The cornea is the front part of the shell of the eyeball, a transparent convex-concave lens. The average thickness of the cornea is 530-540 microns. Some people are born with a thinner cornea than normal, while others experience thinner corneas due to disease or environmental factors.
- Congenital thin cornea
- Acquired thin cornea
- Symptoms accompanying corneal thinning
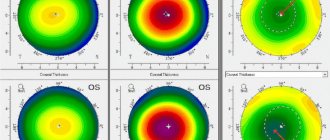
- Diagnostics
- Interpretation of corneal thickness values
- Surgeries for thin corneas Difficulties and limitations
- Modern gentle methods of laser correction
- Implantation of PIOL: when laser correction is impossible
The cornea is the front part of the shell of the eyeball, a transparent convex-concave lens. The average thickness of the cornea is 530-540 microns. Some people are born with a thinner cornea than normal, while others experience thinner corneas due to disease or environmental factors.
There is no generally accepted gradation of corneal thickness; only conditionally the thickness of the cornea can be represented as follows:
- ultra-thick – from 600 microns;
- thick – 561-600 microns;
- normal – 520-560 microns;
- thin – 481-520 microns;
- ultra-thin – less than 480 microns.
The concept of “thin cornea” is not inherently a diagnosis. When it is mentioned, a careful differential approach is always required to decipher what exactly the doctor meant.
Causes
The main cause of corneal layer degeneration is considered to be heredity. When a thin cornea is diagnosed in one or both parents, the probability of the child having such a pathology ranges from 20% to 50%.
Additionally, the following external factors can affect the thickness of the cornea:
- severe form of myopia;
- the influence of negative environmental factors on the eyes;
- diagnosing a patient with Down syndrome;
- exposure to high intraocular pressure, which provokes the development of keratoconus;
- regular long-term exposure to ultraviolet rays on the eyes.
Under the influence of the environment, not only the corneal layer thins, but its shape also changes.
Possible clouding of the cornea. Also, with this pathology, astigmatism or sympathy may develop, which necessarily affects the quality of vision. All this increases the possible risk of corneal rupture and can cause complete loss of vision.
Structure and functions of the cornea of the eye
In shape, the cornea is the transparent part of the ball, most of which (about five-sixths) is the sclera - the white opaque membrane of the eye. The cornea is the main refractive lens of our visual system.
The cornea itself is a transparent, avascular tissue with a strictly ordered fiber structure and a certain amount of water. Normally, corneal tissue is highly sensitive, transparent, shiny and smooth.
The cornea consists of five layers:
- The first is epithelial. It is a flat, multilayered, non-keratinizing cell tissue; Basically, this layer performs a protective function and quickly recovers when damaged; the epithelium also supplies the cornea with oxygen and regulates the flow of fluid into its internal layers
- The second is Bowman's shell. This is a layer that participates in the nutrition of the cornea and is more sensitive, as a result of which it is susceptible to damage, after which it is not restored
- The third layer is the stroma. This is the corneal tissue that makes up the largest part of the cornea (about 90% of its total thickness); this layer consists of collagen fibers and cells responsible for regeneration.
- The fourth is Descemet's membrane. This is the layer that separates the stroma from the endothelium; Descemet's membrane consists of a network of thin collagen fibers and serves as a barrier to prevent infections from entering the eyes
- The fifth layer is the endothelium. This is a layer of cells responsible for nourishing the cornea and regulating the amount of moisture it contains; the endothelium also prevents the formation of corneal edema under the influence of intraocular pressure.
The process of nutrition of the cornea occurs as a result of the work of blood vessels, nerves, as well as due to the presence of the tear film and moisture of the anterior chamber.
The main function of the cornea, in addition to optical, is protective. This part of the eye is the first to be negatively affected by the environment. Any, even the slightest irritation of the surface of the cornea, causes an unconditioned reflex in a person - closing the eyelids and increased lacrimation. The secreted tears instantly wash away small foreign particles or chemicals from the surface of the eyeball, and also protect the eye structures from damage.
Risk group
The most susceptible to corneal dystrophy are people with vision problems such as astigmatism, myopia or farsightedness. It is also possible that the problem may develop when working in dusty rooms, which may lead to other eye problems. Sunbathing enthusiasts and people working with objects that emit ultraviolet light should pay more attention to eye care. The risk group also includes patients with high intraocular pressure and developed ocular keratoconus.
Risks and complications
The most common complication of radial keratotomy is the development of reverse astigmatism. In addition, fibroplasia of postoperative scars can cause discomfort in the eyes or pathologies of refraction. Performing a radial keratotomy can also provoke a hypermetropic shift, which occurs due to the formation of holes in the cornea due to the excessive number, great depth and length of the incisions made. For patients with radial keratotomy, if age-related cataracts occur in the future, it may be difficult to select an intraocular lens.
Another complication of surgical intervention is a decrease in the density of corneal endothelial cells, which can cause its thinning. Degenerative-dystrophic changes in the cornea in the postoperative period are rare, and even more rarely, iridodialysis develops. Very rarely, corneal perforation and traumatic rupture of the keratotomy scar may occur after surgery.
Thus, numerous serious complications of radial keratotomy, as well as the inability to predict the outcome of the operation, have made this method practically unclaimed today. The operation is performed only in rare cases, for special indications, when laser vision correction, which is widely used today, is not possible.
Symptoms
Depending on the type of thinning, corneal dystrophy can manifest itself with different symptoms. In one case, the pathology may not manifest itself at all. For others, the cornea immediately becomes clouded as materials accumulate in the cornea, causing loss or deterioration of visual function.
Most patients experience corneal erosion. In this case, detachment of the outer corneal layer from Bowman's membrane is observed. In the presence of erosions, the following symptoms may appear:
- pain in the eyes with varying intensity from mild to unbearable;
- increased sensitivity of the eyes to light;
- feeling of foreign bodies in the eyes.
Clinical picture
The difference between fresh inflammatory opacification and a corneal scar: the absence of corneal syndrome, clear boundaries of the opacification.
With fresh inflammation, the corneal syndrome is pronounced, the boundaries are blurry, the surface of the turbidity is rough, the cut of the corneal lesion is thickened. The development of connective tissue scars is the outcome of almost all keratitis.
With peripheral scars, unlike central ones, vision is not affected. According to the degree of intensity: a weak cloudiness is a “cloud”, a more intense one is a “spot”, an intense scar is a thorn. When an ulcer of the cornea is perforated, fluid flows out of the anterior chamber, and the iris may fall out or attach to the posterior surface of the cornea. Subsequently, a cataract is formed, fused with the iris. This complication, in addition to a sharp decrease in vision, can lead to secondary glaucoma or the formation of corneal staphyloma. Staphyloma develops due to stretching of the corneal scar fused with the iris. Turbidity with ingrowth of limbal vessels (superficial and deep) or non-vascular.
Corneal opacities as a result of copper deposition along the limbus (Kayser-Fleischer ring), signs of Wilson-Konovalov disease. Deposition of dermatan-, keratan-, and heparan sulfates occurs in patients with mucopolysaccharidoses. Iron deposits in the form of a line in the lower third of the cornea may be age-related.
| Ingrowth of superficial vessels |
Diagnostics
To prevent corneal dystrophy, the problem should be identified in a timely manner. To do this, you should visit a specialist who will prescribe a number of procedures. Methods for diagnosing disorders of the corneal layer include:
- pachymetry – used to measure corneal thickness using ultrasound;
- refractometry - designed to identify vision problems that may contribute to corneal dystrophy;
- skiascopy - used to determine the ability of the eyes to refract light rays;
- ophthalmoscopy - used to examine the eyes through a slit lamp to assess the condition of the vascular system of the eyes, retina and optic nerves;
- biomicroscopy - intended to detect corneal opacities, cracks in the membrane and seals on the nerve endings;
- keratotopography – designed to study the corneal relief through a graphic image.
Symptoms and diagnosis
It is very difficult to determine the initial form of dystrophy, since it does not manifest itself in any way. If the pathology is genetic in nature, you need to bring the child at the age of 10 for a consultation with an ophthalmologist. The first symptoms may be as follows:
- redness of the eyes;
- irritation from bright light;
- feeling of “sand” in the eyes;
- blinking hurts;
- decreased quality of vision;
- Tears are constantly flowing.
If the listed symptoms appear, you should immediately consult an ophthalmologist. Diagnosis is carried out using a slit lamp, ultrasound pachymetry and other methods.
Diagnosis using a slit lamp is called biomicroscopy. The doctor determines the thickness of the cloudy layer and its features. With the help of ophthalmoscopy, fundus reflexes are determined, keratotopography reveals any pathologies using computer diagnostics. At the end of the examination, standard visometry is performed to determine visual acuity and its defects.
Treatment for thin corneas
Depending on the thinning of the cornea, different treatment methods may be prescribed for the disorder. If there is a slight change in thickness, conservative therapy is used using special corrective lenses. The structure of the CL is specially designed to prevent changes in the shape of the cornea, its stretching, dystrophy and ruptures.
To achieve this, the lens has soft sides and a hard center. To restore the cornea and eliminate discomfort, special eye drops, hormonal agents, vitamins and immunostimulating drugs are used. Magnetotherapy, phonophoresis and Sidorenko glasses are also used for treatment.
Treatment methods
Depending on the concomitant eye diseases, the optimal method of surgical correction is chosen, for example, implantation of an artificial lens.
Hereditary corneal dystrophy
The hereditary form of dystrophy is corrected with the help of vitamin preparations and instillation of vitamin-containing medicinal solutions. Sometimes a drug to improve soft tissue trophism can help. If vision is severely reduced, a corneal transplant or keratoplasty is performed.
However, the hereditary form of dystrophy cannot be completely cured, and even in the case of corneal transplantation, re-development of the pathology is possible. After a few years, patients again show signs of thinning of the stratum corneum. Repeated transplantation can significantly improve the condition of the visual organ; as a rule, patients manage to restore vision.
Edema dystrophy
At the initial stage of pathology progression, the installation of glycerin and glucose, vitamin therapy and correction of soft tissue trophism help. Swelling of the epithelial layers of the cornea is treated with antibiotics, antibacterial ointments and drugs to accelerate tissue regeneration. In some cases, laser stimulation of the cornea gives positive results. In case of severe swelling and thickening of the cornea, penetrating subtotal keratoplasty is performed.
Band-shaped dystrophy
If vision is completely lost, the diseased organ is completely removed and an artificial eye is implanted. Typically, the ribbon-like form of corneal degeneration is formed due to injury or the development of glaucoma. If vision is partially preserved, the clouded layers of the cornea are cut off (keratectomy). Subsequently, the patient is prescribed drugs to activate epithelial restoration and tissue regeneration.
Endothelial epithelial corneal dystrophy
Unfortunately, no cure for this pathology has been found. Surgery can only slow down the rapid development of dystrophy and delay the onset of blindness. Additional measures to the main surgical treatment are physical procedures - helium-neon laser stimulation and magnetic therapy.
Donor tissue transplantation is used to replace cloudy layers of the cornea. However, all types of surgical correction have side effects—various types of complications. Therefore, in modern ophthalmology, cryokeratoplasty is used, a more gentle method of correcting the corneal layer.
Crosslinking
This minimally invasive treatment method involves photopolymerization of the corneal connective protein collagen. It is used for any form of dystrophic change in the epithelium. The operation does not require hospital conditions. The diseased eye is anesthetized using drip anesthesia, then the corneal layer is saturated with riboflavin and irradiated with ultraviolet light. The eye is closed with a contact lens and sent home. At home, the patient is required to keep the lenses clean and adhere to the treatment regimen determined by the ophthalmologist.
Laser vision correction for thin corneas
The thickness of the cornea for laser correction is one of the main values, since with such correction the layers are thinned so that the light rays are focused precisely on the retina. The layer that will need to be cut off will depend on the degree of violation. Therefore, before prescribing laser correction, the thickness of the corneal layers is assessed.
Laser vision correction occurs by thinning the layers of the cornea using a laser beam. Achieving results and the risk of developing possible complications will directly depend on the residual thickness of the cornea at the end of the operation.
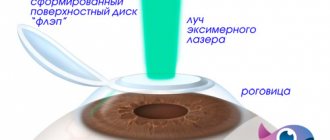
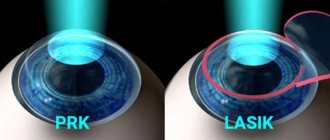
LASIK
The difference between this method and other laser operations is that the top layer of the cornea is not removed, but only partially cut off and finally returned back. It should be taken into account that the upper layers have a jelly structure and are not able to retain their shape, so there is a need to cut off the stroma, which has a denser structure.
Recovery after LASIK is faster, but the thickness of the stroma decreases, which is why it is prohibited to remove a thick lens in the stroma in the future. Based on this, it is clear why it is prohibited to use this correction method when the cornea is thinning.
Femto lasik
The operation is based on the technology of cutting flaps of the upper layers of the cornea with a laser and partially evaporating the lower layers. The effect of femto lasik depends on the residual thickness. Surgery on thin corneas is performed using non-contact femtosecond laser beams. In this case, the upper part of the cornea is grafted using a seamless method.
Femto eraser helps to form a smooth surface of the cornea without any mechanical intervention in the structure of the eye. Thin cornea surgery helps correct vision regardless of the complexity of the disorder. It is prohibited to use the method only in cases of severe myopia.
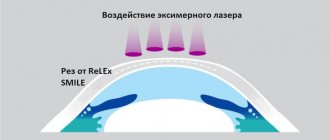
Laser correction SMILE
The new SMILE laser operation allows the laser to be used on the thinnest possible cornea, since there is no longer any need to cut off the thickness. Using a microscopic puncture, a small hole is made through which the flap is removed. This operation allows you to correct vision up to -13.5 diopters, while other technologies can only change -6 diopters. Laser correction allows you to correct vision defects without affecting the function of the cornea.
It must be remembered that thinning of the cornea can be caused by various reasons. And often with such a violation it is prohibited to carry out operations. Only a specialist can choose the correct correction method; he also determines the need for such intervention.
Photorefractive keratectomy
It refers to fairly old operating methods, since the practice of performing the operation is more than 30 years old. During the operation, the corneal epithelium is removed and then the required number of layers of the cornea is evaporated with a laser.
Treatment and correction
Treatment and correction methods for thin corneas are selected taking into account not only the thickness of the cornea, but also the characteristics of concomitant diseases (keratoconus, keratoglobus, astigmatism, etc.).
Contact lenses
Contact lenses, like the lenses used to make glasses, are optical media that refract light and direct it to the inner layer of the eye, covered with photoreceptors, the retina. They are used to correct refractive errors with mild to moderate thinning of the cornea and are worn directly on the cornea of the eye.
An ophthalmologist should select lenses for vision correction, since it is necessary to take into account not only the material of the product, but also other clinically important characteristics: radius of curvature (especially important for patients with keratoconus), optical power, cylinder axes, lens diameter, thickness of the central optical parts, etc.
Lenses must have an optimal contact area with the cornea, stable fixation on the surface of the eye and a suitable degree of correction
To correct refractive errors with a thin cornea, it is optimal to use rigid orthokeratological gas permeable lenses, which should be worn only at night (15-20 minutes before bedtime). Such lenses have the maximum corrective effect, but are not suitable for all patients due to the too rigid rim part. For such patients, scleral or double-layer lenses, consisting of a soft and a hard part, are an acceptable option.
Which lenses are suitable for correcting refractive errors with thin corneas?
Important! Lenses made of soft material, although they provide a comfortable fit and fairly reliable fixation, making them suitable for a large number of patients, are inferior in effectiveness to hard orthokeratological lenses. The use of soft lenses is only possible at the expense of the effect of refractive correction.
Corneal Collagen Crosslinking
CornealCollagenCrosslinking (CCL) is a modern, but still little-studied method that allows you to stop the progression of dystrophic changes and further destruction of the cornea of the eye, obtain higher visual acuity, normalize the uniform curvature of the central part of the cornea and temporarily postpone the need for surgical treatment (cornea transplant).
The essence of the method is the instillation of vitamin B2 followed by irradiation with ultraviolet rays, the duration of which is 20-30 minutes. As a result of ultraviolet heating, collagen filaments are heated, which naturally stimulates neocollagenesis (synthesis of new elastin) and increases the strength of the fibrillar basis of the corneal stroma. Vitamin B2 is a coenzyme of many biochemical processes, in particular, redox reactions and the breakdown of foreign D-isomers formed as a result of the activity of the bacterial flora of the eye.
Despite little practical experience, the corneal collagen crosslinking technique has already shown positive results, so it is increasingly used for the conservative treatment of corneal pathologies, especially corneal dystrophy of the keratoconus type.
Penetrating keratoplasty
Penetrating keratoplasty is a corneal transplant surgery. The indication for its implementation is an extreme degree of thinning of the cornea (especially if it is accompanied by scarring), in which restoration of normal refraction by other methods is impossible due to high risks.
The operation is performed under general anesthesia, and a donor implant is installed in place of the thinned and deformed area of the cornea. Despite the extremely low probability of rejection due to the lack of blood vessels in the cornea, local anti-inflammatory therapy with glucocorticoids (prednisolone, hydrocortisone) is carried out after surgery. To prevent secondary infection of injured tissues, antibiotic instillations (levofloxacin) are prescribed.
The sutures are removed several months after the corneal transplant.
Important! Penetrating keratoplasty in itself is not a complex ophthalmological operation, but after it it is necessary to observe a gentle motor regimen. For 2 years from the date of corneal transplantation, it is prohibited to engage in diving, active sports, lift heavy objects, or be exposed to strong shaking. After transplantation of a donor cornea, children and adolescents are exempt from physical education for 1.5-2 years.
Partial keratoplasty
Partial keratoplasty is a more complex surgical procedure compared to the penetrating transplantation technique, so it is used much less frequently. The difference is that with partial keratoplasty (epiceratophakia), the surgeon first removes the thinned corneal epithelium, and then implants a donor site in its place.
The healing period after such an intervention is longer and more difficult. Therefore, specialists in most cases prefer penetrating keratoplasty.