This technique of microsurgical intervention was developed and proposed in the mid-80s by the school of the outstanding Soviet ophthalmologist, scientist, surgeon - Academician Svyatoslav Nikolaevich Fedorov (V.I. Kozlov, S.N. Fedorov, 1984-86). Today, despite the relative “youth” (by medical standards) of this technique, the NGSE operation throughout the world has become a kind of canon of surgical correction for open-angle glaucoma.
The immediate surgical field is the so-called area. Schlemm's canal - its posterior wall is removed, the filtering Descemet's membrane (membrane) on the inner surface of the cornea is exposed, due to which the drainage conditions inside the eyeball are significantly improved. In this case, the eyeball itself is not opened, hence the definition of the technique as “non-penetrating”. An important distinctive feature of the NGSE operation is that the hypotensive effect is not abrupt, abrupt, which would be fraught with a number of serious complications; on the contrary, intraocular pressure decreases smoothly and gradually. No less important is the minimally invasive nature of the surgical intervention: the rehabilitation period is only a few days.
At the same time, from the point of view of the technique of execution, the NGSE operation is quite complex and requires highly qualified operating surgeon, therefore, more or less successful attempts have been made in various countries to simplify it methodologically. In addition, the positive effect of non-penetrating deep sclerectomy (as, indeed, any other surgical operation) is also not always sufficiently pronounced and stable, which, on the other hand, serves as a source of further development and an object of constant research in the field of ophthalmic surgery.
The situation has changed significantly with the widespread introduction of the so-called. YAG lasers (diode Nd:YAG lasers). Omitting the technical characteristics of modern quantum generators and not even trying to describe the precision of guidance required for ophthalmic surgery, we will only note that NGSE is now increasingly performed in combination with the subsequent procedure of laser descemetogoniopuncture (LDGP). Its essence is that after some time, from several weeks to several months, after successful non-penetrating sclerectomy, powerful, ultra-precise and vanishingly short (which means “imperceptible and non-traumatic”) laser pulses open microscopic perforations in Descemet’s membrane, which additionally normalize the processes of fluid circulation and drainage. Having all the advantages of the basic operation (according to Fedorov) and the latest ophthalmic laser technologies, such combined treatment in most cases makes it possible to achieve a dramatic, reliable and sustainable hypotensive effect in glaucoma.
The essence of the method
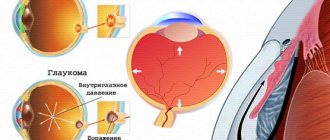
The essence of non-penetrating deep sclerectomy is to create a path for the outflow of intraocular fluid. That is, the goal is to normalize the natural process of fluid exchange, without stress for the organ itself and adjacent tissues. The balance is restored slowly, the intraocular pressure gradually stabilizes - normally it is 10-22 mmHg, and this norm is achieved within the first week.
The outflow of intraocular fluid is restored due to partial removal of the scleral flap. The area up to the circular ligament is affected, which eliminates penetrating effects and injury to the ocular apparatus.
Preparing for surgery
The first step is for the patient to undergo an examination by an ophthalmologist. The doctor will prescribe a comprehensive examination, taking into account the degree of progression of glaucoma and the general condition of the eye system. Before the operation, the following are required: ophthalmoscopy, refractometry, tonometry. Gonioscopy is prescribed to determine the location of glaucoma (main pathological areas). Other studies are indicated and at the discretion of the ophthalmologist.
Before non-penetrating deep sclerectomy, it is necessary to avoid alcohol intake for at least 3-6 days. If there are inflammatory, infectious, bacterial diseases, the first step is therapy with specific medications.
On the day of surgery, it is necessary to exclude physical and emotional stress. The patient should arrive at the clinic in a good mood.
Preparation stage
The preoperative preparation stage involves therapeutic monitoring, as well as laboratory tests in the form of blood and urine tests (general, blood biochemistry, blood sugar tests, drug allergies) and specialized diagnostic eye tests. The latter include:
- Ultrasound;
- tonometry;
- gonioscopy;
- biomicroscopy;
- direct ophthalmoscopy;
- optical coherence tomography;
- electron tonography of the eye.
On the eve of the operation, measures are taken to reduce the risk of further complications. So, on the day before surgery, glycerin diluted with fruit juice or medications that reduce intraocular pressure are prescribed.
How is non-penetrating deep sclerectomy performed?
Non-penetrating deep sclerectomy is performed for all forms of open-angle glaucoma. The technique of this operation does not involve opening the anterior chamber of the eye, so the surgical procedure is minimally invasive.
The outflow of intraocular fluid is restored through the trabecular apparatus. To restore the movement of the liquid substance, Descemet's membrane is exposed, and the outer walls adjacent to Schlemm's canal are removed.
Stages of the operation:
- use of local anesthesia;
- fixing the position of the eyelids;
- surgical incision of the conjunctival membrane of the eye;
- detachment of the conjunctival membrane in the upper segment;
- formation of two flaps;
- partial excision of Schlemm's canal and outer wall;
- suturing the surgical incision;
- applying an aseptic bandage to the eyes.
The duration of eye sclerectomy does not exceed 40 minutes. After surgical treatment, the ophthalmologist talks with the patient, gives recommendations and discharges him home. It is necessary to return for an appointment within a week after surgery. The doctor will measure intraocular pressure and evaluate the effectiveness of the treatment, and, if necessary, prescribe maintenance drug therapy to prevent the risk of relapse of glaucoma.
Non-penetrating hypotensive operations
Description
The main contradiction in glaucoma surgery is the contradiction between the effectiveness and safety of operations. Stronger filtration, while providing and maintaining a hypotensive effect, is fraught with known complications. Slow filtration of aqueous humor is much safer, but the strength and durability of the effect becomes questionable.
Filtering operations distort the hydrodynamics of the eye with a corresponding decline in visual functions. According to TJ Zimmerman et al. (1984), fistulization is associated with the most significant complications of known hypotensive operations.
Recognition of the significant role of morphological changes in the pathogenesis of primary open-angle glaucoma contributed to the development of the so-called “ pathogenetically oriented
» hypotensive operations based on microsurgical changes in the morphology of key elements of the drainage zone of the eye.
Proposals to eliminate intrascleral retention or block of the scleral sinus, removal of juxtacanalicular tissue or part of the trabecular meshwork, despite their speculative nature, led to the development of a number of micro-operations that determined the further direction of glaucoma surgery.
Operations on individual elements of the drainage system of the eye are more precise and much less traumatic compared to fistulization, resulting in a reduced risk of intraoperative and postoperative complications.
Fewer complications and more physiological hydrodynamics after pathogenetically oriented operations contribute to the preservation of visual functions.
Operations during which the anterior chamber of the eye is opened retain “ elements of fistulization”
"(M.L. Krasnov, 1980).
In addition, any “ penetrating
” surgical intervention associated with opening the anterior chamber involves a fairly high likelihood of complications.
Performing a hypotensive operation without penetrating the anterior chamber, that is, a “ non-penetrating operation”
» allows you to expand the indications for surgical treatment of the initial stage of glaucoma, reduce the time of postoperative treatment of patients and carry out surgical treatment of glaucoma on an outpatient basis.
The first microsurgical operation of a non-penetrating type was sinusotomy, which was based on the idea of opening Schlemm’s canal in order to improve the outflow of aqueous humor. In 1972, WM Grant experimentally demonstrated a significant increase in the outflow of intraocular fluid after opening the outer wall of the scleral sinus.
Among the probable mechanisms of action of sinusotomy were noted: filtration through the trabecular meshwork under the conjunctiva, elimination of the intrascleral vascular block and functional block of Schlemm's canal, as well as a possible increase in the permeability of the trabecular meshwork as a result of its stretching or partial damage.
Several options for sinusotomy have been proposed: with opening of Schlemm’s canal “ from the inside to the outside”
"(ab interno), or "
outside in
" (ab externo).
Sinusotomy abіnterno was performed through a traditional conjunctival incision with excision of a strip of sclera above Schlemm's canal, using 2 mm
trephine, or without a conjunctival incision through a short (
3 mm
) radial limbal access after localizing the lumen of Schlemm's canal at its bottom with further dissection of the outer wall of the sinus with scissors under the conjunctiva.
Sinusotomy a b extemo was carried out from a long incision of the limbus concentric to the scleral sinus from the side of the sclera or cornea with oblique tissue dissection and excision of the resulting “visor”. An option without conjunctival incision using a corneal approach has also been described.
One of the conditions for stabilizing the glaucomatous process after surgery is normalization of hydrodynamics. The advantage of sinusotomy was considered to be the preservation of physiological values of tonographic parameters.
Sinusotomy was recognized as a very delicate operation that requires highly qualified surgeons, especially when performing “ tunnel
» option.
The undoubted advantages of sinusotomy attracted the attention of many ophthalmologists, who proposed their own modifications of this operation.
«Sinusotomy under scleral flap
»prevents thinning of the fibrous capsule of the eye in the surgical area, stimulates the outflow of moisture through natural pathways.
One of the essential links in the pathogenesis of open-angle glaucoma is the functional block of Schlemm’s canal. Initially, the collapse of the scleral sinus occurs in the anterior part of Schlemm's canal, subsequently spreading to its posterior part. In order to remove the block of the anterior part of the scleral sinus and improve the outflow through the trabecula B.N. Alekseev and S.F. Pisetskaya (1985) proposed excision of the outer wall of Schlemm’s canal along with a section of tissue from the scleral spur to the line
Schwalbe (“ sinusotomy in the anterior zone of Schlemm’s canal”
"). This operation was intended not only to relieve the blockade of the scleral sinus, but also to free the anterior part of the trabecular meshwork, which is normally functionally less active and therefore less pathologically altered in glaucoma.
Sinusotomy technique (“ externalization of Schlemm’s canal”
"), improved over
20
years, was described as follows:
- wide (
6-8 mm ) conjunctival flap with a base at the limbus; - non-through scleral incisions: a long incision concentric to the limbus
3 mm from it,
2
short incisions from the ends of a long conjunctival flap to the base; - scleral dissection with the formation of a scleral flap with the base towards the cornea;
- localization of Schlemm's canal at the bottom of the formed depression;
- dissection of the outer wall of the canal;
- reposition and fixation of scleral and conjunctival flaps.
The advantages of all developed sinusotomy methods are safety and low trauma, which made it possible to widely use this operation in the initial stages of glaucoma with virtually no risk of vision deterioration.
The widespread use of sinusotomy was limited not only by technical complexity, but also, paradoxically, by its “ pathogenicity”
" The effect of such operations was explained by the elimination of intrascleral retention, which made them indicated only for the intrascleral form of primary open-angle glaucoma.
In real conditions, exclusively intrascleral retention is rarely diagnosed. In addition, with the development of the theory of the functional block of Schlemm's canal and its role in the pathogenesis of glaucoma, the boundary between trabecular and intrascleral forms of retention became arbitrary.
The pathological process in open-angle glaucoma involves the entire drainage zone, especially in the advanced stages of the disease. Therefore, with significant damage to the trabecular apparatus, the hypotensive effect of sinusotomy is reduced. Moreover, even under normal conditions, the inner wall of Schlemm's canal plays an active role in regulating the outflow of intraocular fluid.
To enhance the effect of sinusotomy, a modified technique of JE Gains (1974) was proposed: suturing the scleral spur with a thread that stretches the trabecular apparatus and thus increases its permeability. This technique was complemented by cyclodialysis with cutting out a deep scleral flap and displacing the latter into the suprachoroidal space.
Enhanced filtration can be achieved by suturing the scleral lip of the opened Schlemm's canal with a Z-shaped suture, placing a suture in the area of the Schwalbe ring, or local diathermocoagulation of the tissues of the drainage zone after externalization of the Schlemm's canal: thermotrabeculoretraction or diathermotrabeculospasis. Tissue contraction and subsequent stretching of the trabecula occurs not only at the time of coagulation, but also during subsequent scarring, which provides a more lasting effect.
Another way to increase filtration is to thin the inner wall of Schlemm's canal. « Surgery on the ultrastructures of the inner wall of Schlemm’s canal
"was based on the fact that the main resistance to outflow is localized in the juxtacanalicular tissue. According to the author’s description of the operation, “after excision of the outer wall of the sinus, the endothelium of Schlemm’s canal is removed from the juxtacanalicular tissue (JCT)”; moistening of the scleral sinus bed "indicates the relative preservation of the juxtacanalicular tissue and trabecula." Otherwise, the author recommended a second step: thinning the JCT using forceps or a blade. This “refining” of the trabeculae was continued until sufficient filtration was achieved.
A similar principle was the basis for the “ab-externo trabeculectomy” operation, in which sectoral deep removal of limbal tissue, as well as excision of the JCT and superficial layers of the trabecular meshwork, is performed using a special microdrill.
Further progress in the direction of non-penetrating glaucoma surgery was associated with the development of universal operations involving the maximum number of different mechanisms of action and therefore effective for various forms of glaucoma.
One of these pathways is the activation of uveoscleral outflow. This principle was the basis for deep sclerectomy (DS), which postulated the possibility of drainage directly into the vascular system of the eye through the fenestrated walls of the capillaries of the ciliary body, which reduces unwanted filtration of moisture under the conjunctiva.
This operation is designed to affect all parts of the drainage system of the eye, however, the mechanism of its action includes an element of fistulization, which is probably not auxiliary, but the main one. In essence, deep sclerectomy was a modification of Watson's trabeculectomy.
Based on the GSE operation, non-penetrating deep sclerectomy (NGSE) was developed. The mechanism of action of NGSE is based, according to the authors, on the filtration of aqueous humor through the trabecular apparatus preserved in the surgical area, the permeability of which increases when the outer wall of Schlemm's canal is removed and when the periphery of Descemet's membrane is exposed, with subsequent outflow of fluid into the capillaries of the ciliary body, into the suprachoroidal space and under conjunctiva. A significant reduction in the likelihood of complications and the good health of patients immediately after the intervention shortened the rehabilitation time for patients and made it possible to perform the operation on an outpatient basis.
According to the authors’ concept, the main feature of NGSE is the use of the natural permeability of the peripheral portion of Descemet’s membrane for the outflow of intraocular fluid. The fundamental possibility of filtration through the periphery of Descemet's membrane is indirectly confirmed by the peculiarities of its structure.
Within the belt width 50-150 ?
, lying anterior to Schwalbe’s ring (“zone S”), Descemet’s membrane becomes thinner and disappears, and the posterior corneal epithelium covering it acquires the features of trabecular epithelium: the cells become flattened and probably partially lose their barrier function. On the other hand, to date there have been no experimental data directly confirming the possibility of filtration through Descemet's membrane to a degree sufficient to reduce intraocular pressure.
Moreover, when Descemet’s membrane is exposed over a sufficient length during NGSE, it is clearly visible that all moisture filtration occurs in the space between the scleral spur and Schwalbe’s ring (that is, through the trabecular meshwork), while the periphery of Descemet’s membrane looks dry and impermeable to moisture.
Strengthening filtration after NGSE is facilitated by a number of specific changes in the structure of the drainage zone, achieved sequentially during the operation:
- removal of the outer wall of Schlemm's canal eliminates its functional block - the earliest link in the pathogenesis of open-angle glaucoma;
- removal of deep layers of limbal tissue over the trabecular region lying between the inner wall of Schlemm's canal and Descemet's membrane exposes additional filtering surface. Normally, almost no moisture is filtered through this area (“the non-filtering part of the trabecula”), its pigmentation is minimal, which gives a visual resemblance to Descemet’s membrane;
- if these factors still do not provide sufficient filtration, then, as the authors describe, “the endothelium is removed from the trabecula” to further improve outflow.
- The NGSE operation has found wide clinical application (for example, from 1985 to 1994,
40,000
were performed Eye Microsurgery and, despite technical difficulties, it is becoming increasingly popular. Since 1997, NGSE under the inaccurate name “
deep sclerectomy
” used by foreign ophthalmologists.
The undoubted advantages of NGSE, which definitely increase its effectiveness, are:
- exposure, as a result of the operation, of a much wider filtering membrane than in other non-penetrating operations, consisting not only of the trabecular apparatus, but also of the periphery of Descemet’s membrane,
- creation after removal of a deep scleral flap of an intrascleral cavity that prevents adhesion and scarring of the superficial scleral flap,
- removal of structures responsible for the main share of trabecular retention (endothelium of Schlemm’s canal and JCT),
- possible activation of uveoscleral outflow as a result of providing moisture access to the suprachoroidal space.
- In addition, with NGSE, the possibility of infection is excluded, the percentage of hypotension, choroidal detachment, bleeding is sharply reduced, and the cataractogenic effect is practically eliminated, since peripheral iridectomy is not performed.
- The disadvantages of NGSE are typical of all known non-penetrating operations:
- significantly less effective in advanced and terminal stages of glaucoma,
- instability of the effect in some cases due to deterioration of filtration and excessive scarring,
- inapplicability for closed-angle and narrow-angle forms of glaucoma.
NGSE is typically most effective in the early stages of OAG. At the same time, the percentage of patients with late stages of glaucoma is very high. This determines the need for further improvement of non-penetrating operations in order to increase their effectiveness in advanced and advanced glaucoma.
A reflection of this need is the use of cytostatic drugs, as well as hydrogel or collagen drainages. The benefit of these measures in reducing scarring is undoubted, although clinical studies indicate that the presence of allodrainage has virtually no effect on the effect of non-penetrating operations: the frequency of relapses after NGSE and NGSE with drainage is almost the same, although many studies in recent years indicate the opposite.
Despite quite successful widespread use and undoubted advantages, non-penetrating hypotensive operations have not yet become the basis of glaucoma surgery. Among the reasons for the slow implementation are technical complexity, insufficient hypotensive effect, and ambiguity in the interpretation of the mechanisms of postoperative decrease in ophthalmotonus.
This is based on the lack of complete clarity of the morphological basis of non-penetrating glaucoma surgery. Analysis of the literature data obliges us to raise the question of the probable morphological heterogeneity of the trabecular apparatus and the advisability of clarifying its topography.
Single reports on the morphology and topography of the drainage zone of the eye after hypotensive operations concerned mainly fistulizing interventions. A similar aspect of non-penetrating surgery has been discussed largely speculatively. Special morphological studies of non-penetrating operations (also isolated) were aimed mainly at studying the dynamics of reparative processes.
The lack of a clear concept of topographic histology of the drainage zone of the eye leads to the fact that the trabecular apparatus is perceived by surgeons as a relatively homogeneous “ membrane
", "
film
", but not as a multilayer structure - an object of precise, predictable, topographically oriented surgery.
In any surgical specialty, knowledge of the topography (surgical anatomy) of the object of operation is absolutely necessary. As long as the object of glaucoma surgery was the drainage zone as a whole (the period of fistulizing operations), the topography of the various parts of the trabecular meshwork did not play a significant practical role.
With the transfer of operations to the histological level, when micron-sized structures are subject to operations, the trabecular apparatus becomes something more than just a “ membrane”
"or "
diaphragm
".
The area of 50x300
microns (cross-section of the trabecular meshwork) becomes a fairly large field for subtle and varied surgical manipulations.
At the same time, knowledge of the topography of the drainage zone of the eye at the histological level - “ histotopography”
"- becomes absolutely necessary, and operations developed on the basis of the histo-topographic approach become much more understandable, feasible and predictable.
Article from the book: Microsurgical anatomy of the eye drainage system | Zolotarev A.V..
Rehabilitation
After non-penetrating deep sclerectomy, it is necessary to follow a postoperative anti-inflammatory therapy regimen. A regimen with limited physical activity and limited visual stress for a week is recommended in order to prevent possible overstrain and achieve a maximum reduction in intraocular pressure.
During the recovery period, you should take antibacterial drugs and anti-inflammatory drugs - they are prescribed by the doctor individually (these can be non-steroidal or steroid drugs).
Typically, the rehabilitation period is easy, without complications and does not require significant effort from the patient.
Operation efficiency
The benefits of sclerectomy depend on the technique chosen. Mainly these include:
- effective reduction of intraocular pressure;
- duration of the operation;
- duration of rehabilitation.
The non-penetrating method is characterized by:
- minimally invasive nature (slightly traumatic process);
- a minimum list of restrictions in the postoperative period;
- reduced risk of complications (compared to penetrating techniques).
In most cases, surgery helps achieve your goals. And depending on the qualifications of the surgeon, it is possible to minimize the risk of any negative consequences. The effectiveness of the operation increases with the use of lasers, which avoid deep tissue damage. The following types of laser are used for this:
- excimer;
- argon;
- solid state laser.
The actual effectiveness of surgery, like any antiglaucomatous type of surgery, can be assessed after a year. So, if at the end of this period the level of intraocular pressure remains stable and remains within the normal range, then the operation was successful.
Non-penetrating deep sclerectomy at the Ophthalmic Surgery Center ON CLINIC
The Ophthalmic Surgery Center ON CLINIC successfully uses the method of non-penetrating deep sclerectomy to treat glaucoma and normalize intraocular pressure. Surgical operations are performed by experienced ophthalmologist-surgeons, doctors of the highest category, candidates and doctors of science. The excellent equipment of the Ophthalmic Surgery Center allows doctors to conduct a wide range of preoperative examinations, obtain reliable diagnostic data and monitor the clinical situation using high-precision research methods.
Operating equipment with expert class ophthalmological multisystems. This allows treatment of any complexity, ensuring the achievement of the desired clinical result.
If you or your loved ones have glaucoma or there are signs of its development, make an appointment with the specialists of the Ophthalmic Surgery Center! Doctors pay special attention to your health, taking all measures to relieve dangerous syndromes, reduce the risk of glaucomocyctic crisis and preserve vision!
Trust your vision to professionals - contact experienced doctors at ON CLINIC!
Diagnosis of glaucoma
To make a diagnosis of glaucoma and determine the method of treatment for glaucoma, a thorough diagnostic examination is necessary, which should include:
- visometry (determining visual acuity)
- refractometry (determining the optical power of the eye - refraction)
- perimetry (determining peripheral vision)
- tonometry (determination of intraocular pressure)
- biometrics (determining the depth of the anterior chamber, lens thickness, eye length)
- biomicroscopy (examination of tissues and media of the eye using a slit lamp)
- gonioscopy (study of the structure of the anterior chamber angle)
- ophthalmoscopy (examination of the fundus with assessment of the condition of the optic nerve and retina)