What is chorioretinitis
Any inflammation is based on the harmful activity of pathogenic microorganisms - bacteria, viruses. Microorganisms either penetrate into the cells of the body as a result of mechanical action, or their activity is a consequence of another disease.
Causes of chorioretinitis:
- infections;
- injuries;
- toxoplasmosis.
Focal ENT infections can cause inflammation of the visual organs: they are transmitted through the bloodstream.
Mechanical injuries to the visual apparatus are open doors for bacterial infection. Therefore, even with a minor injury, you need to contact an ophthalmologist for help. Toxoplasmosis is a dangerous infectious disease that is transmitted from a sick animal to humans. You can also get toxoplasmosis after eating poorly cooked meat. Sometimes toxoplasmosis is transmitted to the fetus from the mother through the placenta.
Classification
Classification according to etiology:
- infectious;
- allergic;
- systemic;
- post-traumatic;
- combined.
Infectious chorioretinitis of the eye is caused by the activity of microorganisms - fungi, viruses, bacteria. Allergic pathology occurs as a result of intolerance to any substance or ingredient. Systemic pathology develops against the background of internal diseases of a systemic nature. Post-traumatic pathology is a consequence of trauma to the visual apparatus. Combined chorioretinitis is a tandem of several causes.
Classification according to the localization of inflammation:
- central serous chorioretinitis;
- peripapillary;
- equatorial;
- peripheral.
Central chorioretinitis affects the macula - the yellow spot of the retina, peripapillary is located next to the optic nerve, equatorial - located around the circumference of the eyeball, peripheral is located next to the dentate line of the eye.
Classification according to the number of foci of inflammation:
- one area is focal;
- several areas - multifocal;
- several foci of inflammation are combined into one - diffuse.
Classification according to the nature of the course:
- active form;
- inactive;
- subactive.
The active form is characterized by deterioration in the quality of visualization and rapid eye fatigue. In the inactive form of the disease, there is a deterioration in the quality of visualization in the absence of symptoms of the inflammatory process; the pathology is detected during hardware diagnostics. The subactive form is detected during the diagnosis of other diseases, since it does not manifest itself in anything.
Chorioretinitis can also be acute or chronic. There are two ways of infection: endogenous and exogenous. The endogenous path - inflammation forms directly in the structure of the eye, the exogenous - passes from neighboring tissues.
The endogenous form of the pathology occurs due to mechanical injury to the eyeball, while the exogenous form is a consequence of systemic or autoimmune pathologies.
Central serous chorioretinitis
Central serous chorioretinitis leads to retinal separation. Blood plasma accumulates between it and the adjacent membranes of the eyeball. The pathology is caused by the fragility of the capillaries and their high permeability. Dangerously severe complications, requires treatment by an ophthalmologist. Self-treatment with folk remedies or pharmacy products is unacceptable. In chronic and subacute cases of the disease, laser surgery is required.
Toxoplasmosis
Toxoplasmosis chorioretinitis can appear with reduced immunity, and an infant can also become infected with it during the prenatal period of its development. With this form of the disease, the central nervous system, internal organs, and visual organs are affected. Retinal detachment, retinal hemorrhage, and the growth of additional capillaries may occur.
Tuberculous
Tuberculous chorioretinitis in its initial form proceeds completely unnoticed and is discovered randomly during an examination by an ophthalmologist. With secondary tuberculosis, the clinical picture changes and occurs with vivid symptoms. This pathology is dangerous due to serious complications: it leads to cataracts, damage to the optic nerve, and retinal detachment.
Syphilitic
The syphilitic form of the disease appears either in the prenatal period or in adulthood. The disease progresses brightly: hemorrhage occurs in the retina, atrophic changes in tissues form. If the pathology develops in adults, it is characterized by a diffuse form of changes.
Reasons for development
Central serous chorioretinitis can be provoked by exposure to a variety of factors:
- stress;
- changes in hormonal levels;
- vegetative dystonia;
- Cushing's syndrome;
- systemic lupus erythematosus;
- uncontrolled use of hormonal and other potent drugs;
- state after organ transplantation;
- pregnancy and childbirth;
- hereditary predisposition;
- arterial hypertension;
- hypersthenic type (large, dense) body type;
- severe allergies;
- age over 60 years;
- excessive physical activity.
Pathology can be triggered by frequent stress.
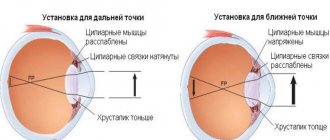
Often the cause of central chorioretinopathy cannot be determined. The mechanism of development of this disease is associated with impaired capillary permeability through the choroid. In this case, plasma from the bloodstream enters the tissue of the eyeball, causing swelling of the retina and its detachment. This process is caused by an imbalance between potassium and sodium ions. The pathology leads to significant impairment of visual function caused by insufficiency of the pigment layer of the eye.
Clinical picture
How does the disease manifest itself, what symptoms are characteristic of the pathology of the retina and choroid?
The symptoms are as follows:
- progressive decrease in visualization quality;
- the appearance of luminous figures and spots before the eyes;
- the appearance of “blind” areas in the field of view;
- distortion and change in the shape of familiar objects;
- increased intraocular pressure;
- retinal disinsertion;
- purulent inflammation of the inner membranes of the eyes;
- night blindness in the evening;
- vitreous hemorrhages;
- complete blindness.
Floating spots may appear before the eyes, and vision becomes clouded. During the daytime, patients do not complain of decreased visual acuity if the foci of inflammation are located in the periphery. But in the evening, the clarity of visualization noticeably decreases. The most common symptom of chorioretinitis is the appearance of spots before the eyes.
Most patients complain of the appearance of chorioretinitis after infectious and autoimmune diseases.
However, ophthalmologists are not always able to make the correct diagnosis, since a decrease in visual acuity with chorioretinitis does not occur immediately. The patient sounds the alarm only when “blind” spots appear in the field of vision.
Characteristic symptoms
Symptoms of chorioretinitis are divided depending on the area of localization of the disease. This:
- in the macular zone
- in the area around the optic nerve head
- near the equator
- near the dentate line
Inflammation may consist of a single focus, several lesions, or may be diffuse. The course of acute inflammation can last up to three months. Chronic diseases are often accompanied by relapse.
Peripheral chorioretinitis sometimes occurs without significant symptoms. Such diseases are more often detected during a medical examination. With disease in the central or macular region, blurring and loss of visual acuity are observed.
Sometimes dark spots or flashes appear. There is a distortion of the shape and size of objects. In some cases, “night blindness” occurs, in which it is difficult for a person to navigate during twilight.
Whatever the symptom of the disease, it indicates eye damage and is an urgent need to consult a doctor. Only a specialist can make a diagnosis.
Do you know who is affected by epicanthus and whether it needs to be removed?
What types of astigmatism are, the causes and methods of treatment can be found in this publication:
Diagnostics
To detect pathology, you need to conduct laboratory testing and instrumental diagnostics. The doctor must identify the causative agent of the inflammatory process and establish resistance to certain antibiotic drugs. Dependence on autoimmune diseases or its absence is also established.
Laboratory diagnostics implies:
- collection of conjunctival fluid to identify the causative agent of infection;
- enzyme immunoassay for virus detection;
- C-protein test.
To assess the extent of the lesion, an instrumental examination is performed. Visiometry allows you to determine visual acuity; intraocular pressure is also tested (to rule out glaucoma).
Specific diagnostics include:
- gonioscopy;
- ophthalmoscopy;
- FAH;
- OCT;
- perimetry
- tonometry;
- electroretinography.
Gonioscopy reveals the presence (absence) of purulent exudate in the anterior chamber of the eyeball. If hemorrhages occur in the anterior chamber of the eyeball, this results in hyphema.
Ophthalmoscopy reveals the presence/absence of pinpoint hemorrhages and pathologically altered areas of the eye.
FA (fluorescein angiography of the retina) allows you to determine the presence/absence of retinal vasculitis. OCT is a scan of the visual apparatus using a tomograph.
Perimetry allows you to determine the presence of concentric narrowing of the visual field in the presence of peripheral chorioretinitis.
Tonometry measures the level of intraocular pressure, since serious forms of the disease are characterized by an increase in IOP. Electroretinography allows you to analyze the condition of the retina, the degree of its functionality and health.
Differential diagnosis is carried out when a malignant neoplasm of the choroid of the eyeball is suspected and when there is a dystrophic change in the macula of the retina. The ophthalmologist must understand whether the narrowing of the visual field is caused by a malignant tumor or chorioretinitis. If there are no hemorrhages in the vitreous body, the pathology is associated with the retina and changes in the macula.
If the eye has been injured, the ophthalmologist prescribes x-rays, which determine internal damage to the bones of the orbit and the presence/absence of fragments of deformed bone tissue.
Laboratory blood tests are also prescribed for HIV, viruses, toxoplasma, and tuberculosis. If an active Koch bacillus is suspected, a chest x-ray is prescribed.
Approaches to the treatment of chorioretinitis
Treatment of acute chorioretinitis should be started immediately in order to stop the active process in time. First of all, medications should be used that are aimed at the immediate cause of the development of such inflammation, and secondly, treatment of symptoms to eliminate immediate complaints.
Due to the existence of a protective barrier in the structures of the eye, not all drugs administered through intramuscular and intravenous injections or in the form of tablets will reach the site of inflammation, therefore parabulbar injections and instillation of drops are considered the most effective way to deliver the necessary drug to the retina.
Treatment aimed at eliminating the cause
Even before determining the immediate cause of the development of chorioretinitis, antiviral agents or broad-spectrum antibacterial agents are prescribed, which are later adjusted if necessary.
When clarifying the diagnosis.
- Syphilis - antibiotics of the penicillin series or macrolides, cephalosporins of the latest generations are prescribed.
- Herpes viral chorioretinitis - Acyclovir at the maximum dosage for 5 days, then the dose is gradually reduced by the attending physician. Since it is almost always accompanied by changes in the corneal epithelium (epithelopathy), the use of protective gels (Korneregel, Solcoseryl) is recommended.
- Toxoplasmosis - therapy is supplemented with specific drugs prescribed by an infectious disease specialist, with the addition of B vitamins.
- Tuberculous chorioretinitis is treated together with phthisiatricians.
Medicines for symptomatic treatment
To relieve signs of inflammation - pain, swelling, infiltration into the vitreous body, anti-inflammatory therapy is used, including glucocorticoids and non-hormonal agents. Dexamethasone is used most often in the form of parabulbar injections, sometimes replacing it with a long-acting glucocorticoid - Diprospan.
In order to eliminate signs of intoxication, intravenous infusions, including 5% glucose, and hyposensitizing drugs are added to therapy.
Vitamins and enzymes
Local immunity against the background of inflammation of the eye membranes is impaired, therefore, depending on the severity and type of process, immunomodulators are prescribed. In addition, multivitamins and antioxidants help stimulate the proper functioning of the immune system.
Photo: https://pixabay.com/illustrations/syringe-pill-capsule-morphine-1884784/
To resolve hemorrhages and foci of infiltration in the vitreous body, enzyme preparations are used in the form of parabulbar injections and physiotherapy. The most commonly used enzymes in ophthalmology are fibrinolysin, hemase, histochrome, lidase.
Surgical approach
Surgical treatment methods are used to prevent complications and to eliminate the consequences of previous chorioretinitis. Laser coagulation of the retina is carried out to delimit the pathological process in a certain area and prevent its spread to adjacent areas.
In case of a severe process, accompanied by proliferation into the vitreous body and with the threat of developing retinal detachment, the vitreous body is removed - vitrectomy.
Traditional methods
Some sources indicate traditional medicine, in particular, valerian root, hawthorn, hazel bark, which must be consumed orally with a certain brewing method.
I would like to remind you that due to the specific vascular barrier, most substances from the blood cannot enter the eyeball and affect the source of inflammation, therefore the use of these drugs for the treatment of chorioretinitis directly is inappropriate. But to strengthen general immunity, some traditional medicine can actually be used.
Conservative therapy
Treatment of chorioretinitis is carried out after a detailed diagnosis, based on its data. The therapeutic regimen depends on the patient’s condition, his clinical picture, and the presence/absence of serious internal diseases of a systemic or autoimmune nature.
Conservative treatment involves:
- the use of ophthalmic drops that eliminate the inflammatory process;
- individually selected set of antibiotics;
- the use of mydriotic drugs to control intraocular pressure;
- biogenic stimulants, reparants for activation of regenerative processes in the choroid and retina;
- hormonal medications for acute pathology.
For the syphilitic form, Doxycycline, Erythromycin, and Penicillin are prescribed. To cure toxoplasmosis chorioretinitis, Pyrimethamine or Sulfadimezine is prescribed. For tuberculosis, hormones and chemical medications are prescribed. The viral form is treated with antiviral medications and immunomodulators are prescribed.
To accelerate cell regeneration, enzymatic agents are prescribed: Fibrinolysin, Lidaza.
For acute chorioretinitis, medications with hydrocortisone are prescribed. To speed up tissue healing, ultrasound therapy and physiotherapy are prescribed.
If the eye has been injured by external mechanical force, surgical correction is performed. Perhaps the patient needs bone grafting, which involves joining the fragments of the orbit.
In case of severe clouding of the ocular media, the vitreous body is removed. Laser coagulation of the retina is also prescribed to prevent the formation of complications. At the stage of active healing of the tissues of the visual apparatus, ultrasound treatment is prescribed.
Forecast
How optimistic is the prognosis for healing? The earlier treatment is undertaken, the more optimistic the prognosis. In the old form, scars form that cannot be reabsorbed. This disease can pass without a trace, or can lead to complete blindness.
The prognosis is determined not only by timely seeking medical help and taking medications - much depends on the person’s immune status, age, lifestyle, and the presence/absence of bad habits.
Prevention and prognosis
You can prevent the development of chorioretinitis by following simple recommendations. If the image begins to distort, your eyes hurt, you need to urgently contact an ophthalmologist. We must not forget about visual hygiene. It is necessary to eliminate infections that lead to inflammation in the choroid.
In case of incorrect or delayed therapy:
- The retina detaches.
- Hemorrhages occur.
- Atrophied lesions appear.
- Vascular thrombosis develops.
During treatment it is recommended to drink plenty of fluids
Any type of chorioretinitis is difficult to treat, and it is especially difficult to cope with chronic pathology. Remissions are replaced by new exacerbations, foci of inflammation often appear in the same places.
The disease is not fatal to a person, but it complicates his life and leads not only to decreased vision, but if left untreated, to blindness. We also recommend that you read our article which will tell you what scotoma of the eye is.
Folk remedies
The use of tinctures and decoctions can speed up the healing process. It is recommended to use vasodilators and vitamins. This will complement the conservative course of treatment, but will not replace it.
An infusion of hazel bark is a vasodilator. The crushed bark is steamed with boiling water, wrapped and allowed to rest for about an hour. 10 g of crushed bark is consumed per glass of water. The product is taken orally in a teaspoon several times a day.
To strengthen the immune status, take vitamins. Riboflavin, folic acid, and retinol have a good effect. You need to eat fresh vegetables and fruits: squeeze juice out of them, stew them. If the pharmacy does not have riboflavin, it can be found in fermented milk products.
Prevention is regular examination by an ophthalmologist, timely treatment of ENT diseases and elimination of infection.
Bottom line
Chorioretinitis is a dangerous inflammatory ophthalmological disease of the posterior part of the eyeball, which can lead to complete loss of visual ability. The pathology is characterized by the formation of foci of inflammation of the choroid (choroid) and retina (retina).
Symptoms of the pathology are “blind” spots in the field of vision, flickering of dark or luminous dots before the eyes, flashes of light, distortion of the shape of familiar objects. However, more often it is asymptomatic and discovered by chance at a preventive appointment with an ophthalmologist.
Chorioretinitis can appear for various reasons: as an allergy to substances, as a result of trauma to the visual apparatus with tissue rupture, or as an infection.
Hormones, antibiotics, and anti-inflammatory drugs are used in treatment: the therapeutic regimen depends on the characteristics of the disease. An integrated approach to treatment consists of using antibiotics, placing ointment in the conjunctival sac, administering medications behind the eyeball, and administering antiviral injections intramuscularly.
Sources used:
- Morphological foundations of ophthalmoscopic diagnostics / V.N. Arkhangelsk. - M.
- Eye diseases. For general practitioners. Reference manual / Yu.S. Astakhov, G.V. Angelopulo, O.A. Jaliashvili. - M.: SpetsLit, 2004.
- Physiology and pathology of the retina: Primary mechanisms of vision / G.G. Demirchoglian. - M.
- Shaikh S, Trese MT (2004). "West Nile virus chorioretinitis." Br J Ophthalmol.