Uveitis is an inflammation of the uveal tract, the choroid of the eye. In ICD 10 (International Classification of Diseases, 10th revision) it is coded H30-H36. The disease is not common: it affects only 0.1-0.2% of people. But it is precisely this that becomes a common cause of low vision and blindness. Let's find out what the types and symptoms of the disease are, why it occurs, and how to treat it correctly.
Uveitis is an inflammation of various parts of the choroid of the eye.
Types and causes of uveitis
Based on the reasons that caused it, uveitis is divided into:
- Infectious (viral, bacterial, fungal, parasitic).
- Non-infectious (allergic or caused by systemic diseases).
Attention! Systemic diseases are pathological conditions in which the functioning of entire body systems, rather than just one organ, is disrupted.
An infectious disease is contagious. Adenoviral uveitis is transmitted by airborne droplets, herpetic uveitis by contact, and enteroviral uveitis by fecal-oral route. You can become infected with the toxoplasmosis form from infected pets and by consuming foods that have not undergone sufficient heat treatment. In fungal and bacterial types of disease, the main route of transmission is contact.
Domestic animals are carriers of the toxoplasmosis form of the disease.
Uveitis is usually caused by endogenous (internal) causes. It develops against the background of pre-existing inflammatory diseases. It can be caused by: tuberculosis infection, ear, nose and throat diseases. In such cases, pathogens are transferred to the eyes through the blood.
There is also autoimmune uveitis, which is not contagious to others. The following diseases can cause it:
- psoriasis;
- sarcoidosis;
- Crohn's disease;
- Bekhterev's disease;
- juvenile rheumatoid arthritis;
- nonspecific ulcerative colitis.
Ophthalmologist Elena Stanislavovna Prokhvachova says:
“The usual cause of uveitis is an infection or a systemic disease of the body. In most cases, the patient himself does not pose a threat to others. It is easy to get infected from it only with tuberculosis. In other cases, this is only possible with very close contact with the patient, who does not follow the rules of personal hygiene.”
Poor hand hygiene is one of the causes of infection.
The disease happens:
- sluggish - with mild symptoms;
- with vivid symptoms - it begins as quickly as it ends.
If uveitis lasts less than three months, then it is called limited, if longer - persistent.
Depending on the nature of the course, the disease can be of the following types:
- Spicy. Begins abruptly, duration is limited.
- Recurrent. Sudden exacerbations are followed by remissions that last longer than three months without treatment.
- Chronic. Persistent acute periods are replaced by short remissions (up to three months without treatment).
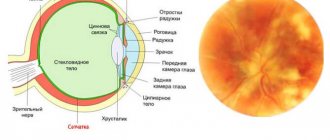
Based on the location of inflammation, uveitis is classified into:
- anterior (iritis - inflammation of the iris);
Symptoms of iritis include red eyes, watery eyes, pain, and mild blurred vision.
- posterior (choroiditis - the choroid is inflamed - the back part of the choroid, which nourishes the retina);
- peripheral (cyclitis - the ciliary body is affected - the middle part of the uveal tract, to which the lens is suspended).
Sometimes the disease affects not only the uveal tract, but also adjacent tissues. Then the following are possible: iridocyclitis (inflamed iris and ciliary body), chorioretinitis (choroid and retina) and neuroretinitis (optic nerve and retina). If the inflammation has spread to the entire choroid, then they speak of the development of panuveitis.
Causes
This disease can be caused by various reasons, the main ones are the following:
- Infections – uveitis of an infectious nature occurs in 45% of cases. The causative agents of the inflammatory process are most often streptococci, toxoplasma, mycobacterium tuberculosis, cytomegalovirus, treponema pallidum, and fungi. Infectious agents penetrate the vascular bed from any source of infection, usually with tuberculosis, sepsis, tonsillitis, syphilis, influenza and even dental caries.
- Allergic reaction - can cause inflammation of the choroid with the development of allergies to medications and food, hay fever, the introduction of potent serums and vaccines.
- Systemic diseases - rheumatism, spondyloarthritis, multiple sclerosis, psoriasis, Reiter's syndrome, sarcoidosis, glomerulonephritis, Vogt-Koyanagi-Harada syndrome, etc.
- Eye injuries - burns, punctures, eye cuts, foreign body getting into the eye.
- Hormonal disorders - diabetes, menopause, blood diseases, etc.
- Eye diseases – keratitis, blepharitis, conjunctivitis, retinal detachment, scleritis, etc.
Diagnostics
When the first symptoms of uveitis appear in the form of pain in the eyes, redness, and decreased visual acuity, you should consult an ophthalmologist. The doctor will first conduct an external examination of the eyes (pay attention to the condition of the skin of the eyelids, pupils, conjunctiva), visometry (determining visual acuity), perimetry (examination of visual fields). Intraocular pressure should also be measured.
Additionally, to diagnose uveitis, the following studies are performed: biomicroscopy, gonioscopy, ophthalmoscopy, ultrasound of the eye, angiography of retinal vessels. To clarify the diagnosis, rheoophthalmography, electroretinography, and optical coherence tomography are sometimes performed. To identify the underlying disease that caused uveitis, a consultation is held with an allergist, endocrinologist, and infectious disease specialist with all the necessary tests.
Differential diagnosis is carried out with the following diseases:
- Anterior uveitis - with keratitis, scleritis, conjunctivitis, episcleritis, acute attack of glaucoma.
- Posterior uveitis – with tumors of the choroid, the initial phase of retinal detachment.
Complications
Due to deposits of lens masses, visual acuity decreases up to complete blindness. The sooner treatment is started, the greater the chance of stopping the process of vision loss. As a result of posterior synechiae (adhesions) of the iris, intraocular pressure increases and angle-closure glaucoma develops. Other complications of inflammation of the choroid are cataracts, vasculitis, papilledema, and retinal detachment.
Symptoms of the disease
Signs of anterior uveitis:
- photophobia;
- lacrimation;
- constricted pupils;
- Pain in the eyes;
- hyperemia of the sclera;
- increased intraocular pressure.
Symptoms of peripheral uveitis:
- blurred vision;
One of the symptoms of the peripheral form of the disease is spots before the eyes.
- points before the eyes.
In the posterior form of the disease, patients complain only of blurred vision, and later of dull pain in the eyes. With panuveitis, signs of all types of uveitis are observed.
Symptoms of uveitis
The clinical picture of ophthalmovascular inflammation is determined by a number of conditions: the nature of the pathogenic factor, the localization of the primary lesion, the speed and intensity of development. Accordingly, the symptoms of uveitis are very diverse.
Thus, more or less typical manifestations of anterior uveitis are subjective sensations of “veil before the eyes” and heaviness in the eyeball; decreased visual acuity and clarity; noticeable redness of the sclera; aching, “pulling” or sharp pain; miosis (constriction of the pupil) with weakened or absent response to light, or, on the contrary, a painful reaction of the eye to bright light; hyperlacrimation (increased lacrimation); surge in IOP (intraocular pressure). The extreme, limiting symptom of uveitis in some cases is complete loss of vision.
Posterior uveitis (choroiditis) is dangerous due to a long period of asymptomatic development, when there are neither visible signs nor subjective painful sensations. A decrease in visual acuity and quality also develops, as a rule, too slowly and gradually for the patient to notice it in the early stages. Seeking help is usually due to obvious “fogging” or the appearance of scotomas (blind spots) in the field of vision.
Diagnostics
In ophthalmology, two methods are used to diagnose uveitis:
- Biomicroscopy of the eye (for iritis and iridocyclitis). The doctor examines the anterior structures of the eyeball under magnification using a slit lamp.
The process of eye biomicroscopy does not cause pain; the patient only observes the beam of light.
- Ophthalmoscopy (for cyclitis, choroiditis and chorioretinitis and neuroretinitis). An ophthalmologist examines the condition of the fundus of the eye using an ophthalmoscope, which provides magnification from 2 to 15 times.
Additionally, the patient may be prescribed general tests, x-rays, ultrasound examinations and other diagnostic procedures to identify systemic diseases that could cause the development of uveitis.
First aid to a patient
No measures can be taken without establishing the nature of the disease, since all its types are treated differently. An exception is anterior uveitis (iritis, iridocyclitis), which can lead to fusion of the edges of the iris with the lens or their complete soldering. First aid in this case is to prescribe drugs from the mydriatic group:
- Mydriacyl;
- Midrimax;
In the initial forms of the disease, the doctor may prescribe Midrimax.
- Irifrit;
- Visofrine;
- Tropicamide;
- Cyclomed.
By dilating the pupil, they will prevent it from completely overgrowing, which will allow the patient to maintain visual ability. An additional effect is a decrease in intraocular pressure.
Classification of pathology
There are several classifications of this disease.
Depending on the location of the inflamed area:
- damage to the anterior section (anterior uveitis, which includes iritis, iridocyclitis);
- inflammation of the posterior parts of the choroid (posterior uveitis - choroiditis, chorioretinitis);
- intermediate – damage to the peripheral parts of the choroid, which are located on the surface of the retina;
- diffuse - in this type, the pathology covers the entire choroid.
Classification according to the etiology of the disease:
- Exogenous causes, in which the infectious agent enters the internal environment of the eye from the outside. This is typical for post-traumatic inflammation.
- Endogenous uveitis is caused by internal microbes that affect the choroid against the background of decreased immunity. Various microorganisms enter the eye through the bloodstream from foci of chronic infection. Also, the inflammatory process can be initiated by the inclusion of autoimmune mechanisms.
According to the course of the disease:
- acute (up to 1.5 months);
- subacute (up to 6 months from the onset of the disease);
- chronic (with frequent or rare relapses, especially in the cold season).
The process is also divided depending on the nature and severity of inflammatory phenomena into:
- serous;
- purulent;
- fibrinous;
- hemorrhagic;
- mixed.
Treatment methods
For uveitis , symptomatic treatment is carried out aimed at reducing the manifestations of the disease. For this, ophthalmologists prescribe the following medications:
- Drugs from the NSAID group to combat mild to moderate inflammation. The drugs can be taken both topically - in the form of eye drops (Diclofenac, Indocollir) and systemically - in the form of tablets (Ibuprofen, Naproxen, Ketoprofen). An additional effect is pain relief.
Indocollir fights ophthalmic inflammation and relieves pain.
- Glucocorticosteroids in the form of eye drops (Dexamethasone) or ointment (Hydrocortisone ointment 0.5%). They reduce inflammation in uveitis of an allergic or unknown nature, and prevent the iris from welding together.
- Antihistamines for allergic forms of the disease. Eye drops - Opantanol, Allegordil, Lecrolin. Inside - Suprastin, Tavegil, Claritin, Xizal.
- Antiviral drugs. Oftalmoferon drops (for adenovirus infection). Ointments Acyclovir, Zovirax (for herpetic eye lesions). Sometimes antiviral drugs are prescribed orally - Acyclovir, Cycloferon tablets, Arbidol capsules.
- Antibiotics for bacterial uveitis. In the form of drops: Tobrex, Tsipromed, Tsiprolet, Levomycetin. In the form of ointment: Tetracycline, Erythromycin. Inside: Amoxicillin, Ciprofloxacin, Gentamicin. It is possible to administer antibacterial drugs intramuscularly or under the conjunctiva.
For bacterial etiology of uveitis, antibiotics are prescribed, for example, Tobrex.
- Combined eye drops and ointments with glucocorticosteroids and antibiotics: Tobradex (tobramycin, dexamethasone), Sofradex (gramicidin, framycetin and dexamethasone).
- Mydriatics (Midriacyl, Midrium) for the prevention of adhesions and elimination of spasm of the ciliary muscles of the iris, which causes pain to the patient.
For uveitis, surgery is sometimes indicated. Usually prescribed:
- vitrectomy;
- phacoemulsification;
- injections under the conjunctiva;
The injections stop the inflammatory response.
- filtering glaucoma surgery.
Patients may be prescribed a biopsy to clarify the diagnosis or surgery to remove pathological structures for cataracts, retinal detachment or vitreous destruction.
Attention! If the cause of the disease (possible systemic diseases) is not treated, uveitis will first become recurrent and then chronic. Then the treatment will be long and ineffective.
Egor from Murmansk writes:
“I have uveitis. The ophthalmologist said that it was caused by some disease that needed to be identified and treated. I saw an infectious disease specialist, an immunologist, an endocrinologist and a rheumatologist. Tests show an inflammatory process in the body, but no one can find anything. The doctor said that this happens in half of the cases. And I will have to limit myself to symptomatic treatment only.”
What is uveitis?
Approximately 30-60% of cases of inflammatory processes in the eyes are due to uveitis. The pathology took its name from the uveal membrane of the eyes, where the vessels are located. This area consists of the ciliary body, choroid, and retina. Accordingly, uveitis is divided into iridocyclitis, cyclitis, iritis, choroiditis, chorioretinitis and so on. A third of cases lead to either blindness or impaired vision.
This prevalence of uveitis is primarily associated with the branching of the vascular system in the eye, as well as with a slowdown in blood flow in the uveal membrane. This feature primarily contributes to the retention of pathogens in the membranes of blood vessels, which often provoke this disease.
Another feature of the functioning of the vascular system of the eye is the separate supply of blood to the anterior and posterior parts of the uveal membrane. Because of this structure, damage to the departments occurs separately, although there were precedents for the simultaneous development of pathology.
Important! Uveitis symptoms are similar to a number of other eye pathologies, both infectious and non-infectious types. It is important to determine the cause and type of treatment so that complications such as cataracts, glaucoma or pterygium of the eye do not develop.
They also have different innervation, which is present in the ciliary body and retina, but is absent in the choroid. Such structural features of the eye and its vascular system in individual parts, as a result of the influence of various factors, provoke the development of the disease.
Complications and consequences
Missing or incorrect treatment of the disease is fraught with the following consequences:
- development of cataracts;
- development of glaucoma;
- fusion of the pupil;
- vitreous opacification;
- damage to the optic nerve;
- the appearance of pathological vessels in the retina and its detachment;
- fusion of the iris with the lens (the diameter of the pupil remains fixed, and it cannot increase in the dark or decrease in the light).
A complication after uveitis is cataract.
10% of people who have lost their sight have become blind as a result of uveitis, which also causes low vision in 15% of cases.
Prognosis and prevention
With comprehensive and complete treatment in the initial stages of uveitis, recovery occurs after 4-6 weeks. Chronic uveitis can recur if the underlying disease worsens. a complicated course leads to the development of various pathologies and complications such as:
- Glaucoma;
- Sinechy;
- Retinal detachment;
- Retinal infarction;
- Retinal dystrophy;
- Optical disc edema;
- Cataracts.
Important! The development of complications increases in the absence of treatment. Moreover, the longer the disease lasts without proper therapy, the greater the chance of losing visual function without its restoration.
As a result, vision deteriorates significantly or disappears completely, often irreversibly even with the use of surgical methods. Therefore, it is important to carry out proper prevention. Its rules are simple:
- It is necessary to carry out preventive examinations in a timely manner;
- Treat existing pathologies in a timely manner;
- Avoid eye injuries;
- Timely treatment of ophthalmological pathologies;
- Eliminate allergies by taking the appropriate type of medication.
Such prevention allows you to solve several problems at once, maintain health and prevent the development of this pathology. If the disease is chronic, it is worth visiting a doctor regularly. It is also necessary to visit other specialized specialists who will help cope with general systemic diseases.
Sources used:
- Uveitis. Guide for doctors: monograph. / Panova Irina Evgenievna. - M.: Medical Information Agency (MIA), 2014.
- Uveitis / N.Ya. Senchenko, A.G. Shchuko, V.V. Malyshev. - M.: GEOTAR-Media, 2014.
- Uveoscleral outflow and treatment of glaucoma / Grigory Stolyarov. - M.: LAP Lambert Academic Publishing, 2014.
- Wikipedia article
Features of the course and treatment of uveitis in children
Unlike adults, diagnosing the disease in children is very difficult. In them, it develops gradually without the appearance of obvious symptoms. A sick child usually complains of worsening vision: it becomes foggy. There is no pain. With iritis and iridocyclitis, the anterior structures of the eye become filled with blood, causing the sclera to appear red. There are no other signs.
Parents who complain of deteriorating vision suspect the development of myopia. They begin to limit the time the child spends on the computer and TV, and monitor how he writes and reads. They may insist on doing eye exercises. But this is the main mistake, because without treatment, uveitis causes retinal detachment within a few months.
Attention! The first step parents should take if their child says they have trouble seeing is to take them to an ophthalmologist.
He will see the problem after checking his vision using the Sivtsev table. With myopia, children see the top lines, and with uveitis, all letters will be blurred. Then the doctor will conduct additional diagnostics.
Only a doctor can diagnose a child.
Treatment of inflammation of the choroid in children is no different. They are also given local and systemic therapy, and in severe cases, surgery. A thorough examination of the body is recommended to detect indolent infections and other hidden diseases that could cause uveitis.
Daria from Saratov writes:
“I have been suffering from tuberculous uveitis since I was 7 years old. For 5 years, she underwent 2 courses of drug therapy per year. Now I’m 24 years old, there are no relapses, but I constantly use drops. Cataracts and glaucoma have developed, the pupil is fused with the lens, and with my right eye I can only see silhouettes. They offer me surgery. I'm at a loss".
Treatment
The following specific antiviral drugs are used in the treatment of patients with viral uveitis: acyclovir (Virolex, Zovirax, Medovir), valacyclovir (Valtrex), ganciclovir (Cymevene), bonaftone.
Acyclovir (Virolex, Zovirax, Medovir)
- an antiviral drug, has activity against viruses: herpes simplex types 1 and 2, herpes zoster, Epstein-Barr and cytomegalovirus, suppresses their reproduction, slowing down the synthesis of viral DNA. For infections caused by herpes simplex, acyclovir is prescribed orally at a dose of 200 mg 5 times a day for an average of 5 days. For prevention - 200 mg 4 times or 400 mg 2 times a day for a long time with periodic breaks of 6-12 months. For herpes zoster, acyclovir is prescribed 800 mg 5 times a day for 7 days.
In case of severe infection, acyclovir is prescribed intravenously (infusion duration of at least 60 minutes) at a dose of 5-10 mg/kg every 8 hours (up to 30 mg/kg per day) for 7-11 days. Side effects include the possible development of intestinal colic, fever, and headache. Alopecia and neurological disorders (hallucinations, agitation, psychosis) are rarely observed. Blood tests revealed a transient increase in the levels of bilirubin, liver enzymes, urea and creatinine. The drug is used with extreme caution in patients with impaired liver and kidney function.
In patients with acute retinal necrosis syndrome in the acute stages of the disease, acyclovir is prescribed not only systemically, but also injected into the eye cavity (10-40 mcg/ml) during vitrectomy. It has been experimentally established that acyclovir at a dose of 40 mcg/ml is non-toxic to the retina.
Valacyclovir (Valtrex)
- in the human body it is converted into L-valine and acyclovir, which blocks the synthesis of viral DNA and the replication of viruses. The drug is in vitro active against viruses: herpes simplex types 1 and 2, herpes zoster, Epstein-Barr, cytomegalovirus and herpes virus type 6.
To treat an infection caused by herpes simplex, Valtrex is prescribed orally at a dose of 500 mg 2 times a day, the duration of therapy is 5 days, in severe cases - 10 days. For herpes zoster, 1 g is prescribed 3 times a day for 7 days. The following side effects are known to develop: renal failure in patients receiving Valtrex for a long time at a dose of 8 g per day; microangiopathic hemolytic anemia; thrombocytopenia.
In case of overdose of the drug, acyclovir can be removed using hemodialysis.
Acyclovir showed no signs of interaction with other drugs.
Ganciclovir (cymevene)
- inhibits viral DNA synthesis. In patients with cytomegalovirus retinitis, histological examination of the retina shows a virusostatic effect, but the virus is not completely removed from the retina; when you stop taking ganciclovir, an exacerbation of the process may be observed.
The drug is active against cytomegalovirus, herpes simplex types 1 and 2, herpes zoster, Epstein-Barr virus. In vitro studies have found that ganciclovir is 10-100 times more active than acyclovir against various laboratory and clinical isolates of cytomegalovirus. The drug is very toxic, it should be used only for retinitis of cytomegalovirus etiology (with laboratory confirmation of the diagnosis), and if the expected positive effect outweighs the risk of side effects and complications.
When administered intravenously, ganciclovir is prescribed at a rate of 5 mg/kg every 12 hours (daily dose 10 mg/kg), with a treatment duration of 14-21 days. Long-term maintenance therapy with ganciclovir is carried out at a rate of 6 mg/kg per day 5 days a week, or 5 mg/kg per day daily. Maintenance treatment is carried out mainly in patients with immunodeficiencies and the risk of relapse of cytomegalovirus retinitis.
Cymevene capsules can also be used for maintenance therapy. The drug is always prescribed during meals, 1 g orally 3 times a day or 500 mg 6 times a day.
Other methods of prescribing ganciclovir in the treatment of cytomegalovirus retinitis are also possible.
So Orellana J. et al. (1987) proposed administering the drug intravenously at a dose of 2.5 mg/kg every 8 hours for 21 days, followed by long-term maintenance therapy of 5 mg/kg per day. Holland G. et al. (1987) used ganciclovir at an initial dose of 5-14 mg/kg per day for a duration of treatment of 9-26 days. Maintenance treatment was carried out using the drug in small doses (1.5-7.5 mg/kg per day). Patients received the drug daily or every other day.
Ganciclovir is an effective treatment for cytomegalovirus infection, but it must be used long-term. Exacerbation of the process during treatment can be stopped by increasing the dose of the drug.
With long-term use of ganciclovir, the concentration of creatinine in the blood or its clearance should be determined every two weeks. Among the side effects, it is necessary to note: neutropenia, thrombocytopenia, anemia, less often - eosinophilia; arrhythmia, arterial hypertension; paresthesia, psychosis, seizures; gastrointestinal bleeding; increased levels of creatinine and urea in blood plasma; hypoglycemia; Phlebitis may develop at the injection site. In high doses, ganciclovir suppresses spermatogenesis and fertility.
Experimental studies have established that cymevene has mutagenic and carcinogenic effects.
The basis for the intravitreal use of ganciclovir was experimental data that showed that when administered intravitreally at a dose of up to 30 mg/ml, the drug does not have a toxic effect on the retina. This was confirmed by electrophysiological and histological studies of the retina.
Henry (1987) first reported the intravitreal use of ganciclovir at a dose of 200 mcg for cytomegalovirus retinitis. Moreover, the concentration of the drug in the vitreous remained at the original level for 62 hours after injection. To stabilize cytomegalovirus retinitis, it is sufficient to use ganciclovir at a maintenance intravitreal dose of 200 mcg per week, however, Harris M. et al. (1989) indicated that long-term (15 weeks) intravitreal treatment with ganciclovir can lead to the development of endophthalmitis.
Heery S. et al. (1989) administered ganciclovir intravitreally (under local anesthesia) at a dose of 2 mg in 0.1 ml. The treatment was well tolerated, there were no signs of retinal toxicity, the only complication was moderate vitreous opacification.
The advantage of this method of treatment lies not only in achieving a higher concentration of the drug in the immediate vicinity of the affected area, but also in the absence of significant adverse reactions from other systems and organs. Intravitreal administration of ganciclovir can be used when systemic use of the drug is limited by adverse reactions.
Foscarnet (trisodium phosphonoformate)
- an antiviral drug blocks viral DNA polymerase, has activity against herpes viruses type 1 and 2, varicella zoster, oncogenic viruses, influenza A and hepatitis B viruses, some retroviruses, as well as cytomegalovirus.
P. Lehoang et al. (1989) used foscarnet for the treatment of cytomegalovirus retinitis. After a 3-week introductory course of therapy, maintenance treatment with the drug was carried out in small doses. In all patients who did not receive maintenance therapy, a relapse of retinitis was noted within 3 weeks after stopping the course of treatment with foscarnet. During maintenance therapy, the relapse rate during the first 5 weeks of treatment was 50%.
Unlike ganciclovir, foscarnet does not cause neutropenia, but has a toxic effect on the kidneys (probably the development of irreversible renal failure).
Foscarnet has poor tissue permeability, which prevents the manifestation of its therapeutic effect in deep infectious eye lesions. In this regard, it is advisable to administer the drug intravitreally. The results of experimental studies show that intravitreal administration of foscarnet at a dose of 20-1000 mcg in 0.1 ml is non-toxic to the retina.
Bonafton
- a domestic antiherpetic drug, prescribed 1 hour after meals, 0.1 g 2-4 times a day for 14-20 days.
If the virus reaches a latent state, then chemotherapeutic agents become ineffective in removing the virus from the host. In this case, it is advisable to carry out only preventive treatment. However, with long-term preventive courses, the development of viral resistance to antiviral drugs, in particular to acyclovir, has been described.
Specific antiviral therapy should be carried out against the background of local and possibly systemic administration of corticosteroids, especially in patients with acute retinal necrosis syndrome.
Of particular interest in the treatment of uveitis of herpetic etiology is the use of interferon inducers (poludan, prodigiosan).
Poludan
- biosynthetic interferonogen, has an inhibitory effect on the herpes simplex virus, which has been proven in experimental models and in the clinic (A.A. Kasparov et al., 1972, 1973; N.S. Zaitseva et al., 1973). Poludan at a dose of 200 mcg stimulates the production of at least 100 IU of interferon in 1 ml of culture fluid.
With herpesvirus infection of the posterior part of the eye A.A. Kasparov (1994) recommends administering the drug retrobulbarly, 0.5 ml (100 IU), for a course of 10-20 injections.
For isolated iridocyclitis caused by the herpes simplex virus, A.A. Kasparov (1973, 1994) injected poludan into the anterior chamber of the eye. According to the same author, intraocular use of the drug is contraindicated for conjunctivitis, infections of the teeth and paranasal sinuses.
Poludan is administered in an operating room, under the control of an operating microscope, after preliminary akinesia of the eyelids, installation and retrobulbar anesthesia.
A.A. Kasparov (1994) recommends two options for administering the drug.
First option
At 1 mm from the limbus, a paracentesis is performed with the tip of the blade, through which a thin needle for subconjunctival injections, connected to a syringe or to an aspiration-irrigation system, is inserted into the cavity of the anterior chamber.
First, the moisture of the anterior chamber is sucked out in a volume of 0.1-0.3 ml, followed by fractional administration of a solution of poludanum, which is prepared ex temporae. To do this, the contents of the ampoule are dissolved in 0.6-0.8 ml of water for injection. The total volume of administered poludanum is 0.4-0.6 ml. At the moment of needle insertion, a pre-applied suture (9/0-10/0 nylon) is tied, sealing the anterior chamber of the eye. An antibiotic solution is injected under the conjunctiva.
Second option
A 5 mm long conjunctival incision is made 5 mm from the limbus in one of the sectors located between the rectus muscles, after which a scleral paracentesis is made 3-4 mm from the limbus.
A blunt-ended curved cannula is inserted into the anterior chamber of the eye through a 1 mm incision in the sclera with slow movements, the intraocular fluid is sucked out, followed by the introduction of a solution of Poludanum in a volume of 0.3-0.5 ml. At the time of removal of the cannula, a previously applied suture is tied to the edges of the scleral incision (nylon 9/0-10/0) and another 0.1-0.2 ml of Poludanum solution is injected. With this option of intraocular infusion of Poludanum, not only the introduction of the drug into the anterior chamber is achieved, but also a small depot is created and the ciliary body is irrigated with Poludanum solution. 2-3 sutures are placed on the conjunctiva, and an antibiotic solution is injected under the conjunctiva.
The course of treatment is from 1 to 3 injections with an interval of 3-4 days. Subsequently, it is possible to switch to subconjunctival injections of the drug. When introducing Poludanum into the anterior chamber, in rare cases, the next day there may be an increase in intraocular pressure, the appearance of hemorrhage in the anterior chamber, and increased tyndalization of the moisture of the anterior chamber. These phenomena, as a rule, disappear within 2-3 days after the procedure.
The pronounced therapeutic effectiveness is due to the direct introduction of an interferon inducer into the area of the primary lesion, which is localized in the anterior part of the vascular tract, achieving a higher concentration of interferon in the intraocular fluid.
Prodigiosan
- a polysaccharide of bacterial origin, its interferonogenic properties were confirmed by Yu.F. Maychuk and G.P. Nikitina (1981) on a model of experimental herpetic keratitis and uveitis. In the clinic, the authors recommend administering the drug subconjunctivally at a dose of 25-50 mcg.
To treat patients with herpetic lesions of the uveal tract, you can also use inhibitors of proteolysis enzymes - aprotinin (contrical, gordox).
Aprotinin (contrical, gordox)
- inhibitor of kallikrein and other proteinases. Inactivates plasma proteinases (plasmin, kininogenases, trypsin, chymotrypsin) of blood cells and tissues. Reduces the fibrinolytic activity of the blood by blocking plasminogen activators and, accordingly, the transition of plasminogen to plasmin.
G.S. Polunin et al. (1983; 1991), O.A. Kot (1990) is prescribed intravenously drip contrical at a dose of 1000 UIC/kg, gordox - 3000 units/kg daily for 7-14 days. The most effective are subconjunctival injections of Contrical and Gordox (300-500 UIC and 900-1500 IU, respectively) in combination with their intravenous drip administration (10,000 UIC and 100,000 IU, respectively).
Administration of aprotinin is contraindicated:
with disseminated intravascular coagulation, hypersensitivity to the drug, pregnancy, lactation.
Side effects should be noted:
arterial hypotension, tachycardia, thrombophlebitis at the injection site after long-term drip infusions; in isolated cases, anaphylactic shock.