Due to the immature immune system, the child’s body is susceptible to various ophthalmological diseases. One of the most common eye pathologies in childhood is blepharitis - inflammation of the ciliary edges of the eyelids. This pathological process is chronic and is most often caused by increased activity of Staphylococcus aureus. Blepharitis in children is accompanied by a number of unpleasant symptoms that significantly worsen the child’s vision and general health.
Causes
The main reason for the development of blepharitis is the activation of pathogenic microorganisms that live on the eyelids, as a result of increased tissue thinness and the lack of fat deposits in this area of the body. Blepharitis can occur at any age, but is most often observed in children due to low immune resistance to infectious agents. In most cases, the inflammatory process is provoked by demodex mites, Staphylococcus aureus or the herpes virus.
The following causes of blepharitis in children are identified:
- inflammatory processes in the eyes;
- infectious diseases;
- lack of personal hygiene;
- hypothermia;
- decreased immunity;
- allergic reactions;
- exhaustion of the body;
- gastrointestinal pathologies;
- seborrheic dermatitis;
- disturbance of material metabolism;
- lack of proper treatment for farsightedness;
- foreign body entering the eye.
The causes of inflammation of the edges of a child's eyelids can be very diverse. It is not always possible to determine the exact nature of the disease.
Most often, childhood blepharitis is a consequence of poor personal hygiene.
Characteristic symptoms
Blepharitis in children has various symptoms, which directly depend on the form and extent of the lesion. Similar symptoms are also inherent in other ophthalmological diseases; it is important not to confuse them. If negative symptoms occur in a child, you should consult a doctor. Symptoms and treatment depend on the form and extent of the lesion.
Blepharitis is manifested by the following symptoms:
- puffiness, swelling and redness of the eyelids;
- itching and burning;
- increased lacrimation;
- photophobia;
- the formation of scales on the eyelashes that are difficult to remove;
- purulent blisters;
- painful sensations.
In the absence of proper drug treatment, a number of complications arise:
- ulcers on the surface of the eyelid;
- thickening of the eyelids;
- damage to the eyelash bulbs, which leads to their loss;
- narrowness of the eye slit.
The symptoms are pronounced, so they are noticeable.
Types of childhood blepharitis
Taking into account the nature of origin, experts identify 5 main types of blepharitis in children:
- Scaly (simple). The edges of the eyelids thicken, turn red and become covered with scaly crusts that settle tightly at the base of the eyelashes. It often occurs simultaneously with seborrheic dermatitis of the skin. Scaly blepharitis requires long-term treatment and often becomes chronic.
- Ulcerative. Purulent inflammation of the ciliary hair follicles occurs, and strong lesions covered with crusts are observed on the edges of the eyelids. When removing purulent ulcers, scars remain, and most of the eyelashes are removed along with the crusts.
- Demodectic. It occurs as a result of the active reproduction of the demodex mite, which lives on the eyelids and can only be detected with a microscope. Demodectic blepharitis is manifested by severe itching and the release of a sticky secretion.
- Meibomian. The meibomian glands of the eyelid intensively produce secretions that are poorly excreted. This provokes the appearance of copious discharge from the eyes and the formation of crusts.
- Allergic. It occurs against the background of increased sensitivity to any allergen (dust, chemicals, etc.). Most often it is a seasonal disease, often accompanied by allergic conjunctivitis.
Somewhat less common in children is acne, mixed and rosacea blepharitis.
Correct determination of the type of inflammatory process allows you to select the most effective treatment.
What Doctor Komarovsky says
The main thing is to make a diagnosis quickly and correctly. After this, we begin to treat, making sure to follow generally accepted rules of hygiene and take photographs at each stage. A simple table will help you understand what you are faced with and what to do before a specialist arrives.
| Disease | Cause of occurrence. | Manifestations | How to fight |
| Blepharitis scaly | The root cause is seborrheic dermatitis. | The edges of the eyelid are red, covered with fatty scales. The meibomian glands are slightly swollen. | Using special shampoos to wash your hair. Mandatory removal of scales with a damp swab twice a day. For more severe forms, bactericidal ointments are used. |
| Ulcerative blepharitis | People can get sick throughout their lives. Accompanied by the frequent appearance of acne, barley and seborrhea. | Severe swelling, formation of dense crusts, after removal of which bleeding ulcers appear. In the chronic form, without proper treatment, deformation of the eyelids occurs. | Using medicated shampoos and washing the eyes daily with warm water. After cleansing, lubricate the damaged area with bactericidal ointment. |
The main advice is to quickly respond to any changes in the child’s condition. Do not self-medicate and do not trust the experience of neighbors and friends. Each child is individual, and what has a beneficial effect on one may have a detrimental effect on the well-being of another. Only a doctor is able to choose the method of influence and achieve a good result.
Symptoms
The first symptoms of inflammation of the ciliary margin of the eyelids in children are similar to the manifestations of many other ophthalmological diseases, which makes timely diagnosis of the pathology difficult. At the initial stage of blepharitis, redness and swelling of the eyelids are observed, the baby complains of severe itching and discomfort in the eyes.
Common manifestations of all types of disease include the following symptoms:
- lacrimation;
- feeling of sand in the eyes;
- increased sensitivity to light;
- separation of fluid from the eye;
- hyperemia of the iris;
- thickening of the eyelids;
- narrowing of the palpebral fissure.
Symptoms of the inflammatory process may differ depending on the form of blepharitis:
- Scaly. The edges of the eyelids become significantly thicker and redden, and small crusts similar to dandruff form near the eyelashes.
- Ulcerative. Purulent crusts form on the ciliary edge, in place of which bleeding ulcers and scars remain. Accompanied by increased loss of eyelashes.
- Demodectic. The edges of the eyelids thicken, pronounced hyperemia and swelling are observed, and translucent crusts form. The skin of the eyelids acquires a darker shade, the child complains of unbearable itching.
- Meibomian. Symptoms are similar to other forms. A distinctive feature is the formation of tiny blisters on the upper part of the eyelid, in place of which scars remain.
- Allergic. In addition to the general symptoms, other manifestations of allergies are observed: coughing, sneezing, runny nose.
With any form of blepharitis, the child becomes capricious and irritable, constantly rubs his eyes, and blinks frequently. In the morning, sticking and swelling of the eyes and loss of eyelashes are often observed.
Prevention
The main preventive measure to eliminate blepharitis is keeping the house clean and teaching the child the rules of personal hygiene .
Children often carry pathogens of infectious ophthalmological diseases with dirty hands, so it is necessary to explain to them the importance of washing their hands every time they return from the street.
Parents should also let their children understand that using other people's towels, handkerchiefs, clothes and hats can also lead to eye diseases. This also applies to drops that another person uses: sometimes bacteria and infections that cause illness remain on the container with the medicine.
Diagnostics
When the first symptoms of blepharitis appear, you should contact a pediatric ophthalmologist. First of all, the doctor will conduct a detailed survey and examination of the child, after which he will prescribe the following tests:
- biomicroscopy;
- visometry;
- ophthalmoscopy;
- stool analysis.
Read in a separate article: Strabismus in newborns: causes and treatment
In order to determine the bacterial pathogen, the eyelash crusts are scraped and the secretion secreted from the child’s eye is collected.
Laboratory research allows you to diagnose the pathogen. If necessary, allergy tests are done.
Common symptoms across species
Different types of blepharitis have some common signs and symptoms by which it can be recognized :
- itching sensation in the periocular area;
- redness, swelling of the eyelids;
- the appearance of secretions that lead to gluing of the eyelids and eyelashes;
- the formation of an excessive amount of tear fluid, which, together with purulent discharge, forms a film on the surface of the eyeball that helps reduce visual acuity.
If a child wears contact lenses, it is difficult to use such optics for blepharitis due to irritation and pain.
At the age of two to three years and in newborns with blepharitis, discharge from the eyes will be more abundant, and other symptoms will also be more pronounced.
It is important for parents not to miss such symptoms and to visit a pediatrician and ophthalmologist if at least two of the listed signs are observed.
Drug therapy for blepharitis in children
Treatment of blepharitis in a child should be selected by a doctor, taking into account the type of pathological process.
First of all, treatment is aimed at eliminating the pathogen, and only then at relieving symptoms. Depending on the type of blepharitis, therapy may look like this. Scaly:
- cleansing the eyelids with synthomycin emulsion 1%;
- treating the eyelids with an antiseptic (brilliant green, essential alcohol);
- glucocorticosteroids: Hydrocortisone-Pos, Dexamethasone;
- application of antibacterial ointments: Tetracycline, Fucidin;
- eye drops: Tsipromed, Fucidin;
- instillation of artificial tears.
Ulcerative:
- complex ointments: Maxitrol, Dex-Gentamicin;
- washing the eyelids with Furacilin solution;
- systemic therapy with Metronidazole;
- eye gel: Solcoseryl, Korneregel.
Demodectic:
- washing the eyelids with saline solution;
- hormonal ointment: Hydrocortisone-Pos 2.5%;
- complex ointments: Dexa-Gentamicin, Maxitrol;
- eye drops: Dexapos;
- zinc-ichthyl ointment.
Meibomian:
- antimicrobial drops: Miramistin, Levomycetin;
- antibacterial ointments: Hydrocortisone, Tetracycline;
- instillation of Artificial tears;
- treatment of eyelids with antiseptics.
Allergic:
- antihistamine drops: Lodoxamide, Alomide;
- corticosteroids: Hydrocortisone, Maxitrol;
- antiallergic drugs: Suprastin, Cetrin.
For any form of blepharitis in a child, it is necessary to regularly clean the eyelids with a special solution or plain warm water, make warm compresses (herbal ones are best) and treat the eyelash edges with antiseptic agents. In addition to local therapy, various immunostimulating, vitamin complexes, and, if necessary, antibiotics, antiviral or other medications are prescribed. The selection of any medications should be carried out by a specialist.
Additionally, for blepharitis in children, physiotherapy, alternative medicine, and eyelid massage may be recommended. In the most severe cases, surgical intervention is performed.
Treatment of the disease
After the doctor examines the child, conducts an examination, talks with the parents, identifies possible causes of the disease, diagnoses symptoms, determines the type of blepharitis in the child, he will give recommendations on how to treat it.
- When allergic blepharitis is diagnosed in children, it is recommended to avoid contact with the allergen and wash the eyelids with warm, filtered water and soap.
- Special eye cream.
- Shampoo if blepharitis is seborrheic and has touched the scalp.
- Treatment of the edges of the cilia with an alcohol solution may be prescribed for demodectic blepharitis.
- Strengthening the immune system with vitamin therapy.
- Adjustment of diet, hypoallergenic diet.
- Massage of the century.
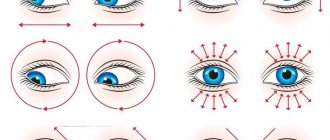
- Physiotherapeutic methods such as electrophoresis with medicinal solutions (antibiotics, vitamins C and B are most often prescribed), UHF therapy, UV irradiation, magnetic therapy, darsonvalization.
- External treatment of the eyelids with a 70% solution of ethyl alcohol, 1% brilliant green, tincture of medicinal calendula, decoction of chamomile.
- External treatment of eyelids affected by blepharitis with antibacterial ointments: erythromycin, tetracycline, Oriprim-P, Colbiocin, Ophthalmotrim.
- Ointments in the form of combined medications that combine both an antibiotic and glucocorticosteroids: Maxitrol, Dex-gentamicin, Garazon.
- When treating ulcerative blepharitis in children, it is recommended to carefully remove purulent crusts from the eyelids. They can be easily removed if you soften them first with lanolin or sterile petroleum jelly.
- Antimicrobial eye drops instilled into the conjunctival sac: solutions of miramistin, picloxidine, sodium sulfacyl, chloramphenicol.
Prescribed by a doctor, timely treatment of blepharitis in children leads to complete recovery without complications. If you miss the disease at the initial stage and ignore medication, this can lead to the most undesirable consequences, including deterioration of vision.
New articles
we are in social networks
up
source: www.vse-pro-detey.ru
If a child has red, irritated eyelids, a burning sensation near the eyes, peeling skin, and eyelashes sticking in the morning, it is most likely blepharitis.
What is blepharitis?
Blepharitis is an inflammation of the eyelids that can be chronic. Its symptoms - redness, scaly skin on the eyelids, burning - can resemble an allergy. Therefore, if something similar appears, you should contact your pediatrician, who, in case of inflammation of the eyelids, will refer you to an ophthalmologist.
If blepharitis is left untreated, it can cause conjunctivitis or styes, or more severe cases may occur.
How to treat blepharitis?
Blepharitis can be treated at home if the inflammation has just begun, however, you still need to see a doctor.
Before going to bed, be sure to wash the infected areas. To remove the crust, you need to wet a soft cloth with warm water and place it on the child’s closed eyes for about 5 minutes. Then, carefully, so as not to damage the skin, wipe the eyelids.
If your eyelashes stick together, you can dilute baby shampoo (2 drops of shampoo in 1/3 cup of water) and soak cotton swabs in this solution. Then gently clean the upper and lower lash line with them.
| Komarovsky Forum | arrhythmia in a child – Doctor Komarovsky |
| arrhythmia The child has. Hello, dear Evgeniy Olegovich! I have a question. child is 6 years old. We recently took our blood pressure and it… https://www.komarovskiy.net/forum/viewtopic.php?p=1223831&sid=2a164ce45d318b83c58ca237ea08125e |
Your doctor may recommend a special antibiotic ointment. After washing the eyes, it will need to be applied to the edges of the baby’s eyelids with clean fingers in order to prevent the infection from spreading to other parts of the skin around the eyes.
In addition to the ointment, drops may also be prescribed.
It is very important to do such procedures regularly for several days, even after the visible manifestations of blepharitis have disappeared, in order to prevent its reappearance.
What Causes Blepharitis?
Very often, the culprit for the appearance of this scourge is seborrheic dermatitis, eczema , bacterial infection (for example, staphylococcus), in addition, anemia, vitamin deficiency, diabetes, helminthic infestations, and problems with the gastrointestinal tract can contribute to its appearance.
Prevention of blepharitis
Parents should encourage and encourage frequent hand washing. In addition, you need to teach your child not to rub his eyes under any circumstances. Friction can spread the infection or worsen existing symptoms.
Please enable JavaScript to view the comments powered by Disqus.
source: health.kr.ua
Treatment with folk remedies
If blepharitis was detected at the initial stage of development, then it can be dealt with using alternative medicine. Depending on the type of inflammation in the child, it is recommended to use the following folk remedies:
- Scaly. Take equal quantities of dried leaves of chamomile, calendula and sage, mix, pour a glass of boiling water and let it brew for 30 minutes. After this, strain the infusion and rinse your eyes with it 2 times a day.
- Ulcerative. Combine 100 ml of strong green and black tea with 1 tablespoon of dry grape wine and rinse your eyes with the resulting product.
- Demodectic. Grind fresh peeled basil leaves into a fine paste, which you then apply on your eyelids for 10 minutes. Wash with warm water without soap.
- Meibomian. Boil 1 medium onion in 0.5 liters of water, add 1 tablespoon of honey to the water, stir. Use the eye wash solution.
- Allergic. Wrap 1 tablespoon of fresh cottage cheese in gauze and make a lotion on your eyelids.
Folk remedies for blepharitis in children help to effectively cope with the problem and improve the child’s condition, but only when used correctly. You should not self-medicate.
Treatment methods
So how to treat blepharitis? In most cases, conservative treatment is used.
If foci of inflammation do not arise as a result of dental, gastroenterological or dermatological pathologies, in which pathogens enter the eye area from other organs, drugs are prescribed depending on the severity and type of disease :
- The ulcerative form is treated with antibiotics and corticosteroids; various combinations of drugs in the form of ointments are possible (Dexamethasone and Neomycin). In case of complicated blepharitis or low effectiveness of such therapy, the same drugs can be additionally prescribed in the form of ophthalmic drops.
- Allergic blepharitis involves excluding the patient's contact with allergens, and antihistamines (sodium cromoglycate, Lodoxamide) are prescribed as therapy.
- Meibomian blepharitis is mainly treated with Doxycycline or Tetracycline. Depending on the severity of the disease, treatment can take from 14 days to one month.
- Demodectic blepharitis is treated with Metronidazole or zinc-ichthyol ointment. When using such products to treat children, it is recommended to use ointments not according to the instructions for use, but according to the scheme drawn up by the attending physician.
In severe cases, physiotherapeutic procedures (electrophoresis, magnetic therapy) can be used in parallel with drug treatment. This allows you to achieve results in a shorter time.
In rare situations, surgical intervention may be necessary: this is necessary for eyelid inversions, trichiasis and chalazion, which can develop against the background of blepharitis or be the primary diseases that provoke it.
Your baby is restless, nervous and constantly rubbing his eyes. You notice that there is something wrong with your eyes. Don't delay visiting the doctor. But to fully understand the situation, we will tell you what to do in case of such problems :
- the whites of the eyes turned red;
- the newborn's eyelids are swollen;
- the child was bitten by a mosquito or midge, and the eyelid was swollen;
- the baby's eyes are watery, red and purulent;
- The child's eyes hurt.
Prevention of childhood blepharitis
You can prevent the occurrence of blepharitis in a child if you take the following preventive measures:
- maintain visual hygiene;
- avoid hypothermia;
- keep the child’s room clean;
- avoid excessive visual strain;
- avoid contact with allergens;
- limit contact with sick people;
- eat properly, balanced;
- promptly treat any pathologies;
- strengthen the immune system.
It is necessary to ensure that the child observes the rules of personal hygiene, washes his hands with soap after going outside or playing with animals, does not touch his eyes with dirty hands and uses only his own hygiene items.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Causal factors
Blepharitis in a child occurs for several reasons:
- infection with staphylococcus, streptococcus, eyelash mite;
- allergic reaction;
- the presence of helminths in the child’s body.
Provoking factors contributing to the spread of infection:
- insufficient compliance by the child with personal hygiene;
- decreased immunity;
- the presence of endocrine diseases;
- poor nutrition;
- hypovitaminosis.
The infection can come from the outside, or from internal foci - carious teeth, inflamed maxillary sinuses, chronic otitis media. Infection occurs when the baby comes into contact with birds, street dogs and cats, and people with colds.
Meibomian blepharitis
It is also called marginal and blepharoconjunctivitis. The disease develops due to hypersecretion and inflammation of the meibomian glands.
The following symptoms are of concern:
- itching of the eyelids;
- foamy discharge in the corner of the palpebral fissure;
- fullness of the excretory ducts of the glands with yellowish-gray contents;
- redness of the conjunctiva and skin around the eyes;
- thickening and hyperemia of the eyelid margin.
When pressing on the cartilage, a cloudy pasty secretion comes out of the excretory ducts. In case of severe leakage, squeezing it out is impossible due to its very thick consistency. The contents of the glands become so dense that they cannot exit through the ducts. Subsequently they expand. This leads to the formation of cysts in the thickness of the eyelid. Dysfunction of the meibomian glands often causes stagnation of lipid secretions, which can result in the formation of scars and deformation of the edge of the affected eyelid.
Allergic blepharitis
Blepharitis can be allergic, which occurs after exposure to an allergen on the eyelids, pseudo-allergic as a toxic reaction to a drug, and infectious-allergic, which is a consequence of an infection of bacterial or viral etiology entering the body. Allergic blepharitis is often combined with inflammation of the mucous membrane of the eye - allergic blepharoconjunctivitis.
Allergies can occur to dust, pollen, pet hair, feathers, fluff, insects, household chemicals, etc. Allergic blepharitis occurs acutely and is accompanied by:
- severe itching;
- swelling of the eyelids;
- lacrimation;
- pain in the eyes;
- photophobia.
Almost always the disease is bilateral. In addition, it can be complicated by an infectious disease. A child rubbing his eyes with his hands introduces bacteria to the conjunctiva, resulting in bacterial conjunctivitis.
Demodectic blepharitis
It develops due to damage to the edges of the eyelids by mites of the genus Demodex folliculorum after they enter the ciliary follicles or the genus Demodex brevis, which penetrate the Zeiss glands and meibomian glands. Parasites are clearly visible under a microscope at the roots of the eyelashes. During inflammation, the mite population increases sharply. At the same time, there must be quite a lot of them for the development of the inflammatory process, since asymptomatic carriage of up to 1-2 individuals on 4 examined eyelashes is possible. The diagnosis is confirmed after the detection of at least 4-6 ticks, as well as their eggs and larvae. At the very beginning of the disease, the patient is bothered by unbearable itching, especially in the morning. Later symptoms such as:
- feeling of stinging in the eyes;
- discharge of sticky consistency;
- severe inflammation of the edge of the eyelid, its thickening and redness;
- accumulation of dried secretion in the form of scales between the eyelashes;
- formation of honey-colored crusts.
Prolonged course leads to damage to other structures of the eyeball - the conjunctiva and cornea. Against the background of blepharitis, keratitis, corneal ulcer, and conjunctivitis develop.