08/15/2018 The organ of vision is one of the first to begin to sense and reflect the aging process in the body. Visual acuity decreases, the eye becomes more sensitive to changes in lighting, and the lens becomes cloudy. Cloudiness of the lens of the eye is caused in ninety percent of cases by age-related changes and is called cataracts.
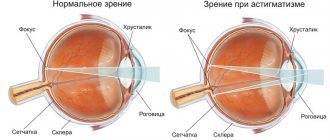
The lens is located between the iris and the vitreous body; it is a natural lens of the human organ of vision, which collects and refracts light rays. It goes without saying that for a lens to function adequately, its transparency is a prerequisite. As long as the lens is transparent, the eye works normally and the person sees a clear picture of the world around him.
- What makes the eye cloudy?
- Symptoms of cloudy lens of the eye
- Clouding of the lens of the eye: is there a treatment?
As a result of clouding of the lens of the eye, cataracts develop, which is characterized by a violation of the transparency of the natural lens of the organ of vision. The name of the disease comes from the ancient Greek word, which literally translates as waterfall. Have you ever seen something through densely flowing water? If so, then you can imagine how a person with cataracts sees the world.
Pathogenesis
The entry of microbes into the eye or their activation leads to the development of keratitis.
An inflammatory gray-yellow infiltrate with blurred edges is formed. Later it transforms into a corneal ulcer, which quickly increases in size and deepens. The pathological process can spread to other parts of the eye. Then scarring of the ulcer occurs with the formation of leukoma (cataract), which threatens blindness.
Features of the clinic:
- one-way process;
- history of chronic eye diseases (conjunctivitis, dacryocystitis, dry eye syndrome);
- acute onset (after microtrauma, within 12 hours there may be a clear clinical picture of inflammation).
Depending on the pathogen, ulcerative keratitis has some differences.
Thus, with pneumococcal, staphylococcal or streptococcal etiology, a creeping ulcer of the cornea of the human eye is formed. The bottom and one of the edges of the ulcer are loosened and soaked in pus. The ulcer “crawls” along the cornea, increasing in size and deepening, until the membranes of the eye are completely destroyed. Fungal keratitis can cause the same consequences.
With diplococcal etiology, the process is more local and superficial and produces fewer complications.
Diagnosis and treatment of the disease
Depending on the symptoms that accompany blue sclera syndrome, diagnostic methods are chosen. After research, experts can determine why the whites of the eyes are blue. This determines which doctor will conduct further examination and prescribe the necessary therapy.
Diagnostic research methods:
- X-ray of the bone apparatus, joints;
- CT scan;
- ultrasound examination of the heart, capable of diagnosing the presence of pathologies present from birth;
- audiogram assessing hearing.
There is no clear treatment option for the syndrome, because this phenomenon is not considered a disease. As therapy, your doctor may recommend:
- massage course;
- therapeutic exercises;
- correction of diet;
- electrophoresis with calcium salts;
- taking a course of chondroprotectors (with an interval of two to three months);
- painkillers that will help relieve pain in bones and joints;
- bisphosphonates, which can prevent bone loss;
- taking medications containing calcium and other multivitamins;
- antibacterial agents if the disease is accompanied by the appearance of an inflammatory process in the joints;
- women with menopause are prescribed the use of hormonal drugs containing estrogen;
- purchase a hearing aid if the patient suffers from hearing loss;
- surgical correction (for fractures, deformation of the bone structure, otosclerosis).
Main symptoms
Parents should pay close attention to this issue and periodically contact an ophthalmologist for preventive purposes. Most diseases tend to progress quickly, and if certain symptoms occur, contacting a specialist is mandatory, including:
- double vision;
- impaired coordination of movements;
- complaints related to eye fatigue;
- squinting;
- dizziness caused by visual stress;
- ability to read only for short periods of time;
- one eye wanders;
- frequent blinking;
- the child's desire to cover his eye with his hand;
- hand-eye coordination is impaired.
An experienced doctor will accurately diagnose the disease and prescribe the necessary therapy. Corrective glasses are used quite often. Parents may be offered to educate their child in a special school, where the necessary exercises to restore vision are done.
Causes of blurred vision in one eye
The root causes that provoked the appearance of blurred image quality in one eye are:
Infectious lesion
Infection by infectious microflora is possible after surgery, failure to comply with hygiene rules, or by air. The pathology develops with additional symptoms and inflammation, and also leads to blurred vision.
Mechanical injury
Due to foreign particles entering the visual organ, damage to the visual organ develops. Trauma leads to a decrease in picture quality. Particles can get into either 1 eye or 2 at the same time. To eliminate foreign particles, it is necessary to rinse the visual organ under running water. For more active tissue regeneration, it is recommended to avoid prolonged work at the monitor and not to overload the visual apparatus.
Inflammatory reactions of the conjunctiva
Temporary one-sided clouding of the picture develops as a result of the inflammatory process in the conjunctival area. Additional symptoms of the pathological condition are swelling of the eyelids and intense lacrimation. In rare cases, the formation of purulent masses is observed.
Barley
An abscess forms in the eyelid and can block the view of one of the eyes. If pathology appears, it is advisable to consult an ophthalmologist to prevent the development of an abscess.
Retinal detachment
The disease develops due to thinning of the retina. A complication of the pathology is complete loss of vision. The root causes of detachment are age-related degenerative processes and diseases of the eyeball.
Overwork
Due to prolonged work at the monitor and overstrain of the eye organs, fatigue of the visual apparatus appears. There may be a temporary blurring of the picture of a one-sided or two-sided nature.
Age-related changes in the lens
After 50 years, changes in the functioning of the visual apparatus begin, which are associated with the age factor. Farsightedness develops and chronic pathologies become more complicated. To reduce destructive processes, it is advisable not to overwork the visual apparatus and balance the diet.
Oncological formation of the nervous system
Neoplasms lead to circulatory disorders and mechanical damage to the visual apparatus. Due to the development of the tumor, loss of vision in the eye that is closer to the disease is possible.
Diabetes
Increased blood glucose levels cause retinal damage. Sugar pathology negatively affects the vascular system of the body. The visual organs may lack nutrients, which leads to one-sided blurred vision.
Cardiovascular diseases
Vessels transport useful components to all organs and systems. Disturbances in the functioning of the vascular system lead to hypoxic conditions or a lack of useful components.
Drying of the conjunctiva
Due to interaction with the environment, the mucous membrane bears the greatest impact of negative factors. As a result of their action, drying out or increased evaporation of moisture from the surface of the visual organs is observed. To eliminate the pathological condition, it is recommended to use appropriate medications as needed.
Glaucoma
Due to the development of glaucoma, the image in one of the organs of vision may become clouded. Jumps in blood pressure inside the eye cavity provoke a deterioration in the functionality of the vascular system of the visual apparatus. To restore picture clarity, a consultation with an ophthalmologist and properly selected therapy is necessary.
Loss of vitreous transparency
Cloudiness of the vitreous body causes hemorrhages in the eye cavity. A characteristic symptom of the pathological condition is the formation of floating spots in front of the visual apparatus. Surgery is necessary to eliminate the clouding.
Pathological conditions provoke the development of anomalies:
- myopia;
- astigmatism;
- farsightedness.
Incorrect or prolonged wearing of contact lenses
As a result of prolonged wearing of lenses, inflammation of the eyeball occurs, and the quality of the image when looking at it deteriorates. Improper hygiene procedures provoke the addition of pathological microflora.
Pathological darkening of the protein
There are many different diseases that can cause the whites of the eyes to darken:
- excessive thinning of the sclera, which may occur congenitally or during the child’s life;
- cardiovascular pathologies leading to impaired blood supply to the eyes;
- pathologies of the body’s excretory system, which eliminate collagen fibers in increased quantities;
- an increase in the number of mucopolysaccharides, which leads to excessive staining of the sclera;
- congenital diseases characterized by changes in connective tissue (Marfan syndrome, elastic pseudoxanthoma);
- diseases characterized by a disorder of the hematopoietic system (iron deficiency anemia);
- pathology of bone tissue (osteitis);
- scleromalacia – excessive thickening of the sclera, which leads to its inflammation; this condition causes vitamin deficiency and metabolic disorders;
- excessive myopia, causing severe visual impairment;
- congenital glaucoma is a disease in which secreted fluid accumulates excessively in the chambers of the eyes, compressing neighboring tissues.
All pathological causes should be treated promptly. Otherwise, complications for the child’s vision organs are possible. The most severe of these is blindness. Initially, parents should contact an ophthalmologist. If the condition is caused by any systemic diseases, he will give a referral to specialist doctors. This could be a geneticist, cardiologist, neurologist, surgeon.
In infants, the color of the tunica albuginea is not normal. It has a grayish tint. The reasons for this can be natural (physiological) or pathological. In the first case, everything goes quickly, in the second, you need to diagnose and begin treatment. Let's find out what signs indicate the need to show your child to a doctor.
The color of the iris in children is formed during the first years of life. Initially, the iris is lighter. Over time, it darkens as melanin accumulates in the body. This pigment does not affect the shade of the scleral (albuginea) membrane. It darkens or loses its luster for other reasons, which can be physiological, which does not pose a health hazard, or pathological, requiring treatment. How to distinguish these two conditions? Let's consider their features.
How to treat eye diseases in children under one year old
After returning from the maternity hospital, parents should closely monitor the development of the baby, not missing the moments of development of visual functions. The first visit to an ophthalmologist lasts up to three months. It is during this time that most congenital diseases are diagnosed. If pathologies have not been established, the next visit to the doctor is planned when the child reaches six months and the main structures of the eye begin to mature, affecting the focusing of the image.
The first symptoms of most diseases before one year of age are:
- the appearance of strabismus;
- slow tracking of a moving object or its complete absence;
- discharge that can accumulate on the eyelids and in the corners of the eyes;
- redness of the tunica albuginea.
As a rule, impaired function is restored with adequate treatment. Therefore, you should not put off visiting a doctor and self-medicate. At the ZIP 100% clinic, after consultation, the doctor will offer the most painless and informative examination. The necessary treatment and surgical intervention are carried out by high-class specialists.
Treatment of corneal opacity (after keratitis)
January 2013.
Continuation of the article on the treatment of the consequences of metaherpes keratitis. The selected treatment option and the diary of events are at the end of the article.
Belmo
(
or leukoma
) is a clouding of the cornea of the eye.
In my case
the cloudiness remained after suffering metaherpes keratitis. We were treated in the hospital with injections in the eye, but the clouding remained. And what to do with it is a big question! Doctors warned that the clouding might remain, but there was no answer to the question of how to treat it.
The thorns are almost exclusively stains
(maculae corneae) of the cornea. Usually being a consequence of previous inflammatory processes of the cornea, its spots present a wide variety in shape, size, color and intensity of turbidity. There are countless transitions from a barely noticeable decrease in the transparency of the cornea to its complete opacity, but in general the following forms of spots are distinguished:
- spot
(albugo), more or less limited and usually pearl-colored, and - a cataract
(leucoma), which is always a scar left after any previous corneal ulcer.
Corneal thorn is a fairly common ophthalmological disease. A cataract is a clouding of the cornea caused by scar changes.
The most common causes of cataract formation are: trachoma, keratitis of various etiologies (viral, tuberculosis and others), trauma (wounds, chemical and thermal burns), eye surgery
.
Depending on the size and intensity of the turbidity, they are distinguished:
- the cataract itself (a dense, extensive clouding of white or yellowish color, located on the entire or most of the surface of the cornea and completely or partially covering the pupil);
- a spot of the cornea characterized by limited opacification,
- cloud (minor, sometimes difficult to discern, clouding of the cornea).
For me, apparently, it’s just a cloud (outwardly the eye looks healthy, the spots are not particularly visible), but even it greatly affects my vision - it’s very cloudy, I can’t read with this eye, for example - it’s cloudy.
The effect of a cataract on vision depends mainly on its location, size and intensity. Thus, when a cloud forms as a result of improper refraction of light rays, a distorted or unclear image of objects appears.
The corneal spot, when located centrally, leads to a significant decrease in visual acuity. The cataract itself may be accompanied by a sharp decrease in visual acuity, up to the preservation of only light perception.
When the cataract is located on the periphery, it affects visual acuity less than when it is localized in the center of the cornea opposite the pupil. Unfortunately, mine is in the center.
An eyesore or leukoma is a clouding of the cornea. It is caused by cicatricial changes in the cornea of the eye caused by a number of reasons. During the process of scarring, the cornea loses its transparency and ability to transmit light unhindered.
An eye with a cataract becomes a specific porcelain-white color. Over time, the color of the cataract changes slightly: it grows a network of blood vessels, undergoes fatty degeneration and becomes yellowish.
A chemical burn or injury to the cornea can also provoke the formation of an eyesore. Alkaline burns are especially dangerous for vision. After them, a person may retain the ability of the eye only to perceive light.
Keratitis is the most common cause of cataracts, since they directly affect the cornea. Keratitis is caused by many reasons. They can be superficial and deep (I had a deep version with a large lesion)
. Deep keratitis often turns into a cataract with inadequate treatment. Superficial ones can ulcerate and leave defects. Keratitis is characterized by the proliferation of blood vessels in the cornea (where they are normally absent), and they do not disappear without a trace after recovery.
During treatment for catarrh, all animal fats should be completely eliminated from food and cholesterol should be kept to a minimum. Most often, a neglected cataract is covered with a thin layer of adipose tissue, which completely deprives the patient of vision. Carrots and blueberries are a must!
Cleansing the eyeball with fresh tea leaves (black tea) also gives positive results. The thorn does not completely disappear, but vision is partially restored and the film becomes more transparent.
In no case should you use active corrosive substances to eliminate a cataract, as this can not only lead to the appearance of a thicker cataract, but also completely deprive a person of his eyes.
Red veins on the whites of the eyes
Contents [Show]
Many people think that the cause of redness of the whites is a burst blood vessel. But it is not always the case. The eyes get tired from the monitor, sleepless nights, and physical activity.
The unpleasant feeling disappears if a person gets enough sleep, takes a walk in nature, limits watching TV, and puts the tablet aside for a while. Red squirrels are observed in babies who have just been born, since they have not yet adapted to life outside the womb.
Veins in the eyes are unpleasant for others and cause pain. Often people buy drops on their own, hoping that they will get rid of redness. Then they are outraged that the drug does not help.
Although there are many small capillaries in the eyeballs, this does not affect the color of the white. If a person does not work at the computer for hours or does not watch TV shows, other factors may cause redness:
- Cold.
- Damage to the mucous membrane.
- Allergy.
- Infectious eye pathologies.
- Decreased immunity.
- Monotonous diet.
The protein changes color and discomfort occurs when the lenses are not removed for a long time.
Is a conjunctival cyst of the eye dangerous and how it is treated is described in detail in the article.
Allergies are the most common cause of redness
With dry eye syndrome, the eyes also acquire a reddish tint. This phenomenon develops after stress, prolonged crying, or hormonal imbalance.
External factors of hyperemia are:
- hard physical work;
- fatigue;
- constant lack of sleep;
- overwork;
- entry of a foreign object.
The mucous membrane is irritated by the presence of tobacco smoke, dust, bright light, strong wind, and cold air. Women's eyes often turn red after applying mascara to their eyelashes or applying eye shadow to the eyelid area.
The article is for informational purposes only. Medicines that will relieve discomfort should be prescribed by an ophthalmologist.
A comprehensive answer to the question of young mothers - when will strabismus in a newborn go away.
Overwork has a negative impact on the functioning of all body systems.
A congenital anomaly that can cause a lot of inconvenience is iris coloboma.
Once pathogenic microbes enter the body, they cause various pathologies. Pathogens in the form of foods, chemicals, pollen, and some drugs provoke the development of allergies. The type of stimulus is determined by making special tests. After this, the doctor prescribes medications that will cure the disease and eliminate unpleasant symptoms.
Whites turn red when you have a cold. When it passes, the burning and itching disappear. Veins are formed when there is a deficiency of ascorbic acid, as the capillaries swell and become brittle.
High intraocular pressure not only leads to changes in the color of proteins, but also to the development of cataracts and disruption of the functions of the lens.
Find out when the use of Combigan eye drops is justified here.
Conjunctivitis can be caused by a bacterial or viral infection
A double blow to inflammation and infection - Combinil Duo eye drops.
When harmful microorganisms get into the eyes, the outer membrane becomes inflamed and conjunctivitis occurs. Pathology happens:
- allergic;
- viral;
- bacterial.
To prevent the infection from spreading to other areas, hygiene rules must not be ignored.
With blepharitis, the pathological process occurs in the eyelash follicles, then the cornea becomes inflamed. The eyelids are very itchy and the whites turn red.
Keratitis develops after injuries, due to vitamin deficiency, when infected, accompanied by:
- abnormal lacrimation;
- photophobia;
- hyperemia.
The same symptoms are present with iridocyclitis, when the iris becomes inflamed.
The presence of such symptoms requires immediate comprehensive diagnosis
Episcleritis affects beautiful ladies. Pathologies lead to it in the form of:
- gout;
- tuberculosis;
- lupus erythematosus;
- Rosacea.
With this disease, the whites acquire a pinkish tint, and there is pain when pressing on the eyelid.
In infectious pathologies the following is observed:
- burning and stinging;
- abnormal tearing;
- discharge of pus;
- dry syndrome;
- discomfort in the bridge of the nose or forehead;
- painful blinking.
Such symptoms do not occur after overwork, prolonged sitting at the monitor, or lack of sleep. These are signs of a serious illness caused by viruses or bacteria.
Pain when blinking may indicate the development of conjunctivitis
Important information before replacing the lens is the lifespan of the artificial lens of the eye.
An unpleasant sensation in a child’s eyes often appears if a foreign body in the form of an insect, sand, or dust penetrates the mucous membrane. Proteins turn red due to allergies, which are common in children.
In infants, the tear duct sometimes becomes blocked. It is up to the doctor to clean it. Spots in such children appear during pressure during childbirth. They disappear after a few days.
Red proteins and photophobia are observed in uveitis, when the choroid becomes inflamed. This pathology is very dangerous, as the baby runs the risk of losing his sight.
For instructions on how to properly put on lenses for the first time, follow the link.
Friction is a common cause of temporary discoloration of the sclera.
Primary self-diagnosis before an urgent visit to an ophthalmologist - symptoms of eye cataracts.
No matter how busy a person is with work, he needs to find time to rest his eyes. Every hour you need to look up from writing texts, from the computer, move your gaze in different directions, change the fixation of focus. It is necessary to arrange the workplace in advance so that there is good lighting and the monitor screen is correctly positioned.
Preparations in the form of drops Tobradex, Vizin, Floxal relieve discomfort and redness after overwork. You should not use them often, since such medications do not cure the disease.
With dry syndrome, it seems as if something has gotten into the eyes. This sensation occurs when the tear secretion is produced in small quantities. Oxyal and Hydromellose drops help increase their synthesis.
Whites turn red due to allergies. If the pathogen is unknown, or there is no way to eliminate it, you need to wear glasses so that they fit tightly, and often rinse the mucous membrane with boiled water. Antihistamines in the form of Claritin, Lorinden, Diazolin relieve discomfort. The ophthalmologist prescribes Allergodil, Cromohexal.
Many people wear contact lenses. They need to be removed at night. Apply moisturizers to your eyes.
Effective methods for treating strabismus in adults are described in detail in the article.
Ofloxacin is a broad-spectrum antibiotic
Bacteria, viruses and fungi provoke infectious pathologies. The eyes are instilled with sulfonamides or tetracycline-based antibiotics or cephalosporins. Oftalmoferon effectively fights pathogenic microflora.
If the proteins turn red due to autoimmune and endocrine disorders, therapy is carried out under the supervision of a specialist.
Discomfort that is associated only with overwork can be relieved at home:
- chamomile compresses;
- lotions made from raw potatoes;
- black tea;
- pieces of ice.
The redness usually goes away quickly. Severe complications occur with infectious eye infections.
Chronic conjunctivitis can cause clouding of the cornea. With trachoma, which is caused by chlamydia, if treatment is ignored, a cataract forms, which sometimes leads to loss of vision.
The correct approach to combating glaucoma is Cosopt eye drops.
Poor-quality cosmetics can cause allergies and cause swelling and redness of the sclera of the eye.
There are many small vessels located on the whites of the eyes. They can be seen when the capillaries expand and reach the surface of the mucous membrane. Red streaks also appear during normal fatigue, but they may indicate a serious infectious pathology such as conjunctivitis, which is caused by bacteria or viruses.
Koch's bacillus, having penetrated the mucous membrane of the visual organ, leads to abnormal lacrimation and damages the membrane. Hemorrhage occurs in the protein, which is observed in the form of red veins. Lack of treatment for tuberculosis, which occurs under the influence of this bacterium, threatens not only deterioration of vision, but also its complete loss.
Red veins (photo)
The reasons for the expansion of capillaries are:
- herpetic eye lesions;
- predisposition to allergies;
- high pressure;
- metabolic disease.
Vessels rupture and hematomas form due to head injuries, concussions, and contusions to the visual organ. The process is accompanied by pain and severe burning.
Complex product containing antibiotic and corticosteroid
You can prevent redness of the white and the appearance of veins by following simple rules. Everyone can do them:
- Do not rub your eyes with your hands.
- When working with numbers and at the monitor, take breaks to rest the visual organ.
- Don't forget about proper sleep.
- Do not abuse alcohol.
- If possible, avoid strenuous physical activity.
Disposable vials ensure the most hygienic use of the drug
Red whites in the eyes not only spoil a person’s appearance, but can also lead to serious complications, such as vision impairment, when their appearance is caused by an infection. If after rest the discomfort does not go away, the veins do not disappear, you need the help of a doctor.
The appearance of red blood vessels on the whites of the eyes often confuses patients and makes them think about the reasons for such a deviation. Some patients believe that this manifestation indicates that the blood vessels in the eyes have burst, but this opinion is completely erroneous. The situation of capillary rupture is much more dangerous and often entails more serious consequences.
This problem is familiar to many
You should not give in to panic, you need to know and always remember that the organ of vision contains many vessels; we can say that it is all dotted with them. Under normal conditions, the capillaries of the eye are hidden and cannot be seen without additional equipment, but they can appear due to many etiological factors.
The etiology for the manifestation of such a deviation may be an infectious disease or simple ophthalmic fatigue. Experts say that patients who do not observe occupational hygiene when working at a computer encounter this problem quite often.
Despite the fact that such a deviation rarely poses a danger, it is still necessary to visit an ophthalmologist. Only a doctor can select a medication that can help the patient cope with the problem. You need to figure out why red blood vessels may appear in the eyes.
Sometimes red blood vessels become an unpleasant surprise in front of the eyes - such a formation frightens the patient, because every person wants to preserve visual functions in full. There can be many risk factors for such a manifestation, the most common of them are presented in a comparative table, which will help you understand the methods of eliminating the problem and explain what the danger is in each specific case.
An ophthalmologist performs an examination
Photos clearly demonstrate the type of pathology:
Attention! Despite the fact that traditional therapy offers many methods to combat the disease, such recommendations should not be used without consulting a doctor. It is important to remember that the treatment of ophthalmic pathologies is a complex process that requires comprehensive influence. Therapy methods should be used under the supervision of an ophthalmologist.
Self-selection of medications is unacceptable
If redness occurs, you must consult a specialist; only a doctor can determine the cause and choose the right treatment. Such a symptom can be dangerous if there is an infectious or viral etiology.
If the patient continues to live his usual life and attend a work or educational group, he will act as a spreader of the infection. The video in this article will explain why the vessels of the eyeball turn red.
In a situation where the appearance of red blood vessels in the eyes does not indicate the presence of a disease, you can get rid of them quite simply and quickly. The main etiology in such situations is overwork.
Healthy sleep is a guarantee of good health.
Cosmetics should be thoroughly washed off from the eye area before going to bed.
Fresh air is necessary for all organs and systems, including the eyes.
Giving up bad habits will prevent health problems.
It's important to take breaks during long periods of work
Artificial tears will help preserve your vision.
Applying ice cubes helps narrow the capillaries.
You need to pay attention not only to muscle training, but also to exercises to improve blood circulation
The drug Blueberry Forte is the optimal composition for restoring vision.
Sunglasses are not only stylish, but also useful.
The following recommendations will help you avoid serious vision problems and help prevent the detection of broken capillaries.
The use of artificial tears is a means of preventing the development of blepharitis.
Drug treatment of hyperemia depends on the causative factors that provoked the disease, for example:
- For infectious diseases, doctors recommend the use of antibacterial drugs.
- If the detection of broken capillaries in the eyes is a consequence of allergies, use antihistamines and moisturizers. At the same time, they ensure isolation of the patient from sources of allergies.
- For inflammatory pathology, steroid and non-steroidal drugs are used.
Attention! A specialist must select a specific drug for treatment.
If a vessel in a patient’s eye bursts, the cause is determined and measures are taken to eliminate it. No special drug therapy is required.
The antihistamine composition helps relieve redness of the eyes.
Local preparations
Modern pharmacology presents to the demanding patient a wide range of drugs that can cope with ophthalmological lesions of various origins.
Do not purchase medications on the advice of a pharmacist.
If redness occurs in the whites of the eye, agents from the following pharmacological groups can be used:
- Moisturizing drops - used when the adequate ability to produce tear fluid is reduced. The price of the drugs is low, the products are suitable for regular use.
- Vasoconstrictors - used to eliminate redness from the eye area.
- Vitamin compositions - used for the prevention of dystrophic disorders.
- Compositions with an antihistamine component are used for red eyes and allergic lacrimation.
- Antibacterial compounds - used for inflammatory processes.
- Antiviral agents - the action is aimed at eliminating pathogenic viruses.
- Combined - used when vasodilation of unknown origin occurs. Instructions for use indicate the likelihood of side effects.
Attention! You should not attempt to determine the cause of the pathology on your own. Unreasonable use of ophthalmic drops can become a factor in the development of serious problems.
The use of traditional methods for eliminating burst capillaries can be used only after the etiology of the deviation has been established. The method can only be used if redness of the eyes is a consequence of excessive fatigue.
The power of plants in the fight against ophthalmic pathologies.
Among the common time-tested methods are:
- applying fresh cucumber pulp to the eyelid;
- compresses from tea bags;
- rubbing the eyes with a strong decoction of oak bark or chamomile;
- rubbing around the eye area with ice cubes.
- using cotton swabs with olive oil.
The listed methods can only be used after consultation with your doctor.
It is important to remember that red capillaries on the whites of the eyes can be a symptom of one of the dangerous diseases, so you should go to the hospital immediately after such a manifestation. Only a doctor, after an initial examination, laboratory and instrumental research methods, will be able to establish the cause and select the optimal method for eliminating it.
When red streaks appear on the whites of the eyes, most often people think that their blood vessels have burst. But this opinion is wrong. When a blood vessel ruptures, it looks different and the consequences are much more serious.
Obvious manifestations of blood vessels indicate inflammation of the eyes. It is worth mentioning that there are many reasons for inflammation - from overwork of the body to a severe infectious disease.
Before you panic, you need to know that the white of the eye is completely covered with blood vessels. In normal condition they are not visible. But during periods of overwork or infection, the vessels dilate and appear on the surface of the protein. Visual disturbances, changes in color, protein structure or pupil are the consequences of certain disorders, which means a visit to an ophthalmologist is simply necessary.
Antibacterial drugs are used for treatment; the ophthalmologist prescribes a course of antibiotics. The use of these drugs accelerates processes in the body aimed at fighting infection. In folk medicine there are many recipes for the treatment of conjunctivitis. But the main effect of such drugs is aimed at relieving symptoms or treating the consequences of conjunctivitis, and not at treating the root cause of the disease.
Koch's bacillus or tuberculosis. Unfortunately, this disease affects not only the human lungs. Koch's bacillus can also get on the mucous membrane of the eye and cause quite unpleasant consequences. With this disease, a person not only experiences increased lacrimation, which is accompanied by painful sensations, but also micro-tears of the membrane itself occur. As a result, microscopic hemorrhages occur in the white of the eye - red streaks appear on its surface. This is a rather dangerous disease, and it can also be transmitted to others.
At the first suspicion of this disease, you should immediately consult a doctor. Tuberculosis does not go away without consequences. Therefore, systematic examinations and comprehensive treatment are necessary to prevent the disease. Koch's bacillus is a fairly strong, stable bacterium that can adapt to any living conditions. An incomplete course of treatment or failure to comply with preventive measures will cause a relapse. Repeated illness causes even more harm to the body, and vision can deteriorate significantly. In rare cases, relapse of the disease leads to complete loss of vision.
Viral diseases lead to eye inflammation. When a person has the flu, in addition to a cough and runny nose, the whites of the eyes may turn red. The reason for this is general malaise and fatigue of the body, weakened by the disease. Once a person recovers from the flu, the redness of the whites goes away. To help your body quickly cope with a viral disease, you need a course of antiviral drugs.
Viral diseases also include herpes infections. It is difficult to cope with such a disease on your own. In this case, the person needs serious treatment and observation by a doctor.
Predisposition of the body and genetic inheritance to allergies If the body is weakened, the immune system does not work at full strength, the person is predisposed to various allergic reactions. In this case, it is recommended to take antihistamines, but under the supervision of a doctor. Thanks to these drugs, the body produces more of the hormone, which reduces the external manifestations of the allergen or irritant.
Disturbance of internal processes in the body When metabolism changes and the endocrine system is disrupted, red blood vessels in the eyes are one of the symptoms. If red eyes occur frequently and for no apparent reason, get a medical examination to check your general condition and check your blood glucose levels. For diabetes mellitus, it is recommended to use vasoconstrictor eye drops to relieve redness of the whites.
In hypertensive patients, high blood pressure is often accompanied by redness of the proteins. The blood vessels of the eye become inflamed and appear on the white of the eye.
Injuries and bruises in the eye area Head injuries, bruises in the eye area, and concussion lead to rupture of blood vessels. In this case, their inflammation is a consequence of mechanical action. The white of the eye is not only redder, but bruises form on it. In this case, it is recommended to use anti-inflammatory and painkillers.
Red vessel in the eye
Usually, when a person notices a red vessel in the eye, he thinks that a hemorrhage has occurred.
However, serious reasons are needed for a capillary to rupture; why red vessels appear can be explained by a number of other reasons.
When the eyes are exposed to unfavorable factors, its superficial vessels dilate. If the redness has spread to its entire surface, and other symptoms have been added: pain, a sense of schedule, increased lacrimation, then you need to consult a specialist.
Often red vessels in the eyeball appear during overexertion, chronic fatigue and do not require special treatment.
It is enough to ensure peace and use natural tear preparations.
Red eyes are a common symptom of many eye diseases.
Therefore, if you notice such a sign in yourself, then in the absence of logical explanations, you need to consult an ophthalmologist. So, the reasons for redness may be:
- infectious eye diseases - keratitis, uveitis, conjunctivitis, blepharitis;
- allergies to house dust, smoke, pollen, etc.;
- injury to the eyeball or hypothermia;
- residual symptoms of previous eye infections;
- presence of a foreign body;
- eye fatigue, long and intense work at a computer monitor;
- some medications may cause redness of the whites of the eyes;
- lack of sleep and chronic fatigue;
- increased physical activity during sports or during childbirth in women.
Capillary rupture
In addition, the red vessels of the visual organ may be the result of hemorrhage, hypertension or diabetes. With these diseases, the elasticity of all blood vessels in the body suffers greatly, therefore, with a sharp jump in blood pressure, which brings more blood into the vessel. Insufficient elasticity in this case leads to it breaking. The causes of such pressure surges may be stress, nervous tension or worsening weather conditions. If this happens repeatedly, you should consult a doctor to examine the vessels and prescribe measures to prevent this from happening.
Sometimes, capillary ruptures can occur due to a lack of ascorbic acid in the body, which makes the vessels more fragile and the walls of the vessels less strong.
The lifestyle of a modern person, when the eyes receive high stress, for example, when working with a computer, leads to dry eye syndrome. Tear fluid moisturizes the ocular surface and if there is a lack of it, it dries out, irritation appears, and the blood vessels turn red. Dry air can also cause insufficient hydration of the eyeballs; this is the air produced by air conditioners. Also, wearing contact lenses can injure the cornea and lead to swelling and redness of the blood vessels.
A more correct way to narrow blood vessels is to use cold lotions. Cold reflexively contracts the blood vessels, and they narrow, without becoming addictive. For lotions, you must use clean boiled water, and wash your hands before the procedure. A moistened cotton swab or handkerchief should be applied to the eyes for a few minutes.
You can also use ice by wrapping it in a cloth. In addition to plain water, you can use compresses with tea and decoctions of medicinal herbs. In this case, alternating warm and cold compresses gives a good effect, so the vascular wall trains and becomes stronger. Tea should only be taken loose leaf, not flavored. Plants include chamomile, blue cornflower, mallow, linden and mint.
Proper diet and daily routine You should take care of a healthy diet, because the lack of vitamins and microelements has a bad effect on the strength of the blood vessels in the eyes. First of all, eat more fruits and vegetables. These are all red, yellow, orange and green fruits and vegetables, they contain many beneficial vitamins for eye health. It also includes fish, nuts, eggs and berries (blueberries). After consulting with a doctor, he may prescribe special vitamin and mineral complexes.
Properly alternate between workload and rest during the working day. Don't let your eyes become overstrained. Their daily routine is of great importance for their health. Sleep should take at least 7-8 hours a day. This is necessary for the conjunctiva to recover after the day. During the day, also provide your visual organs with rest.
When working with a computer, use anti-glare glasses and take breaks at least every half hour. You can do a simple eye exercise.
- sit up straight, relax and move your eyes left and right, then up and down;
- then make circles with your eyes clockwise and counterclockwise;
- Blink quickly, then close your eyes and relax. Repeat several times;
- look first at an object in the distance, and then move your gaze to a closer object;
- Cover your eyes with your fingers and massage them gently.
Protecting your eyes from harmful environmental factors In summer, be sure to wear sunglasses with a good UV filter. Don't let your eyes get too cold in winter. Avoid getting cigarette smoke, dust and litter in your eyes. Treatment of diseases that cause red eyes
For allergies, antihistamines
Above, cases were described where the cause of red blood vessels was not an infectious or other systemic disease. If this is the reason, then treatment should be appropriate. If you have an infection, do not touch your eyes or rub them - this can aggravate the disease and spread the infection process.
If redness of the organs of vision is caused by allergies, then you should take antihistamines. With allergies, in addition to redness, itching appears. Vasoconstrictor antihistamine drops can now be purchased without a prescription. However, they cannot be used for a long time. Use them several times a day.
What to do if a person has cloudy eyes and vision loss?
White color with a pearlescent sheen is the normal characteristics of a healthy eye. The mucous membrane covering the outside of the eyeball is normally transparent and shiny. A person's eyes become cloudy for a number of reasons.
Causes and symptoms
Blurred vision is a symptom of ophthalmological diseases. In this case, the visual organ may remain visually normal, or may become cloudy. Visually, the whites of the eyes may become cloudy after hard work at a computer monitor or fatigue. This condition goes away after rest.
Additionally, symptoms may appear: floaters, decreased visual acuity, double vision, fatigue, foreign body sensation. Visually you can see lacrimation, an expanded vascular network, and loss of shine.
Overwork
The person notes eye fatigue, blurred vision, and a feeling of sand. Visually: redness of the sclera, lacrimation. This happens from lack of sleep, prolonged work at the computer, watching TV, or working with small objects. A cloudy look is characteristic of dry eye syndrome.
Ophthalmic diseases
External clouding occurs due to diseases associated with disruption of the structure and function of the visual organ. As a rule, they are accompanied by decreased visual acuity, blurred vision, and blurred vision.
- A cloudy pupil occurs with cataracts due to a clouded lens.
- Cloudiness of the cornea is characterized by the formation of a white spot - a cataract.
- Cloudy, reddened whites of the eyes in humans can be caused by inflammatory causes (conjunctivitis, uveitis and others).
- Vitreous opacities, glaucoma, myopia and hypermetropia are diseases characterized by blurred vision. However, the eye itself is visually normal.
- Mechanical damage. After an injury, a foreign body, or a burn, the protective film of the eyes is damaged, vision becomes cloudy, and the conjunctiva turns red.
- Age-related thinning of the membranes of the eyeball gives the sclera a blue tint.
General diseases
The sclera of the eyes become cloudy due to blood acidosis (a shift in blood pH to the acidic side). Acidosis is caused by intoxication of the body, kidney disease, decompensation of diabetes mellitus, thyrotoxicosis. Externally from the visual organ: loss of shine, pale mucous membrane.
Improper care
After wearing lenses for a long time, your eyes become cloudy. Poor care, incorrectly selected glasses, as well as the use of low-quality cosmetics and makeup removers can cause a pathological symptom.
Natural periods
Cloudy eyes are possible in a newborn; later they become brighter and can change the color of the iris. Cloudiness occurs in pregnant women due to changes in the woman’s hormonal system.
What to do if your eyes are cloudy
Episodic causes (lack of sleep, overwork) cause temporary clouding. Drug treatment is not required, it is enough to rest the visual organ and get a good night's sleep. Limit the time you spend at the computer and TV. Take breaks during high workloads and do gymnastics.
Moisturizing eye drops: Visine, Systane will help quickly relieve signs of fatigue.
Treatment of inflammatory diseases requires the prescription of antibacterial, antiviral, and anti-inflammatory drugs. If a foreign body gets in, you need to remove it and apply Albucid antiseptic drops.
Blurred vision due to refractive errors is corrected with glasses or contact lenses. Glaucoma is treated with drops to lower IOP.
The operation is performed when drug treatment is ineffective and there is serious damage to the organ of vision. Typically, cataracts and cataracts require surgery. For cataracts, the cloudy lens of the eye is replaced with an artificial lens. At the initial stage, corneal clouding is treated with regenerating drugs. If there is no effect, then keratoplasty is performed.
Maintain hygienic lens care. Exercise the load on the visual organ in doses, with breaks. Take vitamin complexes in the form of tablets and drops for preventive purposes.
Additionally, we invite you to watch the video. Find out how to keep the whites of your eyes white after 45 years:
If one or both eyes have blurred vision, or if other symptoms occur, consult an ophthalmologist. Treatment of diseases in the early stages helps preserve visual functions.
Gray protein color as a sign of disease
If after six months the veil in the baby’s eyes has not disappeared, and the whites remain gray, you will need the help of an ophthalmologist. Usually, doctors do not pay attention to the gray whites around the edges of the eyes and consider this not a dangerous phenomenon, however, they will still have to get advice. The gray edges of the white of the eye may turn out to be an individual feature of the baby, inherent only to him.
It’s worse when all or most of the protein turns gray. A clear sign of the disease can be pronounced gray whites of the eyes in an infant.
The gray-blue tint of a baby’s eyes can be a sign not only of ophthalmological diseases, but also of other pathologies. If the sclera or white of the eye has a pronounced gray-blue color, the baby must be shown to an ophthalmologist and then taken for an ultrasound: the fact is that children with a gray tint to the white or sclera often suffer from cardiovascular diseases.
The baby must be examined by doctors if his sclera is transparent and the blood vessels of the eye are visible through it. The gray color of the whites in children may be a symptom of “Rachitis” - then, after being in the fresh air, the whites may turn white
Do not forget that rickets is accompanied by other symptoms that must be paid attention to, and not just the appearance of a gray coating on the whites of the eyes
The white of the eye is normally white. A change in the color of the sclera may indicate that a person is sick. Blue sclera indicates that the white membrane of the eye, which consists of collagen, has become thinner. The vessels underneath become translucent, turning the whites blue. This phenomenon is not considered a separate disease, but in some cases blue sclera is one of the symptoms of the disease. Causes of the syndrome
The symptom of blue sclera often appears in children from birth due to existing disorders at the gene level. The white of the eye can be blue, gray-blue or blue-blue in color. This phenomenon is often transmitted hereditarily, so it does not always indicate that the child is seriously ill.
If the syndrome is congenital, specialists detect it immediately after birth. When the baby is completely healthy, after six months the pathology recedes. In the presence of serious diseases, the color of the whites of the eyes does not change by this time. Blue protein syndrome is often accompanied by other problems with the visual organs (hypoplasia of the iris, cloudy cornea, glaucoma, cataracts and others).
The main reason for blue sclera is the translucency of the lining of blood vessels through the sclera, which has become transparent due to thinning. This pathology is characterized by the following changes:
- the sclera is too thin;
- the amount of collagen and elastin decreases;
- the appearance of a characteristic color in the whites of the eyes, which indicates a high level of mucopolysaccharides. This indicates the immaturity of fibrous tissue.
Why are my eyes cloudy?
Eyes are an indicator of human health.
Detection of clouding is a serious reason to visit an ophthalmologist.
Cloudy spots may indicate old age. In this case, the lens becomes cloudy and the spot acquires a bluish tint. This condition may also indicate a pathological process in the organs of vision.
Cloudy whites of the eyes
Cloudy vision is manifested by pallor of the connective membrane, hyperemia or clouding of the protein. A person’s gaze loses its shine, a foreign body is felt, as if sand had been poured into it.
We recommend reading: Blue whites of the eyes
The change in shade is associated with a change in the chemical composition of the blood; this occurs with prolonged stay indoors or with general fatigue. The contour between the cornea and the white is erased.
Cloudiness is localized in any part of the visual analyzer. It can be found in the central and peripheral field of vision. It may affect only part of the eye, sometimes the spots are located chaotically.
This condition is accompanied by the following clinical picture:
- headache;
- eye pain;
- nausea;
- cobwebs before the eyes;
- flashes.
Red and cloudy eyes are the cause of many pathological conditions. Simultaneously with these signs, others appear, indicating a specific disease. This may be a deterioration in visual perception, disruption of a certain part of vision, burning, itching and other symptoms.
Sometimes cloudy whites of the eyes go away after rest. In other cases, double vision, fatigue, and severe lacrimation appear.
Causes of cloudiness
There are many reasons that can cause cloudy eyes. Often this condition occurs against the background of long-term chronic infectious lesions, chemical or mechanical injuries.
A common cause of the condition is overwork and chronic fatigue. They are characterized by a foreign body sensation, lacrimation, and redness.
Dry eye syndrome may cause blurred vision. The symptoms are similar to those of overwork, but there is no lacrimation.
Cloudy whites of the eyes cause acidosis. It develops in diabetes mellitus, thyrotoxicosis, and kidney diseases.
Causes of cloudy eyes in a child
In newborns, the whites of the eyes are not white, but cloudy. This is considered normal; later they acquire a natural shade.
If the visual organs are completely cloudy at the birth of a child, this is also normal. After 3-7 days they will turn white, the color of the iris will also change.
Cloudiness is possible with conjunctivitis, measles, injury, herpes virus.
Surgery
Surgical intervention is prescribed for common ophthalmological problems. If the visual organ is cloudy, surgery is performed on the lens. Lens removal is more common for cataracts, myopia and hypermetropia.
It is removed and an implant with powerful refractive power is installed in its place. The procedure is safe, but has some complications.
The operation to install an implant requires postoperative rehabilitation. It lasts about 2–3 weeks. During this period, you should limit physical activity, rest more, and do not overload them with reading or watching TV.
Vision is restored immediately, and if necessary, glasses for vision correction are selected. Glasses can be worn 5 days after surgery.
Special drops are prescribed to speed up healing and prevent infection.
Microsurgical operation (phacoemulsification) involves fragmentation of the lens substance with ultrasound. Then it is extracted using irrigation-aspiration method. You should prepare properly for the operation. Its advantage is reduced rehabilitation time.
Prevention
The risk of developing a defect can be reduced if you carefully monitor the hygiene of the eye area. To avoid cloudy eyes, it is necessary to use suitable correction products when working with a computer or small parts.
Ophthalmological problems can be prevented by preventing visual fatigue by contacting an ophthalmological center in a timely manner.
Poor vision significantly worsens the quality of life and makes it impossible to see the world as it is.
Not to mention the progression of pathologies and complete blindness.
MNTK "Eye Microsurgery" published an article on non-surgical restoration of vision up to 90%, this became possible thanks to...
Read more Was this article helpful?
Manifestations
List of diseases in a child or adult:
- Connective tissue: Elastic pseudoxanthoma.
- Syndromes: Lobstein – Vrolik;
- Ehlers-Danlos;
- Marfana;
- Lobstein-Van der Heve.
- Bone structure and blood: Diamond-Blackfan anemia;
- Paget's disease;
- acid phosphatase deficiency;
- IDA (iron deficiency anemia).
- Eye pathologies: scleromalacia;
- iris hypoplasia;
- myopia;
- corneal abnormalities;
- congenital glaucoma;
- inability to distinguish colors;
- anterior embryotoxon.
Manifestations of diseases with connective tissue lesions:
- bluish or dark blue whites of the eyes;
- bone fragility;
- hearing impairment.
The following symptoms are typical for blood diseases:
- retardation in physical and mental development;
- frequent colds;
- increased activity;
- thinned tooth enamel.
The blueness of proteins in most patients is associated with pathology of the ligamentous-articular apparatus, characterized by fragility of bones and poor healing of fractures. There are 3 types of such lesions, which are symptoms of blue sclera:
- Severe stage of damage. Fractures in a child occur already during intrauterine development. In most cases, they lead to death before birth or in infancy.
- Fractures and dislocations at an early age up to 2-3 years. They are formed from external influences without much effort and deforming the skeleton.
- Fractures appearing after 3 years. In adolescence, their number and danger of occurrence decrease greatly.
The whites of the eyes have this name because they are normally white. When a person is sick, the sclera can signal this by changing its color. Blue sclera is the result of thinning of the white membrane of the eye, consisting of collagen. Because of this, the vessels located under the membrane are translucent, giving the whites of the eyes a blue tint. Blue sclera is not an independent disease, but in some cases it is a disease.
Blue squirrel: what does it mean? With this phenomenon, the white of the eye acquires a blue, gray-blue or blue-blue tint. It often occurs in newborns, and is often caused by genetic disorders. This feature can be inherited. It is also called the “transparent sclera”. But it does not always indicate that the baby has serious illnesses.
With congenital pathology, this symptom is detected immediately after the birth of the child. In the absence of serious pathologies, this syndrome usually recedes by six months of the baby’s life.
If it is a symptom of any disease, then by this age it does not disappear. In this case, the size of the organs of vision, as a rule, does not change. Blue white of the eyes is often accompanied by other pathologies of the visual organs, including iris hypoplasia, anterior embryotoxon, corneal opacification, color blindness, etc.
The main reason for the appearance of blue protein syndrome is the transillumination of the choroid through the thinned sclera, which becomes transparent.
This phenomenon is accompanied by the following changes:
- direct thinning of the sclera;
- reduction in the number of collagen and elastic fibers;
- metachromatic coloring of the ocular substance, indicating an increase in the amount of mucopolysaccharides. This, in turn, suggests that the fibrous tissue is immature.