Dacryocystitis is inflammation of the lacrimal sac. A small pouch is located in the inner corner of the eye.
Tears drain into it from the organ of vision and then pass through the nasolacrimal ducts (often called tear ducts) and into the nose.
In children suffering from dacryocystitis, tears do not drain; they accumulate in the eye, block the canal, and allow bacteria to actively multiply, which leads to infection.
Blocked tear ducts often open on their own without treatment. However, if it occurs more than once, your child's doctor may use a surgical probe and irrigation to open the tear ducts.
Causes of tear duct blockage in infants
The cause of the disease in an infant is a gelatinous film located in the nasolacrimal duct . When the fetus is in the womb, this plug protects the visual organs from the penetration of amniotic fluid. At birth it is torn. If this does not happen, the tear accumulates and stagnates, leading to the development of an infectious process.
There are other reasons associated with developmental anomalies:
- violation of the facial structure in certain genetic diseases;
- tumors of the face, nose, or cysts in the duct;
- anomalies in the structure of the eyelids and facial skull;
- narrow tear duct.
The cause of blockage in a baby is the entry of foreign bodies into the tear ducts. For example, cosmetics, dust. The disease develops with fractures of the nose, bone walls of the orbit and eyeball. Injury to the nasolacrimal duct often occurs when it is probed or washed.
The structure of the nasolacrimal duct in a newborn baby
Tear fluid performs several important functions:
- Protects the eye from drying out;
- Participates in the refraction of light;
- Forms the tear film;
- Nourishes the cornea.
Tears are produced by a gland located in the lacrimal fossa at the upper outer edge of the eye socket. First, it enters the conjunctival cavity, and then, along the lacrimal canaliculi, into the lacrimal sac, located near the inner corner of the eye. Excess tears exit through the nasolacrimal duct into the nasopharynx.
In newborns, the nasal canal is relatively short - only 8 mm , while in adults the length of the canal ranges from 14 to 15 mm. This creates favorable conditions for infectious agents to enter the lacrimal sac. In addition, the lacrimal canal in newborns is underdeveloped, which also contributes to the invasion (penetration) of microorganisms.
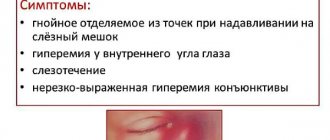
Symptoms of dacryocystitis
The main symptoms of the disease are excessive tearing, even when the baby is not crying - this is called epiphora. The rupture is accompanied by redness in the inner corner of the eye, irritation, swelling, or a bump on the side of the nose.
If treatment is not started promptly, hyperemia spreads to other parts of the eye. These signs are accompanied by an increase in body temperature, and a fever often occurs.
We recommend reading: Obstruction of the lacrimal duct
Another sign of dacryocystitis in a baby is pus or mucus collecting in the corner of the eye. The child wakes up with a crust over the eyelid or in the eyelashes, which blinds them. When you gently press on the bag, a mucopurulent liquid appears from it.
If dacryocystitis is confused with conjunctivitis or the infant is self-medicated, this sign may be blurred . Therapy for inflammation of the connective membrane eliminates signs of obstruction of the nasolacrimal duct , but does not remove the cause of the pathology. This leads to relapse of the disease.
The disease can be unilateral or bilateral. Most often one visual organ is affected.
Obstruction of the lacrimal duct in a full-term baby appears in the first 24–48 hours after birth, in premature babies a little later - at 2–3 months of life . This is due to continued development and bone formation outside the womb until the normal 40 weeks.
Mechanism of obstruction formation
The entire period of intrauterine development, the nasolacrimal canal is covered with a thin film, which prevents amniotic fluid from entering the nasopharynx. However, as the baby passes through the birth canal or with the first cry, this film breaks and frees the entrance to the nasolacrimal canal. If this does not happen, dacryocystitis develops - inflammation of the lacrimal canal caused by fluid stagnation.
The first sign of obstruction of the lacrimal canal in an infant is increased tear production. If in the first weeks after birth the patency of the canal is not restored, infectious agents (viruses or bacteria) penetrate into the lacrimal sac and purulent inflammation develops.
In some babies, the tear film may rupture on its own within the first six months to a year . This is due to the growth and expansion of the nasolacrimal ducts, as a result of which the film stretches and ruptures on its own. All this time, the child should be under close supervision of an ophthalmologist. If all medical recommendations are correctly followed, inflammation of the lacrimal sac can be avoided.
Which doctor should I contact?
Dacryocystitis is treated by an ophthalmologist . If your child has no signs of infection, you can consult your pediatrician. The doctor will look to see if dacryocystitis is the cause, as early treatment will prevent the need for surgery.
If signs of infection are present (redness, swelling, discharge of pus), you should not delay a visit to the ophthalmologist. The infection may spread to other parts of the face and lead to an abscess.
If necessary, parents receive advice from an ENT doctor and surgeon.
Diagnostics
Only an ophthalmologist can diagnose the disease in an infant. The presence of a blockage is determined by instilling a dye solution - fluorescein or collagengol. The Vesta test is performed. The bag is pre-cleaned by squeezing, then washed with a 2% boric acid solution.
After which the ophthalmologist instills the dye. If the tubular function is normal, a colored fluid will appear in the lacrimal punctum.
The second stage of the Vesta test is to determine the amount of dye on the swab in the nose. Normally, it should come out within 5 minutes from the moment the drops are instilled.
If the ophthalmologist deems it necessary, he will give a referral for a computed tomography scan. It allows you to collect data about the sac, nasolacrimal duct and intranasal features of the baby. A CT scan is performed if the tear duct has not opened and the cause remains unknown.
Treatment
Therapy for an infant involves three options - conservative methods, expectant management and surgery . Initially, doctors wait until the canal opens on its own. Anti-inflammatory drugs are prescribed that help prevent the purulent process.
If this does not happen, conservative methods are used - medications and massage. Combining these techniques can significantly speed up the healing process.
Medicines
Treatment with medications is recommended to be carried out inpatiently, under the supervision of a general practitioner or ophthalmologist. This will reduce the risk of complications.
The first stage is a massage to remove excess mucopurulent discharge. The second stage is the use of antibacterial drops. Children are prescribed Levomycetin or Tetracycline.
We recommend reading: Tetracycline ointment for children
The duration of treatment is 2 weeks. If dacryocystitis is not cured, surgery is prescribed.
For the purpose of disinfection, chamomile decoction, Furacilin solution or Ophthalmodec drops are prescribed. They wash the baby's eyes 2-3 times a day . All pharmacological agents are prescribed by the doctor, who also prescribes the dosage and number of uses.
Massage
Using massage movements, knead the film that prevents the outflow of tear fluid. Massaging the tear duct is painless and involves a series of simple steps.
Before handling, wash your hands thoroughly with soap. Do not put pressure on the eyeball. Only the corners and lacrimal punctum are massaged.
The baby twists and cries. He’s not in pain, he just doesn’t understand what’s happening to him, so he reacts as a baby should.
Surgical intervention
The surgical technique is the most effective in treating obstruction of the lacrimal canal. According to statistics, the main percentage of recovery comes from surgery performed at the age of 2–3 months.
Probing allows you to restore the patency of the nasolacrimal duct. The operation is performed in a hospital setting by a qualified doctor. Probing is not performed if the lacrimal canal is clogged in a child who is under 1 month old.
After the procedure, the child can be taken home immediately. Algorithm of actions:
- local or general anesthesia;
- a microscopic Bowman probe is inserted into the lacrimal punctum;
- he pops the plug;
- the lacrimal canals are washed with an antiseptic solution.
If the procedure is successful, the solution pours out through the nose or enters the nasopharynx. This can be understood by the baby’s swallowing reflex.
After the procedure, the child is prescribed antibiotics and decongestants. Massaging is required for 10 days. Massage prevents stagnation of tear fluid.
Symptoms of obstruction
Obstruction of the nasolacrimal duct can be detected in the maternity hospital. However, in most cases, this problem makes itself felt much later.
The very first sign of the disease is the appearance of causeless lacrimation in the baby . Moreover, it can be either unilateral or bilateral (in the case of simultaneous damage to both eyes).
Some time after tears appear, the eye begins to turn red and dacryocystitis develops. In this case, stagnation of tear fluid is formed, which is a favorable condition for the attachment of bacteria and their further reproduction.
Purulent discharge appears, which may be accompanied by sticking of eyelashes and an increase in temperature. Typically, the causative agents of dacryocystitis are streptococci, Escherichia coli, staphylococci, and, less commonly, chlamydia and gonococci.
Sometimes these symptoms are mistaken for neonatal conjunctivitis. However, conjunctivitis, unlike dacryocystitis, often has bilateral localization. In addition, there are a number of other diagnostic signs that help differentiate these conditions. More details about them are described in the “Diagnostics” section.
When pressing on the lacrimal sac, drops of cloudy purulent liquid are released from the lacrimal openings. The largest amount of such discharge is observed after the baby wakes up or during strong crying.
As dacryocystitis progresses, ectasia of the lacrimal sac occurs - its stretching and increase in volume. At the same time, the skin over it is hyperemic (red) and sharply stretched. In particularly advanced cases, the bag can reach the size of a ripe cherry.
Overstretching of the mucous membrane of the lacrimal sac leads to its atrophy and inability to produce mucous secretion.
Recommendations for parents
Constant lacrimation and redness of the eye should alert parents. Dacryocystitis may resolve spontaneously within 2–3 months, but the disease should not be ignored. Timely adoption of measures will protect the baby from surgical intervention.
The child must be shown to a doctor, do not take independent measures, and especially not massage the lacrimal openings if you do not have the appropriate skills and the doctor has not shown you how to do it correctly.
If there is obstruction of the tear ducts, the ophthalmologist will prescribe treatment. It will prevent the spread of infection and the development of such complications:
- cellulite;
- inflammation of the eye tissue located behind the orbital septum;
- infectious brain damage;
- blood poisoning.
Eye drops should be instilled strictly according to the instructions. Before use, wash your hands and clear the child’s eyes of accumulated secretions.
If the eye turns sour in the morning and crusts form after sleep , do not peel them off. It is necessary to treat with an antiseptic solution, slightly soak and only then carefully remove the crusts.
Useful video
Probing for dacryocystitis in infants under mask anesthesia:
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
Treatment of congenital dacryocystitis
In a baby, the tear duct is narrow, but as the baby grows, the lumen of the canal increases, and the clogging embryonic membrane stretches. Therefore, over time, it may burst on its own. This usually occurs in the first 6 months of life. You can help it break by giving your baby a special massage. And medicinal solutions will help prevent or eliminate suppuration. If it was not possible to open the lacrimal canal, the child is advised to probe (bougienage) the duct. If this procedure is done late (after 6 months), the membrane will become denser, which will worsen the result of the procedure.
Massage
Treatment of dacryocystitis in newborns begins with massage of the lacrimal canal. During massage, pressure increases inside the tear duct. This contributes to the natural breakthrough of the embryonic membrane and rid the baby of the problem.
Technique:
- Wash your hands with soap and dry, keep your nails cut;
- Place your index finger on the inner corner of the baby's eye with the tip pointing toward the bridge of the nose;
- Lightly press on this point and, without releasing the pressure, move your finger down along the nose;
- Repeat steps 2-3 5 to 10 times. If at the same time pus or clear liquid is released, then you have done a high-quality massage;
- Remove the pus using chamomile decoction and a cotton swab and apply anti-inflammatory or antiseptic drops, which will be prescribed to you at your appointment with your doctor.
What is probing
For dacryocystitis in newborns, treatment in the form of massage and removal of pus, or instilling anti-inflammatory drops into them may not be enough. What to do if the problem persists by 6 months? Then the only way to cope with the congenital pathology is to probe the lacrimal canal.
Probing (another name is bougienage) of the lacrimal duct is an instrumental procedure aimed at breaking the clogging membrane by introducing a special metal probe into the canal. It looks scary in appearance, but all manipulations are performed either under general anesthesia or local anesthesia. Therefore, there is no need to worry about the child being in pain. Even crying during the procedure should not alarm you: no one will like to lie in a fixed position when there is additionally, albeit painlessly, the sensation of a foreign body in the area of the eye and nose. The baby has no other ways of expressing dissatisfaction.
After probing, dacryocystitis in children usually goes away. But there is a risk of the formation of adhesions (fusion of injured tissues), which will cause a relapse of the disease. Then all the manipulations will have to be repeated. To avoid adhesions, the child is given antibacterial drops immediately after surgery. They prevent inflammation and reduce the risk of adhesions. Drops for preventive purposes should be instilled into the eye for 1-2 weeks.
Drugs prescribed for dacryocystitis
It is not possible to treat dacryocystitis with drugs alone, since they do not break through the embryonic membrane. Drops only help cope with rapidly developing pathogenic microflora caused by stagnation of tear fluid. However, their use is necessary to eliminate the symptoms of inflammation, but you will notice the effect only if you use them in conjunction with massage or after probing the canal.
Before instilling the drops, rinse your child's eyes to remove any accumulated pus. A decoction of chamomile, physiological or furacillin solution is suitable for this. Use cotton pads, but not plain cotton wool or bandages - they leave lint on the surface of the eyes and cause irritation.
For dacryocystitis, children are prescribed one of the following drugs:
- Vigamox;
- Tobrex;
- Gentamicin;
- Levomycetin;
- Vitabact.