Corneal crosslinking is the effect of riboflavin and ultraviolet rays on the thinned cornea, as a result of which it becomes stronger and thicker.
The technique is designed specifically for people with keratoconus or complications after Lasik laser surgery.
Its high efficiency has been proven. In Russia, the procedure appeared relatively recently, although it has been developing abroad since the beginning of 2004. The indications for the procedure must be determined by the doctor after a lengthy examination and diagnostic tests.
Indications for surgery
The procedure is not indicated for all categories of patients; it is performed in the following cases:
- keratoconus – protrusion of the cornea forward, causing it to become very thin, increasing the risk of complete tissue rupture;
- dystrophy - disruption of the nutrition of the eyeball through the vessels, resulting in necrosis (death) of tissue;
- complications after Lasik surgery, when the cornea becomes thinner after mechanical damage from the action of a surgical scalpel or laser;
- autoimmune diseases, due to which one’s own immune cells damage and destroy corneal tissue;
- Bullous keratopathy is a disease due to which the cornea swells, its epithelial layer is damaged, which forms a foreign formation.
After surgery, the cornea is not completely restored, but its quality and thickness are significantly improved.
Contraindications
Surgery is contraindicated for the following conditions and diseases:
- excessively small thickness of the cornea, less than 400 microns, but more modern methods have now been developed, as a result of which the procedure can be performed even with such a cornea;
- high myopia and farsightedness, in the presence of which surgery is not performed even with normal corneal thickness;
- age up to 16 years;
- pregnancy, lactation;
- presence of scar tissue;
- conjunctivitis of an allergic nature, in which the cornea becomes severely inflamed, which worsens the patient’s condition (temporary contraindication).
Other temporary contraindications are also possible. For example, viral and infectious diseases, exacerbation of a chronic disease. The procedure can be performed after the person has fully recovered.
Crosslinking
The cross-linking technique was invented by Professor Theo Sailer. The essence of the cross-linking method is to strengthen the cornea and stabilize keratoconus using a special laser. During this treatment, additional chemical bonds arise between the collagen fibers that form the structural framework of the cornea, which enhance the mechanical density of the entire cornea. Thus, new corneal fibers are formed, crossing each other. The cornea becomes denser and can maintain its shape, preventing further progression of keratoconus.
The basis for research in this area was a series of works devoted to the effect of “gluing” collagen fibrils with the formation of dimers from two a-chains under the influence of various external factors: enzymes, ozone, ultraviolet radiation.
This effect is the result of an oxidative mechanism accompanied by the release of various free radicals. It turned out that, unlike other methods of inducing “gluing,” ultraviolet radiation stimulates the formation of singlet oxygen, which, unlike the hydroxyl radical, does not cause concomitant degradation of CNBr collagen proteins. In addition, the ability of ultraviolet radiation to stimulate the production of matrix metalloproteinases was confirmed. The experiment revealed that in the presence of riboflavin, the degree of absorption of ultraviolet radiation in corneal tissue increased from 32% to 95%, and damage to collagen proteins under the influence of ultraviolet irradiation was minimized.
The first studies in ophthalmology began in 1990 with an attempt to evaluate the possibility of biological oxidative “gluing” of corneal collagen under the influence of enzymes, heat or radiation of a certain wavelength, which would lead to increased resistance of stromal collagen. It is known that a similar mechanism of compaction and thickening of collagen fibers by approximately 4.5% accompanies the “aging” of the cornea, and also occurs in diabetes mellitus and is associated with activation of glycosylation in tropocollagen molecules. The mechanism of induction of collagen “gluing” in diabetes mellitus includes a cascade of biochemical oxidative reactions reflecting non-enzymatic glycosylation.
Currently, riboflavin (vitamin B2) is used for cross-linking as a photosensitizer, activated by ultraviolet radiation in the wavelength range of the A spectrum. The choice is due to the non-toxicity of riboflavin for corneal tissue, the availability of the drug and the preservation of transparency when applied to the cornea.
Riboflavin has three absorption peaks for ultraviolet radiation, at wavelengths of 270, 366 and 445 nm. However, exposure at a wavelength of 370 nm results in a greater energy effect, since over 95% of the radiation is absorbed.
In the process of photochemical crosslinking, riboflavin performs two functions: firstly, it absorbs ultraviolet radiation, and secondly, it releases short-lived free radicals of atomic oxygen under the influence of radiation. Under the influence of atomic oxygen, collagen amino acids undergo deamination and form covalent bonds with each other.
Crosslinking procedure technique
Corneal collagen crosslinking is performed on an outpatient basis using local instillation anesthesia (proximetacaine).
- 30 minutes before the start of irradiation, a solution of normotonic riboflavin (riboflavin 0.1% and dextran 20%) is instilled every 2 minutes and the saturation of the cornea with the solution is monitored by the degree of its staining using biomicroscopy.
- The skin of the eyelids and face around the eye within a radius of 5 cm is treated with betadine diluted with saline (1:1).
- For anesthesia, a 0.5% alcaine solution is instilled into the conjunctival cavity, 1-2 drops 2 times with a break of 1 minute.
- The surgical field area is covered with a sterile napkin with a slit for the eye.
- An eyelid speculum is placed on the eye.
- The eye cavity is washed with saline BSS solution.
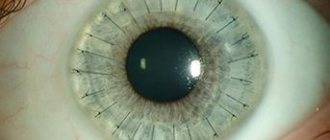
- In the optical zone, epithelium of a given diameter (8-9 mm) is mechanically removed, since it can prevent sufficient saturation of the stromal tissue with the riboflavin solution, as well as absorb part of the ultraviolet radiation necessary for the procedure.
- After which a solution of normotonic riboflavin (riboflavin 0.1% and dextran 20%) is installed, 1-2 drops every 2 minutes for 30 minutes (15 instillations).
- After 30 minutes, biomicroscopy is performed in blue light to identify the yellow color of the anterior chamber moisture and repeated pachymetry. When the thickness of the cornea without epithelium is less than 400 µm, a hypotonic solution of riboflavin is instilled to induce stromal edema (2 drops of solution every 10-15 seconds until the corneal thickness increases to more than 400 µm). Then the focusing of the radiation is adjusted (the distance between the emitter and the patient’s cornea is 5 cm), the diameter of the beam on the cornea (we avoid irradiating the limbus area) and the UV radiation is activated.
- At the same time, the installation of normotonic riboflavin continues (1-2 drops every 2 minutes).
- UV irradiation lasts 30 minutes, after which the cornea is washed with physiological BSS solution, an antibacterial drug (Vitabact 0.05%) is instilled and a soft contact lens is applied.
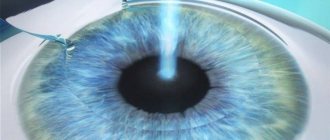
The following ultraviolet irradiation parameters are used: wavelength - 370 nm, radiation power - 3 mW/cm2 (5.4 J/cm2).
In the postoperative period, the patient is prescribed local antibacterial drops (chloramphenicol 0.25%) 4 times a day for 7 days, after complete epithelization of the cornea - anti-inflammatory drops (dexamethasone) 4 times a day for 7 days, as well as a drug to stimulate reparative processes (dexpanthenol) after removing SCL 2 times a day for 7 days + tear substitute without preservatives 3-4 times a day for 1 month.
Along with “superficial” saturation of the cornea with a photosensitizer (transepithelial cross-linking), there is an alternative method of forming a corneal “pocket” with a femtosecond laser for introducing riboflavin without scarification. The femtosecond laser has become actively used to form “tunnels” and “pockets” in the corneal stroma for the introduction of riboflavin. This approach allows you to shorten the postoperative period and is an effective method for treating progressive keratoconus.
A similar effect of increasing tissue resistance to collagenase biodegradation, as a result of the cross-linking procedure, is widely used in modern biotechnologies for the manufacture of various collagen-based implants.
To achieve stabilization of the pathological process by increasing the biomechanical properties of the cornea (CG and FRR), as well as significantly improving clinical and functional results, it is recommended to carry out combined treatment of keratoconus in the following sequence: the first stage is femtolaser implantation of the IRS, the second stage is cross-linking of corneal collagen.
Contraindications to cross-linking are a corneal thickness of less than 400 microns, a history of a herpetic infection, severe scarring or opacification, a low rate of epithelization, pathology of the immune system, pregnancy and breastfeeding.
Preparing for surgery
Before undergoing surgery, a person must adhere to the rules that will reduce the risk of complications and make the rehabilitation period easier:
- 2 weeks before surgery, you should not use medications that the ophthalmologist has not been warned about;
- 3 days before the procedure, start using antibacterial drops to eliminate the risk of infection entering the internal structures of the eyes when opening the cornea;
- do not wear contact lenses, replace them with glasses 2 weeks before the procedure;
- do not drink alcohol 2-3 days before surgery;
- on the day of surgery, you should not wear makeup, foreign particles will get into your eyes, causing irritation, inflammation, and the development of a bacterial infection;
- Before the operation, take a shower and thoroughly wash your face and hair.
If you prepare properly for surgery, the risk of bacterial infection and other complications will be significantly reduced.
Complications of crosslinking
In most cases, the prognosis for cross-linking is favorable. At the same time, like any invasive intervention, the procedure can have a number of complications. Possible complications include:
- temporary visual impairment (recovery of visual acuity is observed within 1 to 4 months after the procedure);
- reversible decrease in corneal transparency that does not affect visual acuity;
- slow (up to 1 month) restoration of the corneal epithelium;
- redness and irritation of the eyes, in rare cases - the development of keratitis;
- activation of herpetic infection with the development of herpetic lesions of the cornea.
Carrying out corneal crosslinking
The technique uses ultraviolet ray exposure together with riboflavin. This can be done after opening the cornea. The technique increases the risk of complications, especially in the presence of keratoconus. Relatively recently, a new technique for transepithelial cross-linking has been developed, which does not require an incision. Therefore, fewer complications arise.
Traditional crosslinking
The surgical intervention is carried out in several stages:
- The patient is prepared. He is put on sterile linen. He lies down on the couch, after which the eyes are instilled with an anesthetic.
- The surgeon removes the surface layers of the cornea with a spatula.
- The eyes are instilled with a solution of riboflavin. Then a slit lamp examination is performed. If there are no changes, the solution is instilled again. The cornea should be completely saturated. If this happens, proceed to the next stage.
- The exposed cornea is exposed to ultraviolet light, which forms a bond with the buried riboflavin. This forms cross-linking of corneal collagen. The tissues become thicker, they connect with each other.
- A solution containing an antibacterial agent and an anti-inflammatory drug is instilled into the patient's eyes.
- A soft support contact lens is inserted into the eyes and must be worn during the rehabilitation period.
The entire procedure can last up to 1 hour. This depends on the time it takes for the cornea to become saturated as a result of instilling riboflavin.
Transepithelial crosslinking
The difference between this procedure is the absence of mechanical removal of the top layer of the cornea. This significantly reduces the risk of tears in this layer. Instead of using a spatula, a special solution (tetracaine) is instilled into the patient's eyes, which helps loosen the tissue. After this, all steps of the procedure are repeated as in the previous method.
Stages of the procedure
Before the operation begins, the patient is given eye drops containing an anesthetic. After the onset of anesthesia, the doctor applies an eyelid speculum and, using an eye spatula, carefully removes the top layer of the corneal epithelium (this is necessary to improve the penetration of the vitamin B2 solution into the thickness of the cornea). Within 15–20 minutes, a riboflavin solution is instilled into the eye, at the same time the doctor examines the cornea using a slit lamp and evaluates how evenly the vitamin B2 solution penetrates the corneal tissue.
Upon reaching the required degree of saturation with the riboflavin solution, the corneal tissue is treated with low-intensity ultraviolet rays for 30 minutes, which avoids damage to the deeper structures of the eyeball. Under the influence of ultraviolet light, collagen fibers located in the cornea are welded together and form a strong frame that is resistant to stretching.
At the end of the procedure, antibacterial eye drops are instilled into the eye to prevent inflammation, after which the operated surface of the cornea is protected with a special therapeutic soft contact lens. Throughout the entire healing period of the cornea (an average of 3 - 5 days), the patient must wear a treatment lens and instill anti-inflammatory drops.
Rehabilitation and postoperative period
When the doctor has completed the procedure, the patient remains for 2-3 hours in the medical facility. During this time, the surgeon monitors the person’s condition; if there are no complications, he is discharged on the same day. After the surgery is completed, the patient must wear sunglasses to leave the clinic.
This significantly reduces the exposure of the eyes to ultraviolet rays from the sun.
After surgery, the patient must adhere to the rules for successful rehabilitation:
- wear bandage lenses for the time prescribed by your doctor;
- do not visit the bathhouse, sauna, or sunbathe, as this can cause bleeding inside the eyeball;
- do not use cosmetics for 1 week after surgery;
- reduce eye strain by reducing time spent watching TV, computer, phone, tablet, reading books;
- wear sunglasses when leaving home for the entire rehabilitation period;
- use all medications prescribed by an ophthalmologist;
- visit a doctor to monitor your vision at the appointed time;
- lack of physical activity and sports during the rehabilitation period.
Compliance with these rules will help to significantly reduce the risk of postoperative complications.
Rehabilitation period
Strict adherence to your doctor’s recommendations for eye care can prevent the development of complications and also reduce the recovery period.
- In the first days, pain and increased sensitivity to bright light may be observed in the area of the operated eye.
- Soft lenses can usually be removed after 3 days, and the outer layer of the cornea, damaged during surgery, regenerates by 5-6 days.
- Strictly follow the instructions for instilling drops: before removing the lenses, an antibiotic solution is dripped 4 times a day, anti-inflammatory drops are used according to a special scheme for 2 months.
- Protect your eyes as much as possible from bright light and dust, limit the load on the visual apparatus (computer, TV, reading).
- During the first month, swimming in any body of water (swimming pool, sea, river) is prohibited.
The rate of restoration of visual acuity is individual for each patient and can vary from a month to six months.
Complications
Some categories of patients may develop the following complications:
- hemorrhage on the cornea or inside the eyeball;
- decreased visual acuity temporarily or permanently;
- corneal clouding;
- decreased quality of twilight vision or its complete absence;
- color vision impairment;
- the appearance of foreign objects in front of the eyes that should not normally be there (dots, spots, lines, lightning, halo effect).
The risk of complications is reduced when choosing a qualified doctor and a medical facility equipped with modern equipment.
Patient reviews
Elena, 38 years old: When methods of vision restoration first appeared, I used the Lasik procedure. I developed a complication in the form of severe thinning of the cornea. The doctor said that I might lose my vision. After this, I performed corneal crosslinking. Now my condition is much better, the ophthalmologist said that I will retain my vision.
Vladimir, 28 years old: For many years now I have been suffering from severe thinning of the cornea. Drug treatment did not help me. The doctor said that surgery was not indicated. But recently a new technique has appeared - corneal cross-linking. The surgeon said that its thickness allows for the operation. After the operation, my condition improved significantly.