What kind of disease is this?
The very origin of the term “ophthalmoplegia” comes from the Greek word plege - “blow, defeat”.
Ophthalmoplegia (photo)
Neurologists and ophthalmologists associate this oculomotor disorder with nerve palsy and inadequate functioning of the muscles that facilitate normal movement of the eyeballs and eyelids.
From an anatomical and physiological point of view, eye movement is determined by certain structures of the brain:
- vertical movement of the eyeballs is realized through the structures of the midbrain;
- horizontal - through the pons;
- The cerebellum ensures adequate fixation of gaze.
With ophthalmoplegia, when some parts of the brain cannot realize their functions (nerve fibers are not activated properly), several types of muscles of the eye movement system are susceptible to pathological effects:
- external - responsible for the movement of the eyeball and raising the upper eyelid; with non-nominal innervation of these muscles, external ophthalmoplegia occurs;
- internal – contribute to the functioning of the pupil, its contraction and dilation, and are responsible for accommodation (adjustment of focus) of the eye; In case of disruption of these muscles, internal ophthalmoplegia appears.
Based on how widely the disorder affects the muscles of the visual organ, ophthalmoplegia occurs:
- complete , a distinctive feature of which is the joint damage to the internal and external muscles of the eye;
- partial , suggesting either an external form - pathology of the external muscles of the eye, or an internal form - paralysis of the internal muscles.
Video:
Treatment methods for ophthalmoplegia
Treatment consists of eliminating the disease that caused the paralysis, as well as restoring the functionality of the muscles and nerves. Therapeutic interventions include several aspects.
Drug treatment. The patient may be prescribed various medications depending on the etiology:
- anti-inflammatory drugs;
- topical corticosteroids;
- vitamins B and C;
- nootropics to improve nervous activity;
- drugs that eliminate muscle weakness.
Hardware therapy. Along with taking medications, treatment using hardware procedures - electrophoresis, phonophoresis, acupuncture - also produces effective results. This helps strengthen the eye muscles and eliminate spasm.
Surgical intervention. It is prescribed if it is necessary to eliminate the tumor that is the cause of paralysis, as well as restore muscle activity of the eyes, and raise the upper eyelid with ptosis.
Three methods are used to influence muscles:
- myotomy (dissection);
- recession (pushing back);
- tenomyoplasty (lengthening).
Surgeries for ophthalmoplegia are aimed at restoring the correct balance between the eye muscles. The doctor decides what type of intervention is necessary, taking into account the existing form of pathology and its severity, the patient’s age and other characteristics. As a rule, several muscles are operated on at once. There are cases when a strengthening operation is performed on one eye and a weakening operation on the other.
The success of treating ophthalmoplegia depends on timely contact with specialists, as with many other diseases, and not only eye ones.
ICD-10 code
In the disease classifier, ophthalmoplegia is presented in the structure of several classes associated with specific disorders.
Most often, this disease is mentioned in the section “paralytic strabismus” (coding in ICD-10 - H49 ):
- complete (external) ophthalmoplegia (with code H3);
- progressive external ophthalmoplegia (with code H4);
- in subclass H8, among other paralytic strabismus - external ophthalmoplegia NOS (i.e., a disorder of an unspecified nature - not otherwise specified).
The remaining types of ophthalmoplegia are found in several subsections:
- G23 “other degenerative diseases of the basal ganglia” - in subclass 1 as “progressive supranuclear ophthalmoplegia”;
- in other disorders of conjugate eye movement (H51) – we find ophthalmoplegia in subclass H2 as “intranuclear ophthalmoplegia”;
- Among the disorders of refraction and accommodation (H52), “internal ophthalmoplegia (complete) (total)” is prescribed (subclass H5 “impaired accommodation”).
Causes
Ophthalmoplegia manifests itself as a consequence of a number of unfavorable conditions and physiological processes.
It may be based on the following factors:
- Pathological phenomena of the brain (all kinds of tumors of its base, inflammatory processes and diseases, cerebral infarction).
- Traumatic effects on the parts of the brain responsible for the functions of eye movement.
- Intoxication with drugs (eg, barbiturates, antidepressants, etc.).
- Diseases that contribute to degenerative processes (progressive paralysis, spinocerebellar degeneration).
- Vascular diseases (thrombosis, vascular aneurysm).
- Endocrine and diabetic disorders affecting the visual system.
- Tuberculosis of the central nervous system.
- Injuries and damage to the orbit.
Some studies support pregnancy as a cause of ophthalmoplegia. Also a risk factor are the consequences of alcohol abuse - degeneration of the brain substance occurs as a manifestation of alcoholic encephalopathy.
Treatment
Treatment of internuclear ophthalmoplegia is carried out based on the causes of the disease. And these reasons must be eliminated first. If the cause is a stroke, it is usually treated with blood thinners. In some cases, it is possible to use surgical methods to widen the arteries and remove accumulated blood clots.
Internuclear ophthalmoplegia in multiple sclerosis: in the absence of the desired effect of treatment, for example, corticosteroids, plasmapheresis is performed in multiple sclerosis. However, at this moment the use of other medications cannot be ruled out, since the resulting effect from the blood purification procedure may be lower than predicted.
When internuclear ophthalmoplegia is caused by certain neoplasms, it is necessary to approach treatment tactics very carefully. When choosing it, proceed from the level of growth and location. Most specialists choose a conservative form of treatment. This is justified by the fact that surgical removal of tumors from the brain stem is extremely difficult.
Kinds
In addition to the types already mentioned in the initial description of the disease, ophthalmoplegia exists in several other variants.
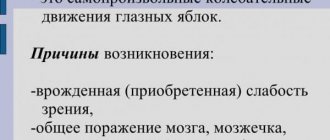
- A type in which there is a violation of horizontal eye movement is called internuclear or internuclear ophthalmoplegia.
This disorder occurs due to damage to the connecting link between the eyes and brain structures - the medial longitudinal fasciculus (nerve fibers). The conjugal movement of both eyes is also impaired here. - Supranuclear (progressive) ophthalmoplegia manifests itself through “one and a half syndrome” - a pronounced inability to move the gaze at will in different directions, although reflex eye movements are not impaired. The reaction of the pupils and convergence (eye contact) are also preserved.
- Toloza-Hunt syndrome (HTS) affects a number of structures of the superior orbital fissure (represented here are the artery and vein, part of the trigeminal nerve, several nerves involved in the functioning of the eyeball - oculomotor, trochlear, abducens) and has several more names that characterize its features: superior syndrome orbital fissure and painful ophthalmoplegia. Pain is observed in the orbital area, patients also complain of double vision, swelling of the eyelids and conjunctiva.
- Painful ophthalmoplegia also manifests itself as a pain syndrome, but unlike CTX it is a “companion” of a number of other diseases of the visual organs of a neurological nature.
Global gaze palsy or total ophthalmoplegia is characterized by loss of the ability to move the gaze.
This type of disease is a rather rare phenomenon and more often reveals itself as a concomitant component of a symptom complex of other diseases (tetanus, pituitary gland disorders, botulism).
Diagnostics
The progression of the disease can also be detected by specific external signs. For this, a consultation with an ophthalmologist and a neurologist will be sufficient. However, in order to correctly determine the cause that provoked the development of ophthalmoplegia, various studies are used using specialized equipment.
Among them are:
- computed tomography of the head and neck (this procedure allows you to detect and determine the type and size of tumor formations that could become the probable cause of the disease);
- X-ray of the skull in both projections (based on the results of the study, a picture is shown where you can examine and determine the nature of the damage, if any, and in addition find out the condition of the sinuses);
- X-ray of the orbital sockets with a contrast reagent (shows the distinctive characteristics of the eyeballs that cannot be seen during a routine examination);
- antigraphic examination of the cerebral vasculature (helps identify problems associated with blood flow and detect aneurysms).
Computed tomography machine
Symptoms
The characteristic symptoms of ophthalmoplegia are the following clinical manifestations:
- disorder of the motor functions of the eyeball (its mobility is reduced and limited, or absent altogether);
- the presence of mydriasis is noted (a condition of the eye when the pupils are unnaturally dilated);
- swelling of the tissue around the eyeball appears;
- protrusion of the eyeball is observed;
- there is diplopia (doubling of the perceived object or object);
- ptosis (abnormal drooping) of the upper eyelid;
- the pupils do not react to the light beam entering the eye;
- the quality of vision is reduced;
- there is pain (both in the eye itself and in the tissues around it - forehead, upper jaw).
Possible complications
Ophthalmoplegia can lead to accommodative disturbances and decreased visual acuity. Internuclear ophthalmoplegia can be complicated by nystagmus. With this type of disease, there is a high risk of an infectious and inflammatory pathological process, since tear production and eyelid function are impaired.
The pathology may be complicated by:
- exophthalmos;
- xerophthalmia;
- conjunctivitis.
Timely assistance and prevention of the cause of visual impairment will help avoid complications and long-term treatment.