Removal of the epiretinal membrane - This is a surgical intervention to excise the pathological film located above the macula. A similar procedure is prescribed if the patient’s vision is significantly reduced and there is a risk of irreversible damage in the macula area. The operation to remove the epiretinal membrane is performed in several stages. At the first stage, an inspection of the intraocular cavity is carried out, then the vitreous body is removed, and then a direct excision of the fold of the macula is carried out. Among the surgical complications are: infection, disruption of the integrity of the retina and its detachment, uncontrolled increase in IOP and the new appearance of the epiretinal membrane. Vision in the postoperative period is restored gradually over 4-6 months, which depends on the patient’s age, the area of excision and the presence of concomitant diseases.
What kind of disease is this
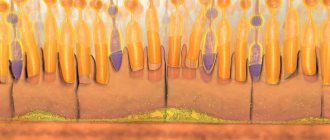
Medical terminology defines the epiretinal membrane of the eye as a thin fibrillar structure located in the structure of the vitreous body of the macula.
It is characterized by a lack of its own blood supply. As the pathology progresses, the epiretinal membrane thickens and scars, leading to serious and sometimes irreversible consequences.
ICD 10 code
According to the International Classification of Diseases, 10th revision, the epiretinal membrane of the eye has code H 35.3 Degeneration of the macula and posterior pole.
Medical terminology defines pathology as ophthalmological, characterized by the formation of a transparent thinned film in the inner shell of the eye in the center. Premacular fibrosis is a slowly progressive disease.
Has several stages. It is diagnosed during an initial consultation with an ophthalmologist. The pathology most often affects older people and especially women.
Causes
The etiology is primarily associated with the formation of pigment spots on the macula from under the inner lining of the eye. They release collagen, leading to deterioration in the transparency of the film.
Experts identify a number of reasons that can provoke the development of the disease:
- Destruction of the fundus.
- Diabetic angioretinopathy.
- Blockage of the central vein of the inner membrane of the eyes.
- Myopathy.
- Development of eye inflammation of varying intensity.
- Bleeding in the eye.
- Vitreous detachment.
- Injury to the organs of vision.
- Damage to the integrity of the retina.
- Presence of malignant tumors.
The main causes of the disease include ophthalmological pathologies.
Who's at risk
Risk factors for development are primarily associated with age-related changes in the body. In addition, patients with:
- Surgical interventions on the eyes.
- Vascular diseases of the retina.
- Inflammation of the back of the eyeball.
- Presence of premacular fibrosis in the other eye.
Epiretinal fibrosis is idiopathic in nature, which makes it difficult to identify the main cause of the disease
Surgical treatment of pathology
Medicines have a toxic effect on eye tissue, so only surgical treatment is permissible.
The operation begins with vitrectomy. During surgery, the posterior and medial parts of the vitreous tissue are removed. When the patient does not have a lens or it is replaced by a prosthesis, an additional stage of the operation is resection of the anterior part of the vitreous.
The second stage of the operation is to rid the patient of the cellophane macula. During its course, the film is picked up by the outer edge and rises slightly above the internal tissues of the eye. To remove the tumor, the surgeon uses tweezers. The inner border part of the film is cut off. Before this, it is marked with special coloring compounds.
Symptoms
Epiretinal fibrosis is characterized by hidden symptoms and increasing progression. The defeat is one-sided.
The initial stage of the pathology has no symptoms. Primary symptoms are manifested by a decrease in visual functions, the formation of a veil and distortion of the image.
As it progresses, the following characteristic symptoms of the macular fold appear:
- Development of photopsia.
- Visual impairment.
- The presence of flies and black spots before the eyes.
- A dark shadow or veil is formed.
- Visual acuity rapidly decreases.
- Formation of macular traction edema at a late stage of disease development.
A feature of the symptoms of epiretinal fibrosis is the presence of diplopia. With the development of premacular fibrosis, the inner lining of the eye within the macula is affected. This leads to loss of central vision, which is the main symptom of the disease.
The manifestation of the slightest disturbances in visual function requires immediate diagnosis in specialized clinics.
Symptoms and signs
The epiretinal membrane develops slowly and is most often characterized by unilateral lesions. At first, the pathological process is asymptomatic, the person does not notice the deterioration of vision. However, as it progresses, the first clinical signs begin to appear. Since the defect is located in the area of the macula, the main symptom of the disease is a decrease in central visual acuity, as a result of which the patient experiences difficulty reading, writing, watching TV and working with small parts. People with this diagnosis see a distorted image, in which numbers and letters are displaced, and straight lines are bent.
With a cellophane macula, the following manifestations can also be observed:
- blurred vision;
- color vision impairment;
- splitting of objects;
- distortion of the contours of objects;
- light flashes, lightning before the eyes;
- flashing “flies” before the eyes;
- formation of a veil;
- floating dark spots.
The epiretinal membrane is accompanied by significant visual impairment. People with this problem see the world as if through cellophane film.
Diagnostics
The examination is carried out by an ophthalmologist and consists of several stages. At the initial consultation, the specialist will listen to the patient’s complaints and conduct a visual examination using ophthalmoscopy.
Subsequently, depending on the state of eye health, the ophthalmologist may prescribe the following types of hardware diagnostics:
- Visiometry.
- Perimetry.
- Autofluorescence test.
- Optical coherence tomography.
- Radiography.
- Non-contact tonometry.
- Fluorescein angiography of the fundus.
- Ultrasound of the eye.
- Fluorescence tomography.
- Research on the Amsler lattice.
Regardless of the etiology of the disease and the stage of its development, the examination should be carried out comprehensively. If necessary, a laboratory examination or consultation with other specialists may be prescribed.
Suspicion of premacular fibrosis may require examination by a cardiologist, therapist or neurologist. This approach allows you to confirm the diagnosis and identify provoking ophthalmological diseases.
The maximum use of various types of studies to identify the macular fold is used at the initial stage of pathology development. This is due to the physiological features of the membrane structure, which at this stage is very thin and quite difficult to visualize.
Timely diagnosis contributes to the subsequent prescription of correct treatment and a speedy recovery without complications.
Epiretinal fibrosis
- Pathogenesis
- Classification
- Clinic of the disease
- Diagnostics
- Treatment
- Surgery
- Treatment of retinal tears
- Complications
The epiretinal membrane (epiretinal fibrosis, epimacular membrane, ERM) consists of collagen that accumulates on the inner surface of the central retina. Being in close interaction with the retina on which they grow, these membranes have a contracting effect, thus provoking metamorphopsia and other changes in the quality of vision.
According to histological studies, newly formed cell membranes consist of retinal pigment epithelial (RPE) cells, glial cells, fibrocytes and macrophages, while RPE cells may be the main cellular component of epiretinal membranes. Smiddy WE et al. (2001) conducted histochemical and morphological studies of collagen, which is part of epiretinal fibrous tissue. The authors identified 2 types of collagen: “new”, whose diameter exceeded 16 nm, and “old”, whose diameter was less than 16 nm. “Old” collagen was considered by the authors as natural collagen CT. This type of collagen was found in the vast majority of cases, which suggested the vitreal origin of fibrous tissue. “New collagen” was rare and, according to the authors, is of retinal origin.
The frequency of ERM formation in patients depends on the concomitant diseases against which it occurs. The idiopathic type of ERM is recorded in 7% of the population. Bilateral cases - in 30% of these cases. Clinically serious cases occur in 3-8.5% of eyes following surgical treatment of retinal detachment.
Age EPM is more common among representatives of the older generation. Postmortem studies have shown a 2% incidence of the disease in patients aged 50 years and 20% in patients aged 75 years.
In the history of ophthalmology, ERMs have had different names, such as
- proliferative vitreoretinopathy
- epiretinal membranes,
- cellophane maculopathy,
- preretinal macular gliosis,
- preretinal macular fibrosis,
- macular wrinkles,
- preretinal vitreous membranes,
- epiretinal astrocytoma membranes.
All these names refer to clinical and anatomical descriptions of the pathological changes that ERM leads to.
ERM may be associated with various ocular pathologies, such as
- detachment of the posterior hyaloid membrane,
- retinal tears,
- retinal detachment,
- occlusive retinal vascular diseases,
- inflammatory eye diseases and
- hemorrhages into the vitreous body.
- However, in a large number of cases, ERM occurs independently of these diseases, and is therefore classified as idiopathic epimacular membrane
Idiopathic membrane and membrane resulting from vitreous detachment are the most common. This article is devoted specifically to these types of epimacular membrane.
Pathogenesis
To date, there is no single theory explaining the causes and patterns of development of the epiretinal membrane. For a long time, the most widespread theory was that disruption of the integrity of vitreoretinal structures serves as the basis for the migration and proliferation of retinal pigment epithelial (RPE) cells, glial cells, monocytes and macrophages on the surface of the retina and in the vitreous body. Active proliferation of cellular elements leads to the formation of the epiretinal membrane (ERM), the appearance of retinal folding and the development of tangential tractions.
For the first time, one of the mechanisms for the development of ERM was described by Roth & Foos in 1971. According to this theory, the cause of the development of ERM is the pathological influence of partial detachment of the posterior hyaloid membrane (PHM) in the presence of its adhesion to the macula.
In some cases, due to stronger fixation of the retinal membrane to the retina, detachment of the retinal membrane is accompanied by a traction effect on the retina, the creation of defects in the internal limiting membrane (ILM), through which glial cells emerge onto the surface of the retina with their subsequent proliferation and formation of the ERM.
This theory well explained the mechanism of formation of so-called idiopathic ERMs, which develop without concomitant ocular diseases. Based on the results of numerous observations of the course of intraocular proliferation, it turned out that ERM is accompanied by a large number of eye diseases and conditions, and the development of ERM is not always accompanied by the presence of defects in the ILM. This fact necessitated the introduction of the term “secondary ERM”, which develops against the background of various eye diseases.
Thus, the development of proliferative tissue is one of the serious complications
- penetrating wounds of the eyeball,
- rhegmatogenous retinal detachment,
- excessively traumatic surgical interventions,
- laser photocoagulation over a large area of the retina
- diabetic retinopathy
- thrombosis of the central retinal vein
- intravitreal hemorrhage
ERMs are avascular fibrocellular membranes that grow on the surface of the retina and can lead to varying degrees of visual impairment. The cells of these membranes, being attached to the retina, can grow and form dense membranes that cover the surface of the retina and lead to various types of visual impairment depending on the severity of the deformation, the location of the accumulation of such cells and other adverse effects on the retina.
There is still debate regarding the origin of the cells that make up such membranes. Earlier reports suggested that glial cells (primarily fibrous astrocytes) from the inner layers of the neurosensory retina grow through tears in the internal limiting membrane (ILM) resulting from retinal tears or posterior vitreous detachments.
Recent vitrectomy specimens show that epiretinal membranes are composed of glial cells, retinal pigment epithelial cells, macrophages, fibrocytes, and collagen cells. These constituent cells may be in different proportions depending on the etiology of the membrane. Membranes resulting from retinal tears or detachments or cryopexy are composed primarily of retinal pigment epithelial cells, whereas cells of glial origin predominate in idiopathic ERMs. Moreover, these cells tend to change their appearance and function, although to a small extent.
Posterior vitreous detachments (PVD) in idiopathic ERM occur in 75-93% of cases. There is an opinion that detachment of the posterior wall of the vitreous body can influence the occurrence of ERM in different ways.
PVD can lead to retinal tears, which in turn release retinal pigment epithelial (RPE) cells, which begin to form a membrane. Small tears in the internal limiting membrane (ILM) following posterior vitreous detachment can also allow free retinal astrocytes to enter the vitreous cavity, where they can further proliferate. Finally, vitreous hemorrhages and/or inflammatory processes accompanying PVD may also stimulate epimacular membrane formation.
Formation of ERM without posterior vitreous detachment (PVD) may precipitate the development of vitreomacular distension syndrome (VMS) in patients. Shang et al describe the VMR syndrome using optical coherence tomography studies of the retina and analyzing the ultrastructural relationships in specimens obtained during surgery. They documented the proliferation of fibrous cells between the inner surface of the retina and the posterior wall of the vitreous, which leads to excessive vitreoretinal traction.
Bovey and Uffer report that the phenomenon of internal limiting membrane rupture is also associated with the occurrence of ERM. They hypothesized that tears and folds of the internal limiting membrane are more likely when ERM forms before posterior vitreous detachment, resulting in a cleavage plane occurring more often between the internal limiting membrane and the inner retina than at the surface of the internal limiting membrane.
Classification
Gass proposed a classification system based on the appearance of the membrane and the underlying retinal tissue and blood vessels.
- Stage 0 membrane - “cellophane maculopathy” At stage 0, the membrane is translucent and is not accompanied by any retinal deformations.
- a cellophane-like reflection appears from the inner surface of the retina during ophthalmoscopy
- on the cross-section of OCT, the foveal profile is not changed, the central thickness of the retina is normal. En Face shows faint diffuse folds on the surface of the retina
- At stage 1 of the membrane, uneven wrinkling of the inner surface of the retina is formed.
- General shrinkage of the macula along its entire thickness can occur simultaneously with retinal edema, small hemorrhages, cotton-wool exudates, and occasionally small-sized macular retinal detachments.
Types of epimacular changes in the vitreous
- Inflammatory process of preretinal vitreum with minimal fibroblastic activity (“wet” membrane)
- Inflammatory process of preretinal vitreum with moderate fibroblastic activity
- Inflammatory process of preretinal vitreum with pronounced fibroblastic activity
- Predominance of fibrocytes and fibroblasts over inflammatory cells
- Mature fibrous tissue
Clinic of the disease
The type and extent of symptoms experienced by the patient depend largely on the thickness of the membrane, the degree of retinal deformation it causes, the location of the wrinkling, and the presence or absence of macular detachment or edema.
Common symptoms accompanying ERM range from no symptoms at all to severe visual impairment.
In the early stages of ERM development, vision either does not deteriorate or deteriorates to a very small extent. As the membrane progresses, visual impairment is often subtle and patients have difficulty describing it.
- The most common symptom is mild metamorphopsia
- Micropsia or distortions detected by the Amsler grid may be observed.
- progressive decrease in central vision,
- deterioration of color perception,
- blurred vision
- diplopia
In 78-85% of cases, vision remains better than 0.3, of which in 56-67% of cases it is better than 0.5. And only in 2-5% of cases there is a deterioration in vision to 0.1.
At the same time, with the simultaneous formation of ERM and local macular detachment, there is a significant deterioration in vision. Only 7% of cases have vision of 0.3 or better, while 56% have vision worse than 0.1. Vision remains low in these cases even after successful surgical treatment.
Diagnostics
Epiretinal membrane can be diagnosed by ophthalmoscopy - examination of the fundus of the eye. It shines slightly, reminiscent of cellophane film. In the initial stage, the thin epiretinal membrane is almost invisible. The effect of epiretinal film on vision is determined by the Amsler grid test.
Optical coherence tomography of the eye can help identify ERM, exclude it in the differential diagnosis, and objectively measure other effects of ERM on the retina, such as macular thickening, the presence or absence of macular edema, and any possible tractional effects of the vitreous on the retina. OCT can also monitor the process of retinal architecture returning to normal after surgery, as well as detect tension or folds that form on the retina.
Fluorescein angiography is usually performed to ensure that there are no other eye diseases that may have signs of ERM. Early-stage macular holes usually show a background glow across the entire hole, which disappears in deeper stages. Epimacular membranes with pseudotears usually do not transilluminate in this way because healthy retinal tissue at the site of the pseudotear prevents this from happening.
Exudative macular degeneration can also take the form of ERM, however, FA is characterized by early luminescence, which makes it possible to clearly distinguish it from the epimacular membrane. ERM fluorescein angiography may detect minute perifoveolar capillary leaks or evidence of ischemia due to capillary obstruction. This can significantly help in predicting the patient's postoperative condition.
Treatment
Treatment should be carried out earlier, prior to the stage of development of ERM, when it can be clinically identified. Thus, it is known that cytostatics can slow down the proliferation rate, but they have a toxic effect on the structures of the eye.
Radiation therapy is another possible mechanism to prevent proliferation, but the high sensitivity to radiation of the ocular structures and especially the lens makes this treatment unsuitable for use. Intravitreal administration of high doses of corticosteroids also has an inhibitory effect on cell proliferation, but can cause a number of side effects: the development of steroid glaucoma, cataracts.
To date, no effective and safe agents have been developed that can have an antiproliferative effect in the early stages of ERM formation. Once formed, the fibrous structure can serve as a scaffold for the attachment of other types of cells - hyalocytes and macrophages. There is no doubt that with the onset of the contractile phase of the proliferative process on the surface of the retina, complications such as macular edema, which develops as a result of contraction of the ERM or as a result of vitreomacular traction, are possible.
Surgery
Surgical removal of clinically severe ERMs usually results in improved vision as well as an improvement in the external biomicroscopic appearance of the retina. Studies have shown that after surgery, 78-87% of patients with idiopathic epimacular membrane and 63-100% of patients with a membrane formed due to retinal detachment received at least a 2-2.5-fold improvement in vision.
The appearance of epiretinal membranes is associated with the proliferative growth of glial cells (astrocytes, Müller cells), which can be caused by damage to the internal limiting membrane of the retina. When performing vitrectomy, you need to remember that often, despite PVD, the PVD can maintain a connection with the macular zone, and increased traction during removal of the PVD can cause ruptures in the foveal zone. Typically, membrane removal is possible through peeling. In order to start membrane peeling, it is necessary to select the edge of the membrane with tweezers or a spatula, but the most gentle way is to release the edge of the membrane using a cannula with an elastic silicone end or a Tano scraper.
With light movements, the membrane is moved with the silicone end from the periphery to the center, while the edge of the membrane comes off from the retina and rises, and can be easily grabbed with tweezers. The most convenient in these cases are tweezers with pneumatic drive. Grabbing the selected edge of the membrane with vitreal tweezers, peeling is performed in the direction from the edge to the center. The membrane is separated and removed. Small membranes or fragments of them can be removed from the eye with tweezers. If the membrane is large, then after separation from the retina its final removal should be done with a vitreotome.
Treatment of retinal tears
After removing the membrane, it is necessary to check the retina for the presence of breaks in it both in the posterior pole of the eyeball and in the periphery of the eye. No matter what techniques and tricks the surgeon resorts to and no matter how delicately he removes the membranes, the result of his work can be offset by possible retinal detachment due to breaks not noticed in time. To treat ruptures that are not burdened by the accumulation of subretinal fluid, laser retinopexy or cryoretinopexy is used. The presence of a significant amount of subretinal fluid requires internal drainage under air pressure, retinopexy or gas tamponade.
Complications
The most common complications during vitrectomy and removal of the epiretinal membrane are intraocular bleeding and the occurrence or increase of retinal tears. After removal of the membrane from the surface of the retina, petechial hemorrhage may be observed along the inner surface of the retina, but this usually resolves within a few days after surgery.
More serious bleeding can occur when a vessel in close proximity to it is damaged during the cutting of a membrane that is strongly fused to the surface of the retina. Such bleeding can be stopped by temporarily increasing intraocular pressure or by cauterizing the affected vessel. The occurrence of retinal tears is the most serious complication that can occur during surgery. The incidence of ruptures in the posterior pole of the eyeball varies from 0 to 15%, while ruptures in the periphery occur in 5-6% of cases. Careful, gentle membrane release procedures coupled with careful inspection of the retina in the periphery can ensure that postoperative problems associated with retinal tears are minimized.
The most common postoperative complication is accelerated progression of nuclear lens sclerosis, which can develop over time in 75% of operated eyes. After surgical removal of the ERM, cataract phacoemulsification usually has to be performed within the first 2 years.
Postoperative retinal detachment may be caused either by an undetected retinal tear during surgery or by a new tear that may form due to contracture of the remaining anterior vitreous. Such detachment occurs in 3-6% of cases and necessitates a new surgical intervention, which, however, almost always successfully solves the problem.
Recurrence of ERM occurs in less than 5% of idiopathic cases, but the risk of its occurrence increases with retinal detachment and inflammatory processes in the eye.
Treatment
A characteristic feature of the epiretinal membrane of the eye is the slow progression of the pathology. Therefore, the treatment of epiretinal fibrosis directly depends on the degree of its development and the general health of the patient.
The initial stage of the disease, which is accompanied by a stable state of the membrane without deterioration, is supported by general therapy. Local medications and strengthening drugs are used. A prerequisite is systematic observation by a doctor to timely determine the progression of the disease.
Operation
Advanced stages of premacular fibrosis require immediate surgical intervention. Drug treatment for this pathogenesis is unsuccessful.
The operation involves several stages:
- The preparatory stage is vitrectomy.
- The main stage is resection of the affected membrane.
- The final stage involves examining the retina to identify damage. If necessary, laser retinopexy or cryoretinopexy, gas tamponade, or special drainage can be used to restore its integrity.
Surgical intervention for diagnosing macular folds is carried out as planned. Urgent hospitalization followed by urgent surgery is possible with severe swelling of the macula.
Traditional methods
Alternative medicine in the treatment of epiretinal fibrosis is used as supportive treatment. The choice of drugs is carried out in consultation with the doctor.
The most effective folk remedies for eye health are:
- Beetroot and carrot fresh juice.
- Eating fresh blueberries, cranberries and blackberries.
- Herbal teas with lemon balm and lemongrass.
- Herbal decoctions and infusions from the buds of birch, mallow, eyebright or burdock.
Traditional methods in the treatment of pathology are exclusively auxiliary. It is impossible to cure the disease with their help.
Therapy should be carried out comprehensively. If the disease is secondary, then the underlying pathology must be treated.
The choice of treatment method and the need for surgery is made exclusively by the doctor. Self-medication of the macular fold can lead to irreversible negative consequences.
Is it possible to save vision?
When diagnosed with macular epiretinal membrane, surgical treatment is considered the most effective, during which the vitreous body and the membrane itself are removed. In most cases, this operation allows you to restore vision by about 20%. It is worth noting that surgical treatment is not performed on all patients, but only on those who have a significant deterioration in visual function or are at risk of spreading the pathological process to the macula. In the absence of such indications, the epiretinal membrane is simply observed by the doctor during regularly scheduled visits. According to ophthalmologists, the prognosis for the preservation of vision will be favorable if the diagnosis was made to the patient on time, medical control over the progression of the disease was carried out, and ophthalmic surgery was performed in a timely manner.
MagazinLinz.ru team
Cost of treatment
The rapid progression of epiretinal fibrosis contributes to regular vision loss. To avoid the progression of partial or complete blindness, surgery is performed.
The cost of treating fibrosis depends on the complexity of the pathology, as well as many associated factors. On average, the price for an operation in various medical centers varies within 84 thousand rubles. State clinics provide treatment services much cheaper than specialized private ophthalmological centers.
It is not recommended to skimp on eye health. Preference should be given to highly qualified specialists. This approach will avoid relapse of the disease and the occurrence of serious complications after surgery.
Cost of surgery to remove epiretinal membrane
The cost of surgery to remove the epiretinal membrane depends on the extent of the intervention and the chosen surgical method. Thus, excision of pathology using a laser is a more modern, low-traumatic and expensive technique. In our clinics in Moscow and Naro-Fominsk, surgical interventions to remove the epiretinal membrane are performed using modern equipment, with the involvement of highly qualified specialists. The cost of removing the epiretinal membrane at Dr. Shilova’s Clinic ranges from 35,000 to 69,000 rubles.
Forecast
Timely contact with an ophthalmologist and comprehensive comprehensive treatment allow doctors to guarantee a favorable treatment prognosis.
At an advanced stage of development of the pathology, which is accompanied by rapid loss of vision, a well-chosen therapeutic course can partially restore the functions of the visual organs. Visual acuity will improve by several indicators, but will require constant monitoring and maintenance therapy.
Possible complications
Surgical treatment is quite complex and traumatic. In medical practice, the following possible complications are distinguished:
- Increased ophthalmotonus.
- Infectious lesions of the organs of vision.
- Rupture or detachment of the retina of the operated eye.
- Retinal hemorrhages.
- Rapid development of secondary cataracts.
- Macular edema.
- Macropsia.
All complications after treatment negatively affect visual acuity, which is a provoking factor in the development of blindness.
Preventive measures
The pathology does not have specific preventive measures for this pathology. Compliance with preventive measures is based on:
- Stabilization of hormone levels in the blood.
- Prevention of venous blockage and vascular embolism.
- Adhering to safety regulations at work.
- Systematic medical examinations by specialized specialists.
- Enriching the daily diet with foods that have a beneficial effect on the quality of visual functions.
Prevention allows not only to preserve the results of treatment, but also to prevent the development of pathology.
Reviews
- Elizaveta, 45 years old. As a result of secondary cataracts, I developed an epiretinal membrane of the eye. After the examination, the doctor said that treatment was only possible with surgery. I was satisfied with the result, my vision stopped deteriorating.
- Nikolai is 66 years old. When my vision began to deteriorate, I didn’t think much of it. I thought that this was typical with age. I tried to support him with the help of traditional medicine. When I took my daughter to the doctor, I was diagnosed with epiretinal fibrosis. An emergency operation was performed; of course, my vision was not restored, but it stopped deteriorating so quickly.
- Tamila, 51 years old. After eye surgery, I regularly undergo examinations with a doctor twice a year and take medications prescribed by the doctor. The pathology has stopped progressing, there is no relapse of the disease. I regret that I didn’t seek help from specialists earlier.
The pathology can only be treated surgically. Timely treatment eliminates the development of irreversible consequences.
Video on the topic:
Prevention
There are no specific methods for preventing epiretinal membrane. Non-specific measures are considered mechanisms that help control hormonal levels in order to prevent the development of blockages and embolism. It is also important to follow safety rules while performing production tasks.
One of the prevention methods is regular visits to the ophthalmologist. In such cases, it is important to undergo a thorough examination at least 2 times a year, since 10% of patients experience re-development of the disease.