Treatment of glaucoma with a laser is carried out if conservative therapy is already useless, and the risk of irreversible deterioration of visual functions due to constant exacerbations of the pathology increases. The decision to prescribe laser surgery is made by the doctor after a comprehensive examination of the patient.
In this article
- What is glaucoma?
- Symptoms of glaucoma
- Diagnosis of glaucoma
- Glaucoma Treatment Methods
- Who is suitable for laser eye surgery for glaucoma?
- Features of trabeculoplasty
- Postoperative period
- Laser iridectomy
- Recovery after iridectomy
- What should you not do after surgery?
What is glaucoma?
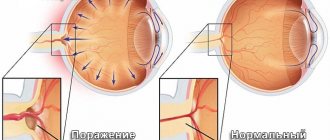
Glaucoma is a chronic ophthalmological disease characterized by damage to the optic nerve, which is caused by increased intraocular pressure. This disease provokes a severe decrease in visual acuity. At the same time, the pathology progresses very quickly. If left untreated, a person may go blind.
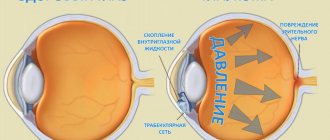
At the front of the eyeball there is a small cavity between the cornea and the lens. This cavity is called the anterior chamber. A clear liquid circulates in it, which nourishes the tissues of the eye. If this fluid leaves the anterior chamber very slowly and begins to accumulate, the pressure in the eye increases. Subsequently, constant surges in intraocular pressure can lead to severe damage to the optic nerve and other ocular structures. The optic nerve performs one of the most important functions in the process of vision. Any pathology affecting this part of the eye is accompanied by a decrease in visual abilities.
What types of glaucoma are there?
Speaking about the types of glaucoma, first you need to understand how fluid normally circulates inside the eye.
Intraocular fluid is secreted by the processes of the ciliary body, then the fluid penetrates through the pupil into the anterior chamber of the eye and is directed to the angle of the anterior chamber. This angle is formed by the posterior surface of the cornea and the anterior surface of the iris. At the top of this angle there is a drainage system consisting of a trabecular network (a kind of filter that promotes the one-way movement of moisture) and the Helmet Canal. The fluid, filtered through the trabecular meshwork, enters the Shlemov canal, then through the collector vessels connected to it into the external veins, within which it flows out of the eye.
The described outflow path is the main one; about 80-90% of the intraocular fluid flows out of the eye through it.
Depending on the anatomy of the anterior chamber angle, the following types of glaucoma are distinguished:
- Primary open-angle glaucoma (POAG) is the most common type of glaucoma, which is characterized by increased intraocular pressure (IOP) and optic nerve atrophy due to progressive death of nerve fibers. In this case, the angle of the anterior chamber is open.
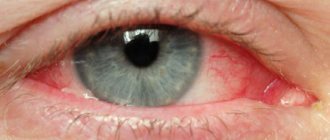
- Narrow-angle (and angle-closure) glaucoma occurs when there is an anatomically narrow angle of the anterior chamber of the eye, which impedes the outflow of intraocular fluid to the drainage system of the eye. Under some circumstances (for example, natural dilation of the pupil in the dark, or drug dilation of the pupil during a diagnostic examination), the drainage system may be completely blocked by the root of the iris. An acute attack of glaucoma develops, accompanied by a sharp critical increase in IOP, severe pain in the eye, headache on the affected side, sudden deterioration of vision (blurred image, the appearance of iridescent halos in front of the eyes), redness of the eye. This condition threatens rapid vision loss and requires urgent assistance.
There are also the following types of glaucoma:
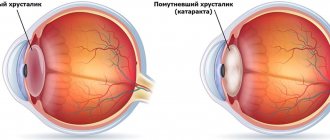
- Secondary glaucoma - develops as a result of eye injury, inflammation in the eye, cataracts, tumors, caused by long-term use of medications (corticosteroids); in rare cases, eye surgery for another disease can trigger the development of glaucoma.
- Normal or low pressure glaucoma - this form of glaucoma is characterized by progressive atrophy of the optic nerve with IOP values within the normal range (the reason for the development of this type of glaucoma is unknown, the theory of impaired blood circulation of the optic nerve is being considered).
There are other types of glaucoma depending on age and course of the disease.
Symptoms of glaucoma
Glaucoma occurs in different forms (depending on the causes that caused it), each of which has its own symptoms. Open-angle glaucoma develops almost asymptomatically. The disease at this stage is very difficult to detect, since almost nothing bothers the patient and he does not consult an ophthalmologist. When the disease progresses to the next stages, a person begins to notice its symptoms.
First, peripheral vision disappears, it becomes “tunnel” (as through a telescope). This happens gradually, so the patient often does not attach any importance to this, explaining the deterioration in lateral perception by ordinary fatigue. Because of this, the disease continues to progress, which leads to decreased vision in poor lighting conditions, rainbow circles appearing before the eyes, and headaches. Jumps in intraocular pressure are accompanied by pain in the visual organs and in the forehead, general malaise, nausea and vomiting. No matter what form glaucoma occurs, it always causes a decrease in visual acuity. If you notice at least one of the above signs, be sure to consult an ophthalmologist.
Diagnosis of glaucoma
This pathology must be identified at an early stage for its effective treatment. This is difficult to do, since at the initial stage the disease does not have clearly defined symptoms. The causes of glaucoma are factors such as tobacco smoking, mechanical injuries to the eye, including burns, genetic predisposition, and myopia. If you are at risk, you must visit an ophthalmologist at least once a year (to measure pressure and check the general condition of the eyes. Glaucoma also often affects the visual organs of people over 35 years of age. After reaching this age, it is advisable for a person to measure intraocular pressure at least once per year.Over the age of 55, ophthalmologists recommend measuring the pressure of the fluid inside the eye at least twice a year.
Several methods are used to diagnose glaucoma:
- perimetry to check visual fields;
- ophthalmoscopy and biomicroscopy, which make it possible to examine the fundus of the eye;
- Ultrasound of the visual organs;
- gonioscopy (visual examination of the anterior chamber of the eye);
- measurement of intraocular pressure.
These examination methods help not only to identify pathology, but also to determine its form and stage.
Comprehensive examination for glaucoma
We use optical coherence tomography (OCT) for diagnosis. With this test, the doctor takes an image of the retina and optic nerve. He can verify the presence or absence of pathological changes characteristic of glaucoma. OCT is also indispensable for monitoring the progress of treatment and determining the stage of the disease.
During the diagnostic process, pachymetry is performed: measuring the thickness of the cornea. The results of this study allow for more accurate interpretation of previously obtained intraocular pressure figures. People with thick corneas are often diagnosed with increased intraocular pressure, which does not pose any danger to them. On the other hand, high intraocular pressure in combination with a thinning cornea can be an additional “alarm bell” indicating glaucoma.
Computer perimetry, which is carried out in our clinic, ideally complements OCT data. If OCT gives the doctor an idea of the anatomical structure of the retina and optic nerve (thickness and density of nerve fibers, etc.), then computer perimetry represents the functional state of the retina. The doctor can understand how retinal cells react to light. Is the retina capable of fully performing its functions, providing a person with excellent vision?
Fortunately, in the initial stages of glaucoma, computer perimetry often shows the absence of any functional changes in the organ of vision. Or these changes are minor. This means that by learning about glaucoma early, we can best fight it.
Also in the diagnostic process, biomicroscopy (examination of the fundus under a microscope) and gonioscopy (examination under a microscope of the condition of the drainage tracts located in the anterior chamber of the eye) are used. As mentioned above, with glaucoma problems inevitably arise with the outflow of intraocular fluid. With the help of gonioscopy we can get an accurate picture of this process.
Who is suitable for laser eye surgery for glaucoma?
Indications for laser procedure for glaucoma:
- first and second stages of open-angle and closed-angle (acute) glaucoma;
- inability to reduce intraocular pressure and eliminate other symptoms of glaucoma using conservative therapy;
- allergic reactions to eye drops used to reduce pressure in the eye;
- when the patient cannot regularly take drops and tablets;
- as a prevention of damage to the second organ of vision, which does not have glaucoma.
The operation may be contraindicated for diabetic retinopathy, swelling and clouding of the cornea, and inflammatory processes in the eyeball. Also, the laser procedure is not used if the anterior chamber of the eye is very small.
The patient undergoes an examination before the operation, and in each specific case the decision to carry out the procedure is made by the doctor. He also chooses the type of laser surgery for glaucoma. There are two of them: trabeculoplasty and iridectomy.
Laser treatment of glaucoma. Reviews from doctors
To summarize, we can say that laser treatment of glaucoma today has no analogues in the world. Laser treatment of glaucoma when drug antihypertensive therapy was ineffective allowed many patients to preserve their vision, avoid antiglaucomatous surgery, and returned them to a full life.
But despite the obvious advantages, using a laser also has a number of disadvantages:
- low efficiency and short duration of the hypotensive effect in advanced stages of glaucoma;
- the possibility of a reactive syndrome, accompanied by an increase in intraocular pressure in the first hours after laser intervention and with the development of an inflammatory process in the future;
- the possibility of damage to corneal endothelial cells, lens capsule and iris vessels;
- formation of scar adhesions in the area of impact - the angle of the anterior chamber, the iridectomy zone.
Laser treatment of glaucoma is effective only in the early stages of glaucoma development. In advanced and terminal stages of the glaucomatous process, laser treatment is no longer indicated due to the low hypotensive effect. We are ready to offer this category of patients an alternative to laser treatment – microsurgical treatment of glaucoma.
Features of trabeculoplasty
The essence of the operation is as follows: the doctor uses a laser beam to apply about 40-60 pinpoint microscopic burns to the tubular diaphragm of the eye. The trabecular diaphragm is an integral part of the drainage system of the organ of vision, through which the outflow of ocular fluid from the anterior chamber occurs. The doctor determines how many burns (holes) to make during surgery by monitoring the decrease in intraocular pressure.
Before the procedure, the patient is given local anesthesia and a goniolens, which ensures reflection of the laser and protection of eye tissue. There are two types of trabeculoplasty, which differ in the type of laser used in the operation: selective and argon. Selective laser surgery is more gentle. The doctor acts selectively on eye cells, which leads to less injury to the cornea. This procedure can be used more than once.
The argon laser technique has a greater impact on the eye. The laser used in this operation is more powerful. After laser treatment, it will take longer to recover. This procedure is not prescribed more than once. Afterward, surgery may be required to remove scar tissue. Trabeculoplasty lasts about 30 minutes. After laser surgery, the surgeon prescribes a course of therapy, including antibacterial drops, vitamins, antiglaucomatous medications and drugs to reduce the production of fluid inside the eye.
Method of laser trabeculoplasty
The procedure is performed on an outpatient basis, local anesthesia, drip. A rather complex optical system is placed on the surface of the cornea, which ensures (when using the currently widespread linear version of trabeculoplasty) the application of pulsed photon “injections” to the area of Schlemm’s canal along one line.
One of the generally accepted standards in the treatment of glaucoma today is argon laser trabeculoplasty, developed in the late 70s by Wise and Witter. Laser coagulation provides shortening and the necessary tension of the trabecular screed, an increase in drainage ducts and, ultimately, reduces the pressure of the intraocular fluid by improving its circulation and outflow. In addition, the argon laser version of trabeculoplasty increases the permeability of the trabecular membrane and helps clear it of pigment granulation.
It is obvious that the widespread use of argon laser modification of the trabeculoplasty method is due, first of all, to its effectiveness: according to clinical and statistical studies, stable (for a period of at least 5 years) normalization of intraocular pressure is ensured in half of the cases, another 30% of patients receive relief in period of 10 years or more.
At the same time, the technique using an argon laser is not universal and is indicated for a limited category of patients, distinguished by certain individual characteristics of the structure of the eye tissues. The fact is that the photon flux of the argon generator is absorbed mainly by pigment cells, i.e. high effectiveness of exposure is possible only under the condition of intense pigmentation of the trabecular membrane and Schlemm's canal. In addition, argon laser radiation promotes the formation of scar tissue, and repeated use of such a laser is especially undesirable - even if it is clinically indicated, in practice, repeated intervention can only worsen the course of glaucoma. The actual effectiveness of a repeated argon laser procedure is slightly higher than 30%.
Significant postoperative risks should also be taken into account: approximately every third patient experiences a reaction in the form of a “burst” of intraocular pressure in the first hours after surgery, and every fiftieth patient experiences this effect within the first three weeks.
The disadvantages of argon laser trabeculoplasty also include high cost (which naturally affects the costs of patients) and the large size of the argon generator, low wear resistance and a relatively short service life.
Considering the above-mentioned disadvantages of this effective and generally promising technique, at this stage an intensive search for new technological and methodological solutions for trabeculoplastic treatment of open-angle glaucoma continues.
Postoperative period
In the first four hours after trabeculoplasty, intraocular pressure may jump sharply, but it quickly stabilizes. The eye may also become very sensitive to light immediately after surgery. This phenomenon is temporary. It is better to wear sunglasses when going outside for several days. The operated patient must carefully monitor eye hygiene throughout the month. Under no circumstances should you rub them, as you can damage the cornea or cause an infection in the eye. There may also be side effects/complications. They appear as:
- excessive formation of scar tissue in the area of the anterior chamber;
- decreased visual acuity and blurred vision;
- painful sensations in the eyes;
- formations between the iris and cornea of adhesions, which will require another operation;
- infectious and inflammatory eye diseases (keratitis, blepharitis, conjunctivitis);
- allergies, manifested in redness of the sclera, irritation, itching, burning in the eyes (an allergic reaction can occur to components of anesthesia).
Any of these symptoms should raise alarm and be a reason to visit the clinic. Trabeculoplasty is very effective in the treatment of glaucoma, it prevents its further progression and is rarely accompanied by complications. However, the method also has a disadvantage - after a few years, in about 50% of cases, attacks of increased intraocular pressure occur again. Further treatment of glaucoma can only be continued with surgical methods.
Cost of services
Glaucoma examination
Name of service
Cost, rub. )
Consultation and examination for glaucoma
Includes:
- autorefractometry
- determination of visual acuity
- intraocular pressure measurement
- fundus examination
- perimetry
- optical tomography of the optic nerve and macula
5400
Additional payment for consultation with surgeon, professor, MD Trubilin V.N.
3000
Additional payment for consultation with a surgeon, Ph.D.
2000
Surgeries for glaucoma
Name of service
Laser iridectomy
It helps to establish normal communication between the anterior and posterior chambers of the eye, thereby normalizing the circulation of intraocular fluid. The operation proceeds as follows: miotics - drops to constrict the pupil - and anesthetic drops are instilled into the patient's eyes. After this, a goniolens is installed on the eye to focus the laser beam. Next, the doctor burns a hole in the iris, allowing the outflow of intraocular fluid. Iridectomy helps with severe glaucoma with frequent attacks of increased pressure in the eye.
This laser surgery has a number of advantages:
- ambulatory treatment;
- pressure in the eye decreases instantly;
- use only local anesthetics;
- formation of natural outflow of fluid in the eye;
- relatively low cost.
Trabeculoplasty is also done on an outpatient basis, but iridectomy is superior to this technique and is more effective.
Minimally invasive surgery “according to the original method” of Professor Trubilin
With non-penetrating deep sclerectomy (NGSE), the wall of the Schlemova canal is exposed and the surgeon gains access to the trabecula, i.e. to the drainage system of the eye. The eyeball is not opened; surgery occurs exclusively in the drainage system of the eye. This is an effective, minimally invasive intervention with an extremely low risk of postoperative complications.
Professor V.N. Trubilin modernized this operation. He developed an original method of installing drainage made of collagen, a material that does not cause rejection or an allergic reaction. The drainage is a mesh plate resembling a labyrinth. Through this “labyrinth”, excess intraocular fluid flows under the choroid, where it is absorbed by the vessels. The retina and optic nerve are released from the pressure of this fluid, which is the purpose of the operation.
In most cases, this operation is the most effective and appropriate for patients with glaucoma. In rare situations when NGSE cannot be performed, another operation is performed at the Professor Trubilin Clinic - sinustrabeculectomy (STE). This is a penetrating operation that has the same goals as NGSE - to ensure the outflow of intraocular fluid and reduce intraocular pressure.
Phacoemulsification of cataracts for patients with glaucoma
For patients with glaucoma who require phacoemulsification of cataracts, our clinic offers surgery using the original method of Professor V.N. Trubilin - “Phacoemulsification of cataracts and trabeculoplasty Ab interno” (from the inside). During this surgical intervention, the surgeon not only implants an artificial lens in the patient, but also flushes the drainage paths and breaks the pathological adhesions that impede the outflow of intraocular fluid. Just like NGSE and STE, this operation provides an effective reduction in intraocular pressure.
What should you not do after surgery?
To avoid complications, the person operated on after iridectomy is strictly prohibited from:
- reading, using gadgets, etc.;
- rub, scratch your eyes and eyelids (you can injure the cornea or cause an infection);
- sleep lying on the side of the eye that has undergone laser treatment;
- wash your hair (the first 2-3 days after the procedure);
- visit the swimming pool, bathhouse, sauna;
- play sports (we are not talking about morning exercises or a light jog, but about intensive training, including strength training);
- There are foods that provoke fluid stagnation in the body (dried, salted, pickled).
The doctor will prescribe you a regimen that must be strictly followed. This way you will save yourself from unpleasant consequences. They are as follows:
- fusion of corneal tissues in holes created with a laser;
- too large an artificial hole can lead to poor vision;
- a sharp increase in pressure in the eye;
- lack of the desired result (in this case, other treatment methods are used).
Do not use eye drops without a prescription and do not self-medicate if side effects begin to occur. If you experience any discomfort, do not delay visiting an ophthalmologist.