more regular cornea. It looks like this:
3.
Phakic IOL
– We put something useful in the eye as described above.
4. Photorefractive keratectomy – PRK or transPRK.
It is preferable to perform it according to the topographic profile and you definitely need a cytostatic agent on the surface. Without mitomycin, in such eyes the development of haze (subepithelial opacities) is practically a one-time process (and this does not depend on the type of laser). And, of course, all the disadvantages of PRK will be present - you can’t do without them.
5. Replacing your own lens with an intraocular lens with new optical characteristics
, for example, with the correction of astigmatism, if opacities appear in the lens, cataracts or severe sclerosis begin. Therefore, the condition of your own lens will play a big role in choosing a technique - they will not feel sorry for it and will offer to solve the issue of correction by replacing the lens with an artificial transparent lens with new optical properties.
What is laser eye surgery?
Laser vision correction is a high-precision method of treating eye diseases. The procedure helps restore the brightness and contrast of the visible image, eliminating the need to wear glasses and contact lenses. Eye surgeries using lasers began to be performed 30 years ago under the leadership of Svyatoslav Fedorov. Laser correction refers to minimally invasive methods of treating visual acuity.
With any type of visual impairment, the image is incorrectly focused on the retina. Therefore, the main principle of laser surgery is to change the shape of the cornea so that the refracted beam of light precisely hits the retina. To do this, surgeons use a laser to vaporize a thin layer of epithelial cells on the cornea.
To perform the operation, the patient must undergo an ophthalmological examination so that doctors receive complete information about the condition of his visual organs. Thanks to laser correction, myopia, astigmatism and hypermetropia can be treated in patients aged 21 to 55 years.
How is it done?
Before the operation begins, the ophthalmologist directs the patient to a number of examinations:
- donating blood for general analysis;
- exclusion of hepatitis B and C, HIV infection;
- ophthalmoscopy;
- slit lamp examination;
- MRI, angiography, radiography using contrast and other examinations depending on the type and severity of the disease, the condition of the tissues of the eyeballs.
IMPORTANT. In preparation for the procedure, the patient should stop wearing contact lenses: soft 1 week before surgery, hard ones 14 days before surgery. You should avoid using alcohol 48 hours before laser correction. On the eve of the operation, it is prohibited to use cosmetics.
The procedure is carried out using a special device that directs a laser beam onto the cornea. Heat waves evaporate thin layers of cells. Despite the use of high-tech techniques, the microsurgical operation takes no more than 15-30 minutes.
Expert opinion
Nosova Yulia Vladimirovna
Ophthalmologist of the highest category. Candidate of Medical Sciences.
Treatment is carried out on an outpatient basis. After receiving the examination results and making an accurate diagnosis, the patient lies down on a couch or a special chair. The doctor instills anesthetic into the eyes for pain relief and fixes the patient’s head. After this, the eyelids of the affected eye must be secured in the open position.
Using a keratome, the surgeon uses a microtome to cut a small section of the cornea and retract it to the side, leaving part of the flap attached to the anterior chamber of the eye. This is necessary to gain access to the deeper layers of the cornea.
The transparent fabric is then exposed to laser light, giving it a new shape. After completing the manipulations, the doctor returns the allocated area of the cornea to its original position and smoothes it over the surface of the eyeball.
To reduce the risk of infection, antibiotic drops are instilled into the operated area. Doctors remove the clamps from the eyelids and head. The patient can go home.
When the eyeball moves during surgery, there is no threat to vision. A scanner on the hardware unit registers the slightest deviations in gaze and corrects the direction of the laser beam. If there is a sudden and strong deviation of the eye, the device automatically stops working.
Conclusion
Additional correction or enhancement is a procedure to change the optical power of the eye after previously performed vision correction.
Additional correction is a good way to improve vision. Each method of both correction and additional correction is selected based on taking into account a large number of factors; undoubtedly, the surgeon’s factor is important, the patient’s individual parameters are definitely important, the determining factor is the choice of the clinic. Each method is good, but in order to make the right choice, the surgeon must master the entire palette of operations. Otherwise, you will be offered at a discount only the method that is available (in most cases this will be LASIK).
The ReLEX SMILE method is not only fast, but also provides the least need for additional correction and the greatest scope for creativity - much more than its predecessors. It can also be used for additional correction after using other methods!
What to do if symptoms occur?
Severe prolonged eye pain, permanent fluctuations in vision, flashes of light are reasons to seek advice from an ophthalmologist. The same applies to inflammation of the cornea, a feeling of dryness in the eyes and slight clouding. In most cases, these symptoms are eliminated with complex therapy. However, in some cases it is necessary to re-correct. Such manifestations include sudden loss of vision, severe clouding of the cornea, and displacement of the pupils. In this situation, immediate contact with your doctor is required.