Superior orbital fissure syndrome (SOFS) is a complex of impaired function of the cranial nerves (III, IV, V, VI) that exit through the superior orbital fissure (SOF). The three main provoking factors are trauma, tumor, inflammation.
The disorder of traumatic origin was first described by Gershfeld in 1858. 1896, Rochon-Duvigneau reported the syndrome as a pathological formation in four patients with syphilis, Lacke defined the complete syndrome in 1962.
Any unnatural narrowing of the SOF due to high-impact trauma to the upper and middle surface of the face (frontobasal skull, zygomatic fractures) can precipitate this condition. Direct bony compression or compression hematoma causes signs and symptoms of the syndrome, which are complete or partial, depending on the degree of compression of the anatomical structure.
Accelerates after reduction of the midface fracture, where it was previously absent.
The incidence is less than 1%. This is a complex consisting of periorbital edema, proptosis, drooping, numbness of the forehead, paralysis of the extraocular muscles due to disruption of the III, IV, VI and first division of the V cranial nerve. Superior orbital fissure syndrome does not involve the optic nerve and vision is not affected.
With involvement of the optic nerve and subsequent visual impairment - orbital apex syndrome, when orbital examination is recommended as an emergency. Cranial nerve IV is the least damaged. VI – is most severely damaged, as it passes through the common tendon ring and is close to the larger wing of the sphenoid bone.
Description
Superior orbital fissure syndrome is a rare complication of craniofacial trauma. The diagnosis is based on the clinical picture, which is confirmed by x-ray examination. In the absence of compression by fracture fragments, a conservative approach with megadose steroids is the first line of treatment.
The prognosis is not as good if symptoms are caused by displaced bone fragments. If bone compression is evident, surgical decompression should be planned. Associated facial fractures, especially those with orbital impact, should be reduced early to relieve intraocular pressure if the general condition is stable. After proper treatment, complete restoration of cranial nerve function can be expected. By the end of 6 months, improvement reaches a plateau.
Traumatic superior orbital fissure syndrome is a rare complication of craniomaxillofacial trauma with an incidence of less than 1%. The syndrome is characterized by ophthalmoplegia, ptosis, proptosis of the eye, dilation and fixation of the pupil, as well as anesthesia of the upper eyelid and forehead.
Etiology and diagnosis are established after a detailed physical and radiological examination. The treatment algorithm for traumatic syndrome of the superior orbital fissure includes the use of steroids, surgical decompression of the superior orbital fissure,
Superior orbital fissure syndrome is a rare complication after craniofacial trauma.
Causes
The disease can be congenital or acquired.
The main causes of the congenital form.
- A rare genetic disease with an autosomal dominant pattern of inheritance. Distant relatives may be sick, but parents are usually apparently healthy. Males are more often affected. Combined with other eye anomalies and disorders of the cardiac, skeletal, and reproductive systems.
- Exposure to negative factors during intrauterine development that disrupt the formation of the eyelids and palpebral fissure. The second month of pregnancy is especially important - the time when the eyelids form, and the seventh, when they split into the upper and lower eyelids.
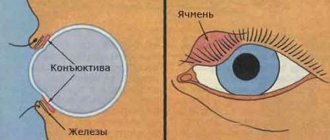
The acquired form is more common than the congenital form and develops against the background of chronic inflammatory diseases of the organs of vision. With long-term blepharitis, conjunctivitis, and trachoma, adhesions may form in the area of the outer canthus. A number of diseases of the endocrine, nervous, and muscular systems can contribute to the occurrence of pathology.
Causes, symptoms
There are several causative factors including inflammation, tumors, trauma, in addition to non-specific etiologies that cause superior orbital syndrome. The literature reports inflammation and infection of the meninges of the central nervous system, cavernous sinus, and retrobulbar space caused by syphilis and tuberculosis.
Neoplasms arising in the meninges, bones, brain tissue near the SOF area, tumors, can produce the disorder. In addition to medical etiology, the main traumatic brain injuries are craniofacial, including skull fracture, zygomaticomaxillary complex, orbit, LeFort II, III fractures. With post-traumatic symptoms, the contents of the crack are torn or compressed by displaced fragments.
However, increased internal orbital pressure caused by swelling or bleeding at the time of injury compresses the nerves against the bony edge of the fissure. The degree of participation depends on the pressure created. Therefore, recovery is influenced by the rate of absorption of extravasated fluids.
A blow to the skull bone may extend forward to the roof of the orbit, involving the greater wing of the sphenoid bone, and result in the formation of a hematoma. Internal carotid artery aneurysm caused by trauma has been noted in the literature as another cause of superior orbital fissure syndrome. The disorder occurs after repair of midfacial fractures in patients with a congenitally narrow SOF.
Greater impact force near the orbit during injury leads to an increased incidence of superior orbital fissure syndrome.
Diagnostic methods
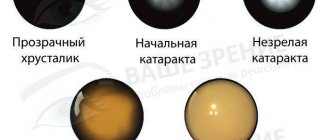
Pathology can be detected during examination by a specialist, and ophthalmoscopy is used for confirmation.
Superior orbital fissure syndrome can be identified by an external examination of the patient by a neurologist or ophthalmologist. For a more detailed study of the disease, it is necessary to conduct a number of laboratory and instrumental studies. It includes ophthalmoscopy with visualization of the fundus and the condition of the vascular network, magnetic resonance imaging, which allows to identify neoplasms, hematomas and cysts of the brain or orbit. Angiography of the vessels of the eyeball is also performed. Doctors recommend conducting a general and biochemical blood test, and also donating urine. If an infectious lesion is suspected, blood PCR is performed to determine the DNA of a possible pathogen and an enzyme-linked immunosorbent assay to detect antibodies to a certain type of virus or bacteria. If an autoimmune process is possible, an immunogram is performed.
Diagnostics
Clinical symptoms are attributed to nerve involvement. External ophthalmoplegia is secondary to disorders of the oculomotor, trochlear, and abducens nerves.
Find out more Causes and signs of edema syndrome
Ptosis develops due to loss of tension and function of the superior levator rod muscles, involving the superior branch of the oculomotor nerve, loss of tone of the Müller muscles, involving the sympathetic fiber arising from the cavernous sinus. Proptosis is caused by decreased tension in the extraocular muscles. A fixed dilated pupil with loss of accommodation occurs due to the destruction of parasympathetic fibers flowing with the oculomotor nerve.
Compromise of the lacrimal and frontal nerves of the ophthalmic branches of the trigeminal nerve leads to anesthesia of the forehead and upper eyelid, lacrimal hyposecretion, retro-orbital pain, and neuralgia along the nerve path. Due to disruption of the sensory nasopharyngeal nerve, anesthesia of the cornea and bridge of the nose may occur with loss of the corneal reflex.
When the disruption is partial, the corneal reflex remains intact. Involvement of the optic nerve, including the above symptoms, is known as orbital apex syndrome, a term coined by Kjaer.
Symptoms are present depending on the severity of the damaged structures and the stage of healing at the time of examination of the patient.
The term "partial superior orbital fissure syndrome" indicates partial or complete involvement of the third and sixth cranial nerves along with the nasopharyngeal nerve. These three structures that run inside the tendon ring are more susceptible to compression.
Diagnosis of traumatic SVGS is based on clinical symptoms, the signs mentioned above and x-ray examination. Optimal viewing of the SOF with a posterior/anterior orbital view is obtained with the head tilted at 20-25 degrees (Caldwell view) before CT appears. However, in patients with severe trauma, obtaining plain films is often difficult and dangerous, especially if there is associated neck trauma.
Angiography
Angiography is a useful tool for identifying injury or carotid aneurysm causing the syndrome. CT is an excellent tool for radiological diagnosis in trauma patients. In contrast to plain radiographs, small bone fragments or retroorbital hematoma with compression around the SOF are visualized using thin computed tomography (2 mm slices).
CT
CT scans show that orbital apex fractures are more common than previously thought. New spiral CT equipment is a promising tool for improving diagnostic accuracy.
Helps avoid the discomfort of neck hypertonia when obtaining coronal CT slices using a traditional CT machine, and also provides information related to adjacent brain injuries and associated craniofacial fractures. Currently, SOF width is measured using computed tomography.
Tolosa-Hunt syndrome
Tolosa-Hunt syndrome is a symptom complex that is clinically manifested by various combinations of the following symptoms: pain in the orbit, double vision, drooping eyelid, and limited movement of the eyeball. The condition occurs with pathology of the structures passing through the superior orbital fissure of the skull (orbital artery and vein, abducens, trochlear, oculomotor nerves, first branch of the trigeminal nerve) and the adjacent cavernous sinus. A significant role in the development of the syndrome is played by autoimmune disorders, provoked by exposure to various factors on the body - hypothermia, previous infections, psycho-emotional stress, etc.
The main causes of Tolosa-Hunt syndrome:
Vascular malformations of the brain are a congenital disorder of the development of the circulatory system, with the formation of vascular glomeruli of various shapes and sizes, clinically appearing almost always against the background of arterial hypertension;
Brain tumors, with Tolosa-Hunt syndrome developing subacutely, without obvious provocation. The tumor process can be metastatic in nature. In this case, the primary focus of the tumor can be in the lungs, bronchi, prostate gland, skin).
Orbital myositis is an inflammation that affects one or more extraocular muscles.
Cavernous sinus thrombosis is a blockage of one of the sinuses of the dura mater of the brain by a blood clot. Located near the superior orbital fissure. The function of the cavernous sinus is to provide venous drainage from the brain and eyeballs, thereby regulating blood circulation within the skull and indirectly intracranial pressure. Thrombosis, sometimes complete occlusion, of the cavernous sinus causes inflammation of its walls. The cause is an infection, usually oto- or rhinogenic, less often – a pustular lesion of the facial skin in the area of the nasolabial triangle.
Idiopathic syndrome. They talk about it when the examination does not reveal the cause.
Diagnostic criteria for Tolosa-Hunt syndrome :
(A) one or more attacks of unilateral orbital pain that persists for several weeks if untreated;
(B) palsy of one or more cranial nerves (III, IV and/or VI), as well as detection of granuloma by MRI or biopsy;
(C) nerve palsy coincides with the onset of pain or occurs within two (2) weeks after it;
(D) paresis and pain resolve within 72 hours after adequate treatment with corticosteroids;
(E) other causes of pain have been excluded by appropriate testing methods.
Clinical picture . As a rule, the first neurological manifestation of Tolosa-Hunt syndrome is pain of varying intensity, localized retrobulbar, in the frontal, superciliary or temporal regions. A few days later (less often simultaneously), double vision (diplopia), strabismus and limited mobility of the eyeball on the side of pain appear. When all nerves passing through the superior orbital fissure are affected, total ophthalmoplegia develops (in approximately every fourth patient). The pain syndrome is caused by irritation of the first branch of the trigeminal nerve (ophthalmic), running next to the trunk of the oculomotor nerve. The localization of pain may vary: orbit, forehead, temple, root of the nose. The intensity of pain has a wide range - from minimal to severe. Atypical (painless) variants of this syndrome, associated with the localization of the pathological process before the entry of the V pair of cranial nerves into the cavernous sinus, should be taken into account.
When the pathological process is localized in the area of the orbital apex, neurological symptoms are often combined with a disturbance of the visual analyzer, which is manifested by edema or atrophy of the optic nerve head, central scotoma. Frequent ophthalmological symptoms of Tolosa-Hunt syndrome are exophthalmos and chemosis, which are caused by infiltration of retrobulbar tissue and obstruction of venous outflow from the orbit.
Thus, Tolosa-Hunt syndrome is a polyetiological syndrome. Detection of Tolosa-Hunt syndrome in patients requires a thorough differential diagnosis. If the autoimmune nature of the disease is established, glucocorticoids are highly effective, course treatment of which in large doses is carried out under medical supervision.
The prognosis of the disease depends on its cause.
Treatment
Treatment of the syndrome depends on the cause, if one is identified. Patients present with chemosis, pulsatile exophthalmos, orbital or frontal edema, and blurred vision in addition to clinical findings; Traumatic CCSF should be suspected as a cause of superior orbital fissure syndrome.
Prompt carotid angiography is performed to confirm CCSF, which is successfully embolized using a removable balloon or coils. Symptoms of ptosis, facial numbness, and ophthalmoplegia disappear gradually over several months after embolization.
The appropriate treatment for trauma-inducing disorder is not clearly defined in the literature due to the relatively small number of reported cases. It ranges from conservative treatment to steroids and surgery.
Conservative
A conservative approach using observation alone is suggested because complete or partial spontaneous recovery of motor and sensory function usually occurs when the syndrome results from trauma. The risk of further hemorrhage or nerve damage and operational difficulties are the main disadvantages of surgical exploration. Symptoms completely disappeared in 8 (42.1%) of 19 cases.
Steroid therapy is useful for patients with swelling after a craniofacial fracture. Postma et al report short-term use of dexamethasone (4 mg every 6 hours) for people with a fracture of the zygomaticomaxillary complex, the sphenoid bone. Neurological and ocular symptoms did not appear during the 3-month follow-up.
Patients treated with steroids had a greater chance of neurological recovery than those with observation alone (70% vs 42.1%). The authors currently administer megadose steroid with methylprednisolone (intravenous loading dose of 30 mg/kg followed by 15 mg/kg every 6 hours for 3 days) to reduce swelling that worsens symptoms unless contraindicated to use.
Retroorbital hematoma is one of the reasons. Hemorrhage usually occurs spontaneously between 3 weeks and 4 months.
Surgery
Surgery is indicated when there is significant narrowing of the SOF from a displaced fracture fragment. Four different routes of decompression have been described:
Find out more Enteroviral hand-foot-mouth syndrome in children, adults, prevention and treatment
(1) extranasal intraorbital route, for lateral wall decompression,
(2) modified extranasal intraorbital route with trochlear nerve protection,
(3) extranasal transethmoidal route to decompress the medial wall;
(4) transtemporal route, indicated for suppuration around.
The author's surgical method is direct decompression. When a patient has evidence of a significant depressed wedge fracture with compression in the SOF, a coronal incision is used to approach the affected area.
The narrow canal is decompressed by removing the greater wing of the sphenoid bone, and the temporal lobe is carefully protected. Once adequate decompression has been achieved, the bone flap and zygomatic segment are anatomically laid back and secured using miniplates. After this operation, eyeball movement and sensory function are restored within 3-6 months.
With a facial fracture
Facial fractures associated with superior orbital fissure syndrome are common. Some doctors do not treat a midfacial fracture for fear of further worsening the cranial nerve palsy with surgical reduction.
Others prefer surgery for an associated facial fracture if reduction of the fracture is expected. Patients with an associated facial fracture undergo open reduction an average of 10 days after injury. There are no acute neurological signs after surgical repair.
If the patient experiences decreased visual acuity, orbital apex syndrome should be considered. Treatment of traumatic optic neuropathy (TON) is controversial with varying therapeutic approaches and response rates. Documented visual improvement after a combination of steroid therapy and surgical decompression is 40 – 79%.
Peculiarities
The basis of treatment for trauma-induced disorder is to minimize further irreparable damage to neural structures. Restoration of the fracture and bone anatomy is secondary. The initial observation period is 10-14 days before surgical manipulation of the fracture segments is performed. This prevents the risk of further hemorrhage, involvement of the optic nerve, or damage to others.
What is the treatment?
To reduce the severity of the inflammatory process in neurons, it is recommended to influence the pathogenesis of the disease by taking steroids. The most effective is the use of pulse therapy or high doses of the drugs Prednisolone, Metipred and Methylprednisolone. If a tumor or hematoma is detected in the tissues of the orbit and brain, an operation is performed to excise them, which can slightly improve the patient’s condition. After the cessation of the inflammatory process, the use of neuroprotectors and vitamin-mineral complexes that promote neuronal recovery is indicated.
Ophthalmologists warn that complete elimination of superior orbital fissure syndrome is impossible, and after the cessation of the disease, the patient experiences residual effects.
Forecast
In the absence of compression by fracture fragments, symptoms usually subside over a long period of time, up to 3-4 months. The prognosis may not be as good if symptoms are caused by displaced bone fragments. Recovery of cranial nerves III, IV, VI reaches a plateau approximately 6 months after injury.
Initial steroid therapy (dexamethasone) influences prognosis. Neurological signs and ocular symptoms recover after 3 months of follow-up. The literature on steroid treatment shows that patients treated with steroids have a better chance of neurological recovery than those treated with observation.
Reducing swelling helps to decompress the contents of the fissure and restore neuronal function. Improvement reaches a plateau at the end of 6 months.
Surgery is considered when there is an obvious retrobulbar hematoma with no signs of resolution. The orbital apex is examined using a lateral transconjunctival orbitotomy to remove blood. A CT scan showing obvious bony compression due to a displaced wedge fracture or an orbital blowout fracture with narrowing should prompt surgical decompression to relieve intraorbital pressure.
Superior orbital fissure syndrome: symptoms and treatment
Psychotherapist of the highest category Oleg Viktorovich
43217
Update date: January 2020
The superior orbital fissure is a space just over 20 mm in size, which is located deep in the orbit and borders the wings of the sphenoid bone. This gap plays the role of a connecting cavity between the cranial fossa and the orbit itself.
The orbital cavity is not empty - it is covered by a special film with veins and nerve fibers passing through it. External or internal impact on the cavity can cause superior orbital fissure syndrome.
This process is characterized by damage to the cranial nerves III to VI.
Pathogenesis
It is very difficult to describe the condition of this disease. If you combine in one anesthesia of the upper eyelid, half of the forehead and cornea with full ophthalmology, you can correlate similar parameters. This condition usually occurs when the ophthalmic, abducens, and oculomotor nerves are affected. This, in turn, occurs under various conditions - from a small number of pathologies to mechanical damage.
The main group of causes of this syndrome:
- brain tumor located in the orbital area;
- deviations of the arachnoid membrane of the brain of an inflammatory nature - arachnoiditis;
- meningitis in the area of the superior palpebral fissure;
- orbital injury.
The clinical picture manifested in superior palpebral fissure syndrome is characteristic exclusively of this disease.
Symptoms of the disease:
- ptosis of the upper eyelid;
- paralysis of the eye muscles caused by pathology of the optic nerves – ophthalmoplegia;
- low tactile sensitivity in the cornea and eyelids;
- mydriasis – dilation of the pupil;
- dilated retinal veins;
- inflammation of the cornea in a sluggish state.
- exophthalmos - bulging eyes.
Syndromes are not necessarily fully expressed, sometimes only partially expressed. During diagnosis, this fact is always taken into account. If two or more signs coincide, you should immediately contact an ophthalmologist.
Symptoms for diseases of the orbit
The following symptoms are typical for superior orbital fissure syndrome:
- When the upper eyelid droops, ptosis occurs. The palpebral fissure may close completely or partially.
- As a result of the development of a pathological condition of the oculomotor nerves, paralysis of the eye muscles may occur. This condition is called ophthalmoplegia. A sick person has a lack of motor activity of the eyeball.
- The skin of the eyelids and cornea becomes less sensitive to tactile contact.
- After the lesion, the pupil may dilate (mydriasis). This condition is caused by a decrease in the amount of light, as well as poisoning by chemicals.
- With the syndrome, the retinal veins dilate and changes occur in the arteries.
- As a result of damage to the trigeminal nerve, the cornea becomes inflamed. The process is called neuroparalytic keratitis and is sluggish.
- Sometimes there is the occurrence of bulging eyes - exophthalmos, in which protrusion of the eyeball occurs.
Signs of the syndrome may not be fully identified. It depends on the degree and amount of nerve damage. If the patient experiences two or more alarming signs, it is necessary to urgently visit a doctor for examination.
This disease is compared with other pathologies of the eyes and nervous system. First of all, it is necessary to exclude inflammatory processes in the brain and its membranes, as well as tumors. If meningitis or encephalitis is suspected, a spinal tap is performed. In order to exclude benign neoplasms and cancer, the patient undergoes MRI, CT scan of the brain and X-ray of the skull.
The disease is differentiated from lymphomas, cavernous sinus cysts and its thrombosis. Also, similar symptoms can be observed in systemic pathologies, such as sarcoidosis, orbital myositis, migraines, etc. To make an accurate diagnosis, the patient must be examined by various specialists: an ophthalmologist, a neurologist, a vascular surgeon, an endocrinologist.
- External examination with assessment of the position of the eyeballs in the orbit, their symmetry, mobility and displacement under light pressure with the fingers.
- Carrying out palpation of the outer bony walls of the orbit.
- Exophthalmometry is a procedure that is needed to determine the degree of displacement of the eyeball.
- Ultrasound diagnostics is the detection of changes in the soft tissues of the orbit in the immediate vicinity of the eyeball.
- X-ray, computed tomography, magnetic resonance imaging. These are methods that determine the violation of the integrity of the bone walls of the orbit, foreign bodies in the orbit, and inflammatory changes in the tumor.
These are the main diagnostic methods that are actively used today. A specific diagnostic method should only be prescribed by a qualified specialist.
An upward or downward displacement can occur with injuries, inflammatory processes, tumors, changes in blood vessels in the orbit, as well as endocrine ophthalmopathy. Impaired mobility of the eyeball in certain directions is observed in the same conditions as previous tensions. Swelling of the eyelids, redness of the skin of the eyelids, exophthalmos are observed in inflammatory diseases of the orbit.